Osteochondroma of Bilateral Mandibular Condyle with Review of Literature
Vijaya Kamble1, Jitesh Rawat2, Ameya Kulkarni3, Nilufer Pajnigara4, Avinash Dhok5
1 Associate Professor, Department of Radiodiagnosis, NKPSIMS and Research Centre, Nagpur, Maharashtra, India.
2 Junior Resident, Department of Radiodiagnosis, NKPSIMS and Research Centre, Nagpur, Maharashtra, India.
3 Senior Resident, Department of Radiodiagnosis, NKPSIMS and Research Centre, Nagpur, Maharashtra, India.
4 Junior Resident, VSPM Dental College and Research Centre, Nagpur, Maharashtra, India.
5 Professor and Head of Department, Department of Radiodiagnosis, NKPSIMS and Research Centre, Nagpur, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jitesh Rawat, Junior Resident, Department of Radiodiagnosis, NKPSIMS and Research Centre, Nagpur- 440019, Maharashtra, India.
E-mail: jiteshsrawat@gmail.com
Osteochondroma (OC) is a common slow growing tumour of bone. This lesion is frequently seen in the axial skeleton and is relatively uncommon in oral and maxillofacial region. In facial bones, it usually affects the mandibular condyle followed by coronoid process. Very few cases of condylar osteocondroma have been reported in the literature. The aim of this article was to present an atypical case of osteochondroma of bilateral mandibular condyle in an asymptomatic patient and facilitate making an exact diagnosis of it. To the best of our knowledge this is the 2nd case of this type reported in literature.
Computed tomography, Temporomandibular joint, Benign tumour
Case Report
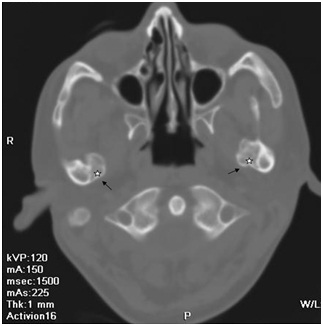
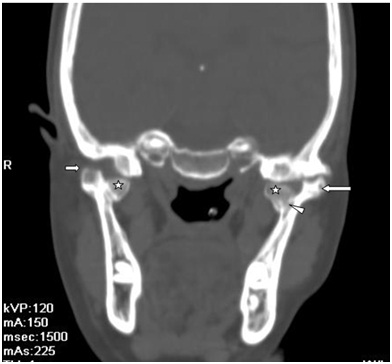
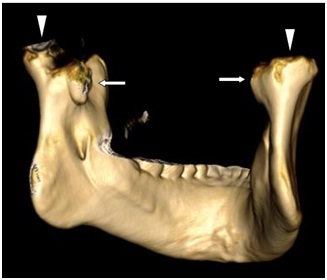
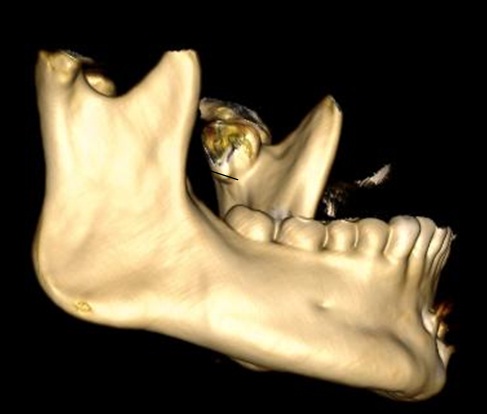
A 23- year-old male patient was referred to Department of Radiodiagnosis, from casualty for Computed Tomography (CT) brain who had chief complaint of sudden onset of weakness and giddiness. The CT brain revealed lacunar infarct in left lentiform nucleus with mild generalized cerebral atrophy. An incidental finding of bony protuberance was seen involving both the mandