Retinol Binding Protein 4 in Non Obese Psoriatic Cases
Ola Ahmed Bakry1, Mohamed Abdel Moneim Shoeib2, Iman Masoud Abdel Gayed3, Amany Said El Menoufy4
1 Assistant Professor, Department of Dermatology, Andrology and STDs, Faculty of Medicine, Menoufiya University, Egypt.
2 Professor, Department of Dermatology, Andrology and STDs, Faculty of Medicine, Menoufiya University, Egypt.
3 Lecturer, Department of Medical Biochemistry, Faculty of Medicine, Menoufiya University, Egypt.
4 Dermatology Specialist, Department of Dermatology, Andrology and STDs, Faculty of Medicine, Menoufiya University, Egypt.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ola Ahmed Bakry, Department of Dermatology, Andrology and STDs, Menoufiya Faculty of Medicine, Shebein El Kom-32817, Egypt.
E-mail: olabakry8@gmail.com
Dear Editor,
Psoriasis is a complex chronic inflammatory skin disease affecting approximately 2% of people living in western civilizations [1]. The disease is no longer regarded as a cutaneous disorder only. Psoriasis patients have been found to be at greater risk of developing co-morbid diseases, in particular, metabolic syndrome and vascular disorders. A fundamental pathological process that leads to skin manifestations and co-morbidities is chronic inflammation [2].
Retinol Binding Protein 4 (RBP4), a protein that belongs to the lipocalin family, was initially known as a specific carrier for the delivery of retinol in the circulation. It is expressed and secreted primarily by adipocytes and hepatocytes [3]. The association between RBP4 and different metabolic co-morbidities, closely linked to psoriasis, like metabolic syndrome, obesity and insulin resistance, suggests that RBP4 might be an adipokine of a meaningful role in psoriasis pathogenesis [4]. In the present work, serum RBP4 was measured by ELISA and lipid profile was evaluated in 55 non-obese psoriasis vulgaris cases and in 30 age, gender and Body Mass Index (BMI)-matched healthy subjects as a control group. Disease severity was assessed by Psoriasis Area and Severity Index (PASI) Score [1].
