Introduction
Coronary Artery Disease (CAD) is a condition in which atherosclerotic plaque builds up within the wall of the coronary arteries leading to narrowing and the clinical manifestations of acute coronary syndrome [1]. It is one of the most common causes of mortality and morbidity in both developed and developing countries. It is also predicted to be the most common cause of death globally, including India, by 2020 [2,3]. The occurrence, morbidity and mortality from CAD among Asian Indians have been reported to be elevated among Europeans, Americans and other Asians, irrespective of whether they live in India or abroad [4]. The CAD rates in large Indian cities are reported as high or higher than that of Indians living overseas [5–7].
The occurrence of CAD has gradually increased in India during the latter half of the last century, predominantly among the urban population [8]. The predictable risk factors, namely hypertension, Diabetes Mellitus (DM), hypertriglyceridaemia, low levels of high-density lipoprotein cholesterol (HDL-C), central obesity, high low-density lipoprotein) cholesterol (LDL-C), low levels of antioxidants (vitamin A, E, beta-carotene), escalating affluence, rapid modernization associated with sedentary but stressful lifestyle in summation are suggested as additional risk factors for CAD [9].
Hepatic Lipase (HL) is an enzyme synthesized and secreted into the Disse space where it binds to the surface of sinusoidal endothelial cells and the external surface of microvilli of parenchymal cells [10]. It catalyzes the hydrolysis of triglycerides and phospholipids from plasma lipoproteins, contributing to the remodelling of Very Low- Density Lipoprotein (VLDL) remnants, LDL and HDL [11,12]. Independently of its lipolytic function, HL also plays a role in the hepatic uptake of remnants, HDL and LDL particles. Low HL activity has been related to high HDL concentration and more buoyant, less atherogenic LDL particles, but also to hypertriglyceridemia and the accumulation of remnant lipoproteins [13].
The human hepatic lipase (LIPC) gene encodes HL, an enzyme involved in lipoprotein metabolism and regulation [14]. Therefore, variants in LIPC gene may influence plasma lipoprotein levels. It is found to be on chromosome 15q21 and consist of nine exons and eight introns, covers over up 30 kb of DNA and encodes a protein with 449 amino acids [15,16]. The four common SNPs in the promoter region, consist of four extremely associated polymorphism in the 5’-Flanking region of the LIPC gene (-250 G/A,-514C/T,-710T/C and -763A/G) with respect to the transcription star site, which are in complete linkage disequilibrium, have been identified [17,18]. A substitution in the promoter region of the LIPC gene (-250G/A) has been reported to be related to modifications of plasma lipid levels [19–26] and the risk of CAD [27,28]. The association between hepatic lipase and CAD has been controversial [29]. The inverse relationship between HL activity and plasma HDL-C [30], a well known protective factor against CAD and the positive association of HL with small dense LDL-C [31], a possible risk factor of CAD, have pointed towards the pro-atherogenic role of HL [32]. However, reports that patients with the HL deficiency developed premature CAD [33].
The A allele of G-250A SNP are associated with lower HL activity and higher HDL levels in healthy subjects [29,34–38]. The distribution and clinical significance of G-250A polymorphisms have been extensively investigated among the Europeans, Asians and Americans, while they are still widely unknown among Indians [39–47]. Therefore, in this study, we plan to investigate the HL promoter -250G/A gene polymorphisms and risk of CAD in North Indian population.
Materials and Methods
This was a population based case control study conducted in the Department of Physiology and Cardiology at King George’s Medical University, Uttar Pradesh, Lucknow, India. Total 477 subjects (n=233 cases and n=244 control subjects) between the age group of 40 to 70 years were enrolled in the study on the basis of well defined inclusion and exclusion criteria. The sample size was statistically calculated with 80% of power [48]. The study group was recruited from the Intensive Care Unit (ICU) of Department of Cardiology, King George’s Medical University, Uttar Pradesh, Lucknow, a tertiary care hospital in India, between March 2011 and September 2014.
Controls were recruited from teaching/non-teaching staff of the institute as well as from other OPDs of our institute. Subjects having a previous history of medication, endocrinological disorder, pregnancy, chronic diseases, infection, gynaecological problem, were excluded. The diagnosis of CAD was defined as 50% stenosis in any major coronary artery, as revealed by coronary angiography [49]. On the basis of angiography results, patients were classified into two groups: with and without CAD. The study was approved by the ethical committee of King George’s Medical University, Lucknow. Written informed consent for the participation in the study was obtained prior to enrollment from all the subjects. “We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research”. This study was conducted under the principles of the Declaration of Helsinki [50].
Anthropometric Parameters
All subjects were evaluated, for Waist to Hip Ratio (WHR), waist circumference (WC); was measured at the narrowest point superior to the hip and was divided by the circumference of the hip measured at its greatest gluteal protuberance, height (Ht), weight (Wt), Blood Pressure (BP), and Pulse Rate (PR) and Body Mass Index (BMI); calculated as weight (in kilograms) divided by height (in meters) squared [51].
Biochemical Parameters
A 5 ml of venous blood samples were collected from all subjects and controls after 12 hours fasting. Blood samples were centrifuged at 5000 rpm for 15 min and plasma/serum was separated and stored at -20°C until being assayed further. Estimation of plasma glucose was done by GOD-POD method (Randox Laboratories Ltd., Antrim, UK). Lipid profile concentrations (TG: triglyceride, TC: total cholesterol and HDL: high density lipoprotein) were done by enzymatic method (Randox Laboratories Ltd., Antrim, UK). Low density lipoprotein (LDL) and very low density lipoprotein (VLDL) were calculated by Friedewald equation [52].
Genotyping of LIPC -250 G/A gene polymorphism
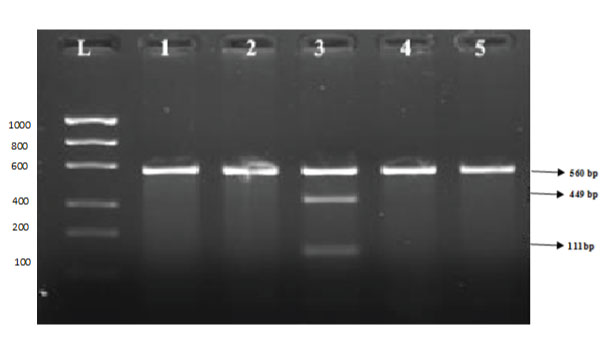
The genomic DNA was extracted from peripheral blood lymphocytes by salting out method [53]. The genotyping was performed using Polymerase Chain Reaction–Restriction Fragment Length Polymorphism (PCR-RFLP) technique. To improve the genotyping quality and validation, all variants and heterozygous samples were re-genotyped and the results were noted only for those samples which were reproducible and with no discrepancy. The transition polymorphism G to A of (LIPC-250) polymorphic site was amplified by the polymerase chain reaction (PCR). The amplification was performed using 5’-CCTACCCCGACCTTTGGCAG-3’ and 5’-GGGGTCCAGGCTTTCTTGG-3’ (Zambon A et al., 1998) as forward and reverse primer pair, respectively. The reaction was carried out in a final volume of 25 μl containing 3 mmol/l MgCl2, 0.5 mmol of each dNTP (Bangalore GeNie), 0.2 μmol of each primer, and 2.5 U of taq DNA polymerase (Bangalore GeNie). DNA was amplified with cycling conditions of 95°C for 4 min, 95°C for 45 sec, 60°C for 45 sec, 72°C for 45 sec and for 30 cycles with final extension of 7 min at 72°C. The 560bp amplicon was digested with Dral restriction enzyme (Fermantas) to identify the G and A allele. The digested PCR product was analysed by gel electrophoresis using 2% agarose gel. G/A heterozygote mutant genotype shows three bands of 560 bp, 449 bp and 111 bp and G/ G homozygote wild genotype shows one band of 560 bp [Table/Fig-1].
Restriction Fragment Length Polymorphism Analysis of LIPC-250G/A (rs2070895) gene: L: 100 bp DNA molecular weight marker, Lane1,2,4 and 5 G/G Homozygous wild, Lane 3 G/A Heterozygous mutant.
Statistical Analysis
Statistical analysis was carried out using the INSTAT 3.0 (Graph Pad Software, San Diego, CA). Quantitative variables are presented as the mean ± standard deviation. Comparisons of continuous data between two independent groups were done by Student’s unpaired t-test. Minitab version 15.0 was used for univariate to assess the association with each variable in turn and then with adjustment for other significant associations in coronary artery disease. All statistical tests were two-tailed, and p < 0.05 was chosen as the level of significance. The 2 test was used to perform the analysis of the association of the polymorphism with CAD and categorical features. Allelic and genotypic frequencies were estimated by genotype count. Hardy–Weinberg equilibrium assumptions were assessed by comparing the observed and expected numbers of genotypes. The association between genotypes and clinical characteristics was expressed as Odds Ratio (OR) with 95% confidence interval (95% CI).
Results
Anthropometric and Biochemical Characteristics of the Studied Subjects
The demographic and biochemical features of the study and control groups are presented in [Table/Fig-2]. Among the 477 participants, 233 patients had angiographically proven CAD and 244 had normal coronary arteries (without CAD). The CAD cases had significantly higher fasting blood sugar (FBS) (p = <0.0001), BMI (p =<0.0001) systolic blood pressure (p= <0.0001), diastolic blood pressure (p= 0.046), total cholesterol (p = <0.0001), TG (P = 0.0001), LDL-C (p <0.0001), and lower HDL-C (p= < 0.0001) than controls. For the demographic data the Weight (p= <0.0001), Waist Circumference (p = <0.0001) and Waist to Hip Ratio (p = <0.0001) were significantly higher in CAD cases as compare to controls. An elevated level of LDL-C, TG and lower level of HDL-C have been considered to increase the risk of CAD.