Obese subjects and those with disorders of lipid metabolism, dietary restriction, or intake drugs that may affect lipids were excluded. Subjects with psoriatic arthritis, dermatological diseases other than psoriasis and systemic or autoimmune diseases were also excluded. Cases included 30 males (54.5 %) and 25 females (45.5 %). Their age ranged from 17 - 57 years with mean ± SD age of 40.18 ± 9.08 years. Control group included 16 males (53.3 %) and 14 females (46.7%). Their age ranged from 21 to 62 years with a mean ± SD age of 39.17 ± 9.75 years. Regarding BMI among cases, it ranged from 21-29kg/m2 with mean ± SD BMI of 24.75 ± 2.46 kg/m2. Among controls, it ranged from 21-28 kg/m2 with mean ± SD BMI of 24.17 ± 1.88 kg/m2.
Clinical data of selected cases are shown in [Table/Fig-1].
Clinical data of selected cases.
| Variable | CasesN = 55 |
|---|
| Duration of the disease/monthX ±SDRange | 8.47±5.422 – 20 |
| No | % |
| Family historyPositive Negative | 946 | 16.483.6 |
| Type of psoriasisEarly onset (<35 y)Late onset (>35 y) | 3322 | 60.040.0 |
| SiteTrunkExtremitiesTrunk & Extremities | 22312 | 40.056.43.6 |
| Scalp affectionAbsentPresent | 469 | 83.616.4 |
| Palm & sole affectionAbsentPresent | 487 | 87.312.7 |
| Nail affectionAbsentPresent | 3916 | 70.929.1 |
| Mucosal affectionAbsentPresent | 4510 | 81.818.2 |
| ItchingAbsentPresent | 2530 | 45.554.5 |
| KobnerizationAbsentPresent | 3916 | 70.929.1 |
| PASI ScoreX ±SDRange | 31.67±7.3618 – 47 |
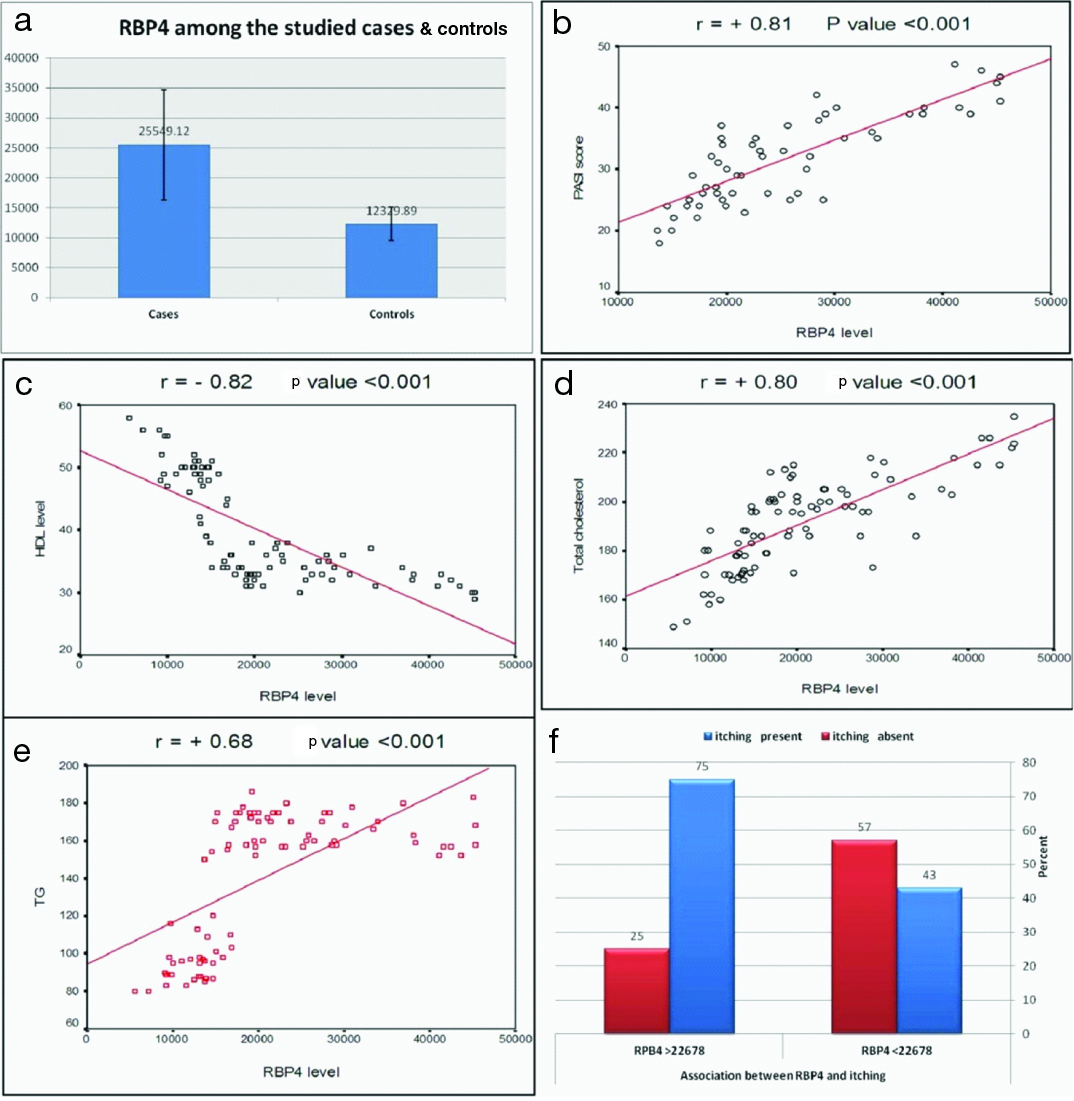
Total cholesterol and triglyceride levels were significantly higher among cases than among control group (p <0.001 for both), while high density lipoprotein cholesterol level was significantly lower among cases than among controls (p <0.001). Serum level of RBP4 was significantly higher in case group than controls (p<0.001) and its serum level was positively correlated with PASI Score, with total cholesterol and triglyceride levels and was negatively correlated with high density lipoprotein cholesterol in studied cases. Higher values were associated with itchy psoriatic lesions compared with asymptomatic ones [Table/Fig-2,3]. No significant relationship was detected between RBP4 level and other clinical data of selected cases.
a) RBP4 levels in studied cases and controls; (b) Significant positive correlation between RBP4 and PASI score; c) Significant negative correlation between RBP4 and high density lipoprotein cholesterol; d) Significant positive correlation between RBP4 and total cholesterol; e) Significant positive correlation between RBP4 and triglycerides; f) Association between high RBP4 serum levels and itching in studied cases.