Anthropometric and biochemical characteristics among study and control groups.
| Parameters | Cases (n=233) | Controls (n=244) | p-value |
|---|
| Age (yr) | 56.15±8.13 | 55.10±7.10 | 0.1332 |
| Weight (kg) | 71.63±11.50 | 59.85±12.33 | <0.0001* |
| Height (cm) | 159.71±8.37 | 159.11±8.29 | 0.44 |
| BMI (kg/m2) | 27.60±5.82 | 24.23±4.366 | <0.0001* |
| WC (cm) | 95.96±11.53 | 83.60±9.24 | <0.0001* |
| WHR | 0.97±0.16 | 0.91±0.08 | <0.0001* |
| SBP (mmHg) | 133.67±15.25 | 121.13±9.92 | <0.0001* |
| DBP (mmHg) | 90.81±13.45 | 80.35±7.07 | 0.046* |
| FBS (mg/dl) | 121.41±32.21 | 93.213±18.78 | <0.0001* |
| TC (mg/dl) | 185.33±36.34 | 164.37±44.08 | <0.0001* |
| TG (mg/dl) | 168.27±78.33 | 115.73±56.36 | <0.0001* |
| HDL-C (mg/dl) | 34.21±9.06 | 45.09±16.20 | <0.0001* |
| LDL (mg/dl) | 113.02±41.28 | 93.96±35.88 | <0.0001* |
| VLDL (mg/dl) | 35.56±27.80 | 21.58±9.84 | <0.0001* |
*Data are expressed in mean ± SD; Significant p-value <0.05.
Study Group = subjects with coronary artery disease, Control Group = subjects without coronary artery disease; SBP: Systolic Blood Pressure; DBP- diastolic Blood Pressure; WC: Waist Circumference; WHR: Waist to Hip Ratio; BMI: Body Mass Index; FBS: Fasting Blood Sugar; TC: Total Cholesterol; TG-Triglyceride; VLDL- Very Low Density Lipoprotein; HDL- High Density Lipoprotein; LDL- Low Density Lipoprotein. mmHg: Millimeters of mercury
The Genotype and Allele Frequencies of –250G/A Polymorphism in Hepatic Lipase gene
The allele frequencies were G (wild type): 88.42% vs. 94.67% and A (mutant type): 11.58% vs. 5.33% in with and without coronary artery disease. The frequencies of LIPC genotypes and alleles were compared between with and without coronary artery disease subjects [Table/Fig-3]. In all genetic models (co-dominant, dominant and recessive) LIPC-250G/A gene had a strong association with coronary artery disease. The genotype distribution of LIPC-250G/A deviates significantly. [Table/Fig-2] shows the distribution of genotype and allele frequencies of the case and control groups for LIPC-250G/A genotypes. In LIPC-250G/A genotype, the frequencies of GG, GA and AA genotype in CAD group was 80.69%, 15.45% and 3.86%, respectively; in the control group, the corresponding frequencies were 90.16%, 9.02% and 0.82%, respectively. Significant difference was found in the genotype (LIPC-250G/A) distribution between the two groups. Further logistic regression analysis indicated that the GA and AA genotypes in SNP -250G/A were significantly associated with CAD in all genetic models (In co-dominant model- GA vs. GG, OR=1.91, 95% CI=1.09-3.37, p=0.03 and AA vs. GG, OR= 5.26, 95% CI= 1.10-24.60, p=0.04; in dominant model- GA+AA vs GG, OR=2.19, p=0.004 and in recessive model- AA vs GG+GA, OR=5.26, p=0.04 whereas, A allele at nucleotide −250G/A in the LIPC gene had an association with increased risk of CAD (OR=2.33, p=<0.0008).
Genotype and allele frequency distribution of Hepatic lipase gene (LIPC)-250G/A polymorphism among study and control group.
| Model | Genotype250 G/A | Case n (%)n=233 | Control n (%)n=244 | χ2 | p-value | OR (95% CI) | p-value |
|---|
| Codominant | GG | 188 (80.69) | 220 (90.16) | | | 1.00 | - |
| GA | 36 (15.45) | 22 (9.02) | | | 1.91 (1.09-3.37) | 0.03 |
| AA | 9 (3.86) | 02 (0.82) | 10.095 | 0.006 | 5.26 (1.10-24.60) | 0.04 |
| Dominant | GG | 188 (80.69) | 220 (90.16) | | | 1.00 | - |
| GA+AA | 45 (19.31) | 24 (9.84) | 8.652 | 0.003 | 2.19(1.29-3.74) | 0.004* |
| Recessive | GG+GA | 224 (96.14) | 242 (99.18) | | | 1.00 | - |
| AA | 9 (3.86) | 02 (0.82) | 4.899 | 0.026 | 5.26 (1.10-24.60) | 0.04* |
| Allele | G | 412 (88.42) | 462 (94.67) | | | 1.00 | - |
| A | 54 (11.58) | 26 (5.33) | 12.160 | 0.0005 | 2.33 (1.43-3.79) | 0.0008* |
1Binary logistic regression, OR = age and gender matched odds ratio, 95% CI = 95% confidence interval, for risk analysis assuming strong associations with disease outcome (OR = 1)*A value of p<0.05 was considered statistically significant.
Genotype distribution of –250G/A polymorphism according to anthropometric and biochemical parameters in study population
Comparison of anthropometrical and biochemical characteristics of the cases and controls according to the LIPC-250 genotype among non-carriers (GG) and carriers (GA+AA) of LIPC -514C/T promoter gene polymorphism with and without CAD are summarized in [Table/Fig-4]. In our study, we could not find the significant association between LIPC-250 G/A gene polymorphism and anthropometrical as well as biochemical characteristics among cases and controls. Only WHR was significantly (0.0001) different between LIPC genotypes among the cases. There was a significant association between LIPC-250 G/A gene polymorphism and its circulating serum level.
Comparison of anthropometric and biochemical circulating level among carriers and non-carriers of LIPC-250 G/A mutant allele (A) in study and control group.
| variables | LIPC-250 G/A (Case) n=233 | LIPC-250 G/A (Control) n=244 |
|---|
| GG | GA+AA | p-value | GG | GA+AA | p-value |
|---|
| Age (yr) | 56.11±8.19 | 56.26±7.97 | 0.91 | 56.31±8.04 | 53.04±7.01 | 0.05 |
| Weight (kg) | 71.59±11.42 | 71.80±11.94 | 0.91 | 59.54±12.29 | 62.67±12.60 | 0.23 |
| Height (cm) | 159.84±8.73 | 159.13±9.49 | 0.63 | 158.92±8.43 | 160.83±6.64 | 0.24 |
| BMI (kg/m2) | 27.62±5.77 | 27.52±6.09 | 0.91 | 24.14±4.37 | 25.00±4.34 | 0.36 |
| WC (cm) | 95.79±11.67 | 96.64±11.02 | 0.65 | 83.28±9.15 | 86.50±9.73 | 0.10 |
| HC(cm) | 91.31±10.30 | 101.33±11.14 | 0.0001* | 91.35±7.33 | 87.50±9.44 | 0.01* |
| WHR | 0.97±0.17 | 0.95±0.10 | 0.44 | 0.87±0.21 | 0.91±0.11 | 0.35 |
| SBP (mmHg) | 133.67±16.21 | 133.68±10.47 | 0.99 | 121.40±9.85 | 118.75±10.40 | 0.21 |
| DBP (mmHg) | 90.10±13.16 | 93.80±14.35 | 0.09 | 80.35±7.47 | 80.37±8.40 | 0.99 |
| FPG (mg/dl) | 119.10±29.84 | 131.08±39.08 | 0.02* | 93.44±18.92 | 91.05±8.54 | 0.54 |
| TC (mg/dl) | 183.99±37.47 | 190.91±34.49 | 0.25 | 165.20±44.61 | 156.73±38.80 | 0.37 |
| TG (mg/dl) | 165.43±75.66 | 180.16±88.21 | 0.25 | 117.40±57.99 | 100.35±35.55 | 0.15 |
| HDL(mg/dl) | 34.30±8.70 | 33.80±10.52 | 0.74 | 45.25±16.74 | 43.68±10.11 | 0.65 |
| LDL (mg/dl) | 113.36±41.36 | 111.60±41.41 | 0.79 | 94.05±36.33 | 93.17±32.08 | 0.90 |
| VLDL (mg/dl) | 35.48±29.19 | 35.86±21.33 | 0.93 | 21.43±10.11 | 23.00±6.99 | 0.45 |
*p-value1 Comparison of cases with controls, *Significant (ANOVA)
SBP: Systolic Blood Pressure; DBP- diastolic Blood Pressure; WC: Waist Circumference; WHR: Waist to Hip Ratio; BMI: Body Mass Index; FBS: Fasting Blood Sugar; TC: Total Cholesterol; TG-Triglyceride; VLDL- Very Low Density Lipoprotein; HDL- High Density Lipoprotein; LDL- Low Density Lipoprotein. mmHg: Millimeters of mercury
Discussion
India is predicted to bear the greatest CAD burden, according to the estimates from the Global Burden of Disease Study [54]. A matter of serious concern is that 52% of the CAD deaths in India occurred in people aged below 70 years, while the same was just 22% in developed countries [55,56]. Reports on CAD in Indians from different parts of the world have shown that Asian Indians are at 3-4 times higher risk of CAD than white Americans, 6 times higher than Chinese, and 20 times higher than Japanese [57–60].
In the present study, we are reporting the association of LIPC promoter gene polymorphism, lipoprotein levels and coronary artery disease among the North Indian population. In our study, we observed 233 CAD and 244 without CAD, in which 286 male and 191 female were between age group of 40-70 years. Age is a powerful risk factor for coronary heart disease [61]. The development of atherosclerosis increases noticeably with age up to 65, regardless of sex and ethnic background [62,63]. According to the inherent study, the median age for developing CAD in the South Asian population is 53 years, whereas in western Europe, China & Hong Kong it is 63 years [64].
In the present study we reported significant difference in the distribution of allelic and genotype frequencies of LIPC gene (–250G/A) polymorphisms in between study and control group. We also found the significant association between polymorphisms and anthropometric parameters. This agreement supported by Pihlajamäki et al. However, Hegel et al., could not found such an association between the genetic variation in the promoter of LIPC gene and plasma lipoproteins in the Canadian population. Possibly it may be due to the differences in study populations, sample size and different ethnic group [65,66].
Ramachandran et al., reported the clustering of various cardiovascular risk factors in Asian Indians. Total serum cholesterol and LDL cholesterol are considered to be important risk factors for CAD in some studies and hyper triglyceridemia with low HDL is reported to be the major risk-factor in other studies [67]. In the present study, total cholesterol, LDL cholesterol and TG were found to be risk factors for CAD. It is well known that lower HDL-C levels could be one of the risk factors for premature CAD in Asian Indians [68]. The findings of our study were in agreement with these reports, as in our study the serum level of total cholesterol, triglyceride LDL and VLDL were found significantly higher in all study group, and high density lipoprotein was significantly lower in study group compared with control subjects. The inherent study showed that hypertension and diabetes were more important risk factors in younger Indian women than men. These studies indicate that abnormalities in lipid metabolism play an important role in development of CAD in young Indians [69].