Laboratory data of studied groups.
| Variable | The studied groups | Test | p-value |
|---|
| CasesN = 55 | ControlsN = 30 | t-test |
|---|
| HDL-C (mg/dl)X ±SD | 34.0±2.76 | 50.17±3.26 | 24.22 | <0.001 |
| Total cholesterol (mg/dl) X ±SD | 200.27±15.28 | 17.27±13.61 | 7.19 | <0.001 |
| Triglycerides (mg/dl) X ±SD | 165.82±9.42 | 95.07±10.49 | 31.80 | <0.001 |
| RBP4 (ng/ml)X ±SD | 25549.12±9182.79 | 12329.89±2759.18 | U test 7.21 | <0.001 |
HDL-C: high density lipoprotein cholesterol, X ±SD: mean± standard deviation, U test: Mann Whitney test; t-test: Student’s t-test
The significant differences in lipid profile between cases and controls were similarly reported in a previous study [5]. The demonstrated results of correlation between RBP4 level and measured lipids suggests its role in induction of dyslipidemia and unfavourable lipid profile and was consistent with previous reports [2,4].
The significant difference in RBP4 serum levels between cases and controls may provide evidence about the role of RBP4 in disease pathogenesis. The suggested mechanisms by which RBP4 may induce psoriasis could be through the induction of insulin resistance [6], induction of dyslipidemia and hypertension through the impairment of glucose and lipid metabolism and adipose tissue dysfunction [7], inducing expression and secretion of pro-inflammatory cytokines in primary human macrophages such as Tumor Necrosis Factor-α (TNF-α) and Interleukin-6 (IL-6) [3] that characterize psoriatic lesions [8] and inducing vasodilatation and angiogenesis [9].
In 1985, Rollman and Vahlquist investigated levels of RBP4 in the serum of 107 patients with psoriasis [10]. They found a normal mean serum concentration of RBP4 in patients with less than 25% body surface area affected and a significant lower serum RBP4 concentration in patients with a more extensive disease or pustular/erythrodermic psoriasis in comparison to 37 healthy controls [10]. However, authors did not mention BMI of their studied cases; were they obese or not. Contrary to our results, Baran et al., did not show any statistical difference between individuals with psoriasis and healthy ones regarding RBP4 serum level [4]. Their selected population included obese and non obese cases.
This discrepancy among results can be explained by the difference in number and clinical data of selected population in every study. Gerdes et al., found that the mean value of RBP4 was significantly lower in the patient group than controls [6]. The authors suggested that the decrease in the concentration of RBP4 could be a protective mechanism to prevent the development of insulin resistance and diabetes in a chronic inflammatory state as psoriasis. They added that, RBP4 which is a marker for insulin resistance and diabetes may be increased in severely affected psoriatic cases as diabetes is a well known co-morbidity in this patient population. The significant positive correlation between serum RBP4 and PASI score, detected in the present work, underscores the observation of Gerdes et al., [6]. To the best of our knowledge, no studies have investigated the association between RBP4 and itching in this disease entity; this is an area that requires further investigation.
[1]. Nestle FO, Kaplan D H, Barker J, PsoriasisN Engl J Med 2009 361:496-509. [Google Scholar]
[2]. Gerdes S, Mrowietz U, Impact of co-morbidities on the management of psoriasisCurr Probl Dermatol 2009 38:21-36. [Google Scholar]
[3]. Newcomer ME, Ong DE, Plasma retinol binding protein: structure and function of prototypic lipocalinBiochemica et Biophysica Acta 2005 1482:57-64. [Google Scholar]
[4]. Baran A, Swiderska M, Flisiak I, The effect of topical treatment and psoriasis severity on serum retinol-binding protein-4 levelsJ Dermatol Treat 2016 27:114-19. [Google Scholar]
[5]. Gul FC, Cicek D, Kaman D, Demir B, Nazik H, Changes of serum lipocalin-2 and retinol binding protein-4 levels in patients with psoriasis and Behçet’s diseaseEur J Dermatol 2015 25:195-97. [Google Scholar]
[6]. Gerdes S, Rostami-Yazdi M, Mrowietz U, Adipokines and psoriasisExp Dermatol 2011 20:81-87. [Google Scholar]
[7]. Christou GA, Tellis CC, Elisaf MS, Tselepis AD, Kiortsis DN, The changes in plasma retinol-binding protein 4 levels are associated with those of the apolipoprotein B-containing lipoproteins during dietary and drug treatmentAngiology 2011 63:67-75. [Google Scholar]
[8]. Lakshmi S, Nath AK, Udayashankar C, Metabolic syndrome in patients with psoriasis: A comparative studyIndian Dermatol Online J 2014 5:132-37. [Google Scholar]
[9]. Al khouri N, Lopez R, Berk M, Feldstein AE, Serum retinol binding protein 4 levels in patients with non-alcholic fatty liverJ Clin Gastroenterol 2009 43:985-89. [Google Scholar]
[10]. Rollman O, Vahlquist A, Psoriasis and vitamin A. Plasma transport and skin content of retinol, dehydroretinol and carotenoids in adult patients versus healthy controlsArch Dermatol Res 1985 278:17-24. [Google Scholar]