In human, LIPC gene encodes HL enzyme that is involved in the metabolism and regulation of plasma lipoprotein with well-documented clinical importance of G-250A SNPs in LIPC gene the G-250A polymorphism has been found to be associated with type 2 diabetes, peripheral arterial disease and postprandial lipemic response [20,39,47,70,71]. This involvement has been reported in many populations including Austrians, Finnish, Spanish, and Turkish; however, it is less apparent in Japanese, Iranians, Chinese, Koreans, Americans, and Brazilians [14].
The findings of our study show that the -250G allele was more abundant among North Indian than -250A allele. The homozygous mutant allele (A) was singnificantly higher in the study group (p=0.0008), while homozygous wild allele (G) was higher in the control group(p=0.04). We also found that GA+AA genotype was significantly higher in study group (p=0.004). Here, we have evaluated that homozygous mutant were found at increased risk of CAD. Zambon et al., reported the allele frequency of the LIPC-250A polymorphism is 47% in a small group of Japanese Americans [34]. Another study De Andrade et al., was reported 32% allelic frequency of LIPC-250A polymorphism in Brazilian population. The findings of our study were agreement with these reports. These results indicate that the allelic variation of the LIPC -250G/A may have an ethnic specificity [27]. The distribution of this SNP is similar to that reported in Austrian, Spanish, Finnish, Turkish Brazilians and Americans, however, the -250 G/Allele is relatively less frequent in Japanese and Koreans [14]. This inconsistency may be due to the differences in genetic makeup of population, ethnic specificity and life style in our study population.
Epidemiological studies have suggested that both low HDL-C10 and the presence of small, dense LDL are associated with increased risk of CAD [31,72]. These lipid abnormalities often coexist in the same subject as part of a multifaceted phenotype referred to as an atherogenic lipoprotein profile [73]. In the current study, we showed that the FPG, TC, TG levels are significantly higher in GA + AA genotype and HDL-C level significantly higher in GG genotype of –250G/A polymorphism. This observation is in agreement with previous studies demonstrating an important role of HL activity as a major player in determining LDL size and density, and it provides further evidence for genetic regulation of LDL subclass distribution. A number of other factors have also been shown to affect HL activity in association with changes in LDL size and density, HDL2-C levels, and CAD risk [74]. In a study reported by Jimenez et al, there was no significant associations between the –250G/A polymorphism and plasma HDL-C levels [20].
Limitation
The variations in the lipid profile levels, may due to environmental factors, life style and physical activity. A study on larger sample size is needed to explore the biological pathways to underlying coronary artery disease and identify the functional variants.
Conclusion
On the basis of our findings, we concluded that higher frequency of heterozygous mutant genotype (G/A) and mutant allele A of LIPC-250G/A promoter gene polymorphism was significantly associated with the risk of CAD among the North Indians. The alteration of lipid levels was also a significant risk factor for CAD
[1]. Ebrahimi M, Kazemi-Bajestani SMR, Ghayour Mobarhan M, Ferns GAA, Coronary artery disease and its risk factors status in iran: a reviewIran Red Crescent Med J 2011 13(9):610-23. [Google Scholar]
[2]. Sekhri T, Kanwar RS, Wilfred R, Chugh P, Chhillar M, Aggarwal R, Prevalence of risk factors for coronary artery disease in an urban Indian populationBMJ Open 2014 4:e005346 [Google Scholar]
[3]. Padmanabhan S, Hastie C, Prabhakaran D, Dominczak AF, Genomic approaches to coronary artery diseaseIndian J Med Res 2010 132:567-78. [Google Scholar]
[4]. Enas EA, Kannan S, How to beat the heart disease epidemic among South Asians. A prevention and management guide for Asian Indians and their doctorsDowners grove: Advanced Lipid Clinic 2007 [Google Scholar]
[5]. Mohan V, Deepa R, Shantirani S, Premalatha G, Prevalence of coronary artery disease and its relationship to lipids in a selected population in South India. The Chennai urban population study (CUPS No.5)J Am Coll Cardiol 2001 38:682-87. [Google Scholar]
[6]. Reddy KS, India wakes upto the threat of cardiovascular diseaseJ Am Coll Cardiol 2007 50:1370-72. [Google Scholar]
[7]. Gupta R, Recent trends in coronary heart disease epidemiology in IndiaIndian Heart J 2008 60(2suppl-B):B4-18. [Google Scholar]
[8]. Gupta R, Epidemiological evolution and rise of coronary heart disease in IndiaSouth Asian J Preventive Cardiology 1997 1:14-20. [Google Scholar]
[9]. Rissam HS, Kishore S, Trehan N, Coronary artery disease in young indians –the missing link. journalIndian Academy of Clinical Medicine 2001 2(3):128-32. [Google Scholar]
[10]. Sanan DA, Fan J, Bensadoun A, Taylor JM, Hepatic lipase is abundant on both hepatocyte and endothelial cell surfaces in the liverJ Lipid Res 1997 38(5):1002-13. [Google Scholar]
[11]. Deeb SS, Zambon A, Carr MC, Ayyobi AF, Brunzell JD, Hepatic lipase and dyslipidemia: interactionsamong genetic variants, obesity, gender, and dietJ Lipid Res 2003 44:1279-86. [Google Scholar]
[12]. Zambon A, Bertocco S, Vitturi N, Polentarutti V, Vianello D, Crepaldi G, Relevance of hepatic lipase to the metabolism of triacylglycerol-rich lipoproteinsBiochem Soc Trans 2003 31:1070-74. [Google Scholar]
[13]. Lindi V, Schwab U, Louheranta A, Vessby B, Hermansen K, Tapsell L, The G-250A polymorphism in the hepatic lipase gene promoter is associated with changes in hepatic lipase activity and LDL cholesterol: The KANWU StudyNutrition, Metabolism & Cardiovascular Diseases 2008 18:88-95. [Google Scholar]
[14]. Khabour OF, Alomari MA, Alzoubi KH, Gharaibeh MY, Alhashimi FH, Lack of association between polymorphisms of hepatic lipase with lipid profile in young jordanian adultsLipid Insights 2014 7:1-5.doi:10.4137/LPI.S14798 [Google Scholar]
[15]. Cai SJ, Wong DM, Chen SH, Chan L, Structure of the human hepatic triglyceride lipase geneBiochemistry 1989 28:8966-71. [Google Scholar]
[16]. Ameis D, Stahnke G, Kobayashi J, McLean J, Lee G, Buscher M, Isolation and characterization of the human hepatic lipase geneJ Biol Chem 1990 265:6552-55. [Google Scholar]
[17]. Guerra R, Wang J, Grundy SM, Cohen JC, A hepatic lipase (LIPC) allele associated with high plasma concentrations of high density lipoprotein cholesterolProc Natl Acad Sci USA 1997 94:4532-37. [Google Scholar]
[18]. Murtomaki S, Tahvanainen E, Antikainen M, Tiret L, Nicaud V, Jansen H, Hepatic lipase gene polymorphisms influence plasma HDL levels. Results from Finnish EARS participants European Atherosclerosis Research StudyArterioscler Thromb Vasc Biol 1997 17:1879-74. [Google Scholar]
[19]. Bertolini S, Pisciotta L, Di Scala L, Langheim S, Bellocchio A, Masturzo P, Genetic polymorphisms affecting the phenotypic expression of familial hypercholesterolemiaAtherosclerosis 2004 174:57-65. [Google Scholar]
[20]. Jimenez-Gomez Y, Pérez-Jiménez F, Marín C, Gómez P, Moreno R, Delgado J, The -250G/A polymorphism in the hepatic lipase gene promoter influence the postprandial lipemic response in healthy menNutr Metab Cardiovasc Dis 2008 18:173-81. [Google Scholar]
[21]. Ko YL, Hsu LA, Hsu KH, Ko YH, Lee YS, The interactive effects of hepatic lipase gene promoter polymorphisms with sex and obesity on high density- lipoprotein cholesterol levels in Taiwanese-ChineseAtherosclerosis 2004 172:135-42. [Google Scholar]
[22]. Lindi V, Schwab U, Louheranta A, Vessby B, Hermansen K, Tapsell L, The G-250A polymorphism in the hepatic lipase gene promoter is associated with changes in hepatic lipase activity and LDL cholesterol: The KANWU StudyNutr Metab Cardiovasc Dis 2008 18:88-95. [Google Scholar]
[23]. Pihlajamaki J, Karjalainen L, Karhapaa P, Vauhkonen I, Taskinen MR, Deeb SS, G-250A substitution in promoter of hepatic lipase gene is associated with dyslipidemia and insulin resistance in healthy control subjects and in members of families with familial combined hyperlipidemiaArterioscler Thromb Vasc Biol 2000 20:1789-95. [Google Scholar]
[24]. Stancakova A, Baldaufova L, Javorsky M, Kozarova M, Salagovic J, Tkac I, Effect of gene polymorphisms on lipoprotein levels in patients with dyslipidemia of metabolic syndromePhysiol Res 2006 55:483-90. [Google Scholar]
[25]. Wood KC, Fullerton MD, El-Sohemy A, Bakovic M, Interactions between hepatic lipase and apolipoprotein E gene polymorphisms affect serum lipid profiles of healthy Canadian adultsAppl Physiol Nutr Metab 2008 33:761-68. [Google Scholar]
[26]. Zhao S, Xie X, Nie S, The -250G/A polymorphism in the human hepatic lipase gene promoter affects blood lipids in ChineseClin Chim Acta 2006 365:149-52. [Google Scholar]
[27]. De Andrade FM, Silveira FR, Arsand M, Antunes AL, Torres MR, Zago AJ, Association between -250G/A polymorphism of the hepatic lipase gene promoter and coronary artery disease and HDL-C levels in a Southern Brazilian populationClin Genet 2004 65:390-95. [Google Scholar]
[28]. Wei M, Lu YS, Li PP, Association of the hepatic lipase gene -250G/A promoter polymorphism with the susceptibility to type 2 diabetes mellitus combining with coronary heart diseaseZhonghua Yi Xue Yi Chuan Xue Za Zhi 2009 26:219-22. [Google Scholar]
[29]. Park KW, Choi JH, Chae IH, Cho HJ, Oh S, Kim HS, Hepatic lipase c514t polymorphism and its relationship withplasma hdl-c levels and coronary artery disease in koreansJ Biochem Mol Biol 2003 36(2):237-42. [Google Scholar]
[30]. Blades B, Vega GL, Grundy SM, Activities of lipoprotein lipase and hepatic triglyceride lipase in postheparin plasma of patients with low concentrations of HDL cholesterolArterioscler. Thromb 1993 13:1227-35. [Google Scholar]
[31]. Gordon DJ, Rifkind BM, High-density lipoprotein the clinical implications of recent studiesN Engl J Med 1989 321:1311-16. [Google Scholar]
[32]. Lamarche B, Tchernof A, Moorjani S, Cantin B, Dagenais GR, Lupien PJ, Small, dense lowdensity lipoprotein particles as a predictor of the risk of ischemic heart disease in men: prospective results from the Quebec Cardiovascular StudyCirculation 1997 95:69-75. [Google Scholar]
[33]. Breckenridge WC, Little JA, Alaupovic P, Wang CS, Kuksis A, Kakis G, Lipoprotein abnormalities associated with a familial deficiency of hepatic lipaseAtherosclerosis 1982 45:161-79. [Google Scholar]
[34]. Zambon A, Deeb SS, Hokanson JE, Brown BG, Brunzell JD, Common variants in the promoter of the hepatic lipase gene are associated with lower levels of hepatic lipase activity, buoyant LDL, and higher HDL2 cholesterolArterioscler Thromb Vasc Biol 1998 18(11):1723-29. [Google Scholar]
[35]. Tai ES, Corella D, Deurenberg-Yap M, Dietary fat interacts with the -514C.T polymorphism in the hepatic lipase gene promoter on plasma lipid profiles in a multiethnic Asian population: the 1998 Singapore National Health SurveyJ Nutr 2003 133(11):3399-408. [Google Scholar]
[36]. Deeb SS, Peng R, The C-514T polymorphism in the human hepatic lipase gene promoter diminishes its activityJ Lipid Res 2000 41(1):155-58. [Google Scholar]
[37]. Daneshpour MS, Hedayati M, Azizi F, Hepatic lipase C-514T polymorphism and its association with high-density lipoprotein cholesterol level in TehranEur J Cardiovasc Prev Rehabil 2006 13(1):101-03. [Google Scholar]
[38]. Isaacs A, Sayed-Tabatabaei FA, Njajou OT, Witteman JC, van Duijn CM, The -514 C-T hepatic lipase promoter region polymorphism and plasma lipids: a meta-analysisJ Clin Endocrinol Metab 2004 89(8):3858-63. [Google Scholar]
[39]. Valdivielso P, Ariza MJ, de laVega-Román C, Association of the -250G/A promoter polymorphism of the hepatic lipase gene with the risk of peripheral arterial disease in type 2 diabetic patientsJ Diabetes Complications 2008 22(4):273-77. [Google Scholar]
[40]. Gündoğdu F, Gurlertop Y, Pirim I, Association between -514C-T polymorphism of the hepatic lipase gene and coronary artery disease in a Turkish populationActa Cardiol 2008 63(2):197-202. [Google Scholar]
[41]. Ghatreh Samani K, Noori M, Nobar MR, Chaleshtory MH, Farrokhi E, Amin MD, The -514C/T polymorphism of hepatic lipase gene among Iranian patients with coronary heart diseaseIran J Public Health 2012 41(1):59-65. [Google Scholar]
[42]. Lahoz C, Peña R, Mostaza JM, The -514C/T polymorphism of the hepatic lipase gene significantly modulates the HDL-cholesterol response to statin treatmentAtherosclerosis 2005 182(1):129-34. [Google Scholar]
[43]. Riestra P, López-Simón L, Ortega H, Fat intake influences the effect of the hepatic lipase C-514T polymorphism on HDL-cholesterol levels in childrenExp Biol Med (Maywood) 2009 234(7):744-49. [Google Scholar]
[44]. Pulchinelli A Jr, Costa AM, de Carvalho CV, Positive association of the hepatic lipase gene polymorphism c.514C-T with estrogen replacement therapy responseLipids Health Dis 2011 10:197 [Google Scholar]
[45]. Wu J, Yin R, Lin W, Pan S, Yang D, Hepatic lipase gene -514C/T polymorphism in the Guangxi Hei Yi Zhuang and Han populationsLipids 2008 43(8):733-40. [Google Scholar]
[46]. Wang H, Jiang M, Qiu J, Quantitative assessment of the effect of hepatic lipase gene polymorphism on the risk of coronary heart diseaseArch Med Res 2010 41(5):383-90. [Google Scholar]
[47]. Ou L, Yao L, Guo Y, Fan S, Association of the G-250A promoter polymorphism in the hepatic lipase gene with the risk of type 2 diabetes mellitusAnn Endocrinol (Paris) 2013 74(1):45-48. [Google Scholar]
[48]. Jaykaran C, Tamoghna B, How to calculate sample size for different study designs in medical research?Indian J Psychol Med 2013 35(2):121-26. [Google Scholar]
[49]. Su G, Mi S, Tao H, Li Z, Yang H, Zheng H, Association of glycaemic variability and the presence and severity of coronary artery disease in patients with type 2 diabetesCardiovasc Diabetol 2011 10:19 [Google Scholar]
[50]. World Medical AssociationDeclaration of Helsinki Ethical Principles for Medical Research Involving Human SubjectsJAMA 2013 310(20):2191-94. [Google Scholar]
[51]. Anthropometric reference data for international use Recommendations from a World Health Organization Expert Committee de Onis M and Habicht JP AmericanJournal of Clinical Nutrition 1996 64:650-58. [Google Scholar]
[52]. Varley H, Gewenlock A, Bell M, Practical clinical biochemistry 1980 Vol.15th edLondonWilliams Heinemen Medical books, Ltd:741-897. [Google Scholar]
[53]. Miller SA, A simple salting out procedure for extracting DNA from human nucleated cellsNucleic Acids Res 1988 16:1215 [Google Scholar]
[54]. Murray CJ, Lopez AD, Alternative projections of mortality and disability by cause 1990e2020: Global Burden of Disease StudyLancet 1997 349:1498-504. [Google Scholar]
[55]. Reddy KS, Yusuf S, Emerging epidemic of cardiovascular disease in developing countriesCirculation 1998 97:596e601 [Google Scholar]
[56]. Bahl VK, Prabhakaran D, Karthikeyan G, Coronary artery disease in IndiansIndian Heart J 2001 53:e707-13. [Google Scholar]
[57]. Ghaffar A, Reddy KS, Singhi M, Burden of non-communicable diseases in South Asia (Rapid Response)BMJ 2004 328:807-10. [Google Scholar]
[58]. Enas EA, Garg A, Davidson MA, Coronary heart disease and its risk factors in the first generation immigrant Asian Indians to the United States of AmericaIndian Heart J 1996 48:343-54. [Google Scholar]
[59]. Gupta R, Epidemiological evolution and rise of coronary heart disease in IndiaSouth Asian J Prev Cardiol 1997 1:14-20. [Google Scholar]
[60]. Enas EA, Yusuf S, Third Meeting of the International working group on coronary artery disease in South AsiansIndian Heart J 1999 51:99-103. [Google Scholar]
[61]. Kumar S, Verma AK, Kumar N, Verma RK, Prevalence of coronary atherosclerosis in different age groups: a postmortem studyBiomedical Research 2013 24(1):139-41. [Google Scholar]
[62]. McGill HC Jr, McMahan CA, Malcom GT, Oalmann MC, Strong JP, Effects of serum lipoproteins and smoking on atherosclerosis in young men and women. The PDAY Research Group: Pathological Determinants of Atherosclerosis in YouthArterioscler Thromb Vasc Biol 1997 17:95-106. [Google Scholar]
[63]. Berenson GS, Srinivasan SR, Bao W, Newman WP, Tracy RE, Wattigney WA, Association between multiple cardiovascular risk factors and atherosclerosis in childrens and young adults.: The Bogalusa Heart StudyN Engl J Med 1998 338:1650-56. [Google Scholar]
[64]. Nagamalesh UM, Prakash VS, AV Hegde AV, Ambujam N, Cross-sectional observational survey evaluating myocardial infarction, risk profile and managementInternational Journal of Clinical Cases and Investigations 2014 5(5):69-77. [Google Scholar]
[65]. Pihlajamaki J, Karjalainen L, Karhapaa P, Vauhkonen I, Taskinen MR, Deeb SS, G-250A substitution in promoter of hepatic lipase gene is associated with dyslipidemia and insulin resistance in healthy control subjects and in members of families with familial combined hyperlipidemiaArterioscler Thromb Vasc Biol 2000 20:1789-95. [Google Scholar]
[66]. Hegele RA, Harris SB, Brunt JH, Young TK, Hanley AJ, Zinman B, Absence of association between genetic variation in the LIPC gene promoter and plasma lipoproteins in three Canadian populationsAtherosclerosis 1999 146:153-60. [Google Scholar]
[67]. Ramachandran A, Snehalatha C, Latha E, Clustering of cardiovascular factors in urban Asian IndiansDiabetes Care 1998 21:967-71. [Google Scholar]
[68]. Nag T, Ghosh A, Cardiovascular disease risk factors in Asian Indian population: A systematic reviewJournal of Cardiovascular Disease Research 2013 4:222-28. [Google Scholar]
[69]. Dave TH, Wasir HS, Prabhakaran D, Profile of coronary artery disease in Indian women: correlation of clinical, non-invasive and coronary angiographic findingsIndian Heart J 1991 43:25-29. [Google Scholar]
[70]. Todorova B, Kubaszek A, Pihlajamäki J, The G-250A promoter polymorphism of the hepatic lipase gene predicts the conversion from impaired glucose tolerance to type 2 diabetes mellitus: the Finnish Diabetes Prevention StudyJ Clin Endocrinol Metab 2004 89(5):2019-23. [Google Scholar]
[71]. Eller P, Schgoer W, Mueller T, Hepatic lipase polymorphism and increased risk of peripheral arterial diseaseJ Intern Med 2005 258(4):344-48. [Google Scholar]
[72]. Miller GJ, Miller NE, Plasma high-density-lipoprotein concentration and development of ischemic heart diseaseLancet 1975 1:16-19. [Google Scholar]
[73]. Austin MA, King M-C, Vranizan K, Krauss RM, The atherogenic lipoprotein phenotype (ALP): a proposed genetic marker for coronary heart disease riskCirculation 1990 82:495-506. [Google Scholar]
[74]. Zambon A, Austin MA, Brown BG, Hokanson JE, Brunzell JD, Effect of hepatic lipase on LDL in normal men and those with coronary artery diseaseArterioscler Thromb 1993 13:147-53. [Google Scholar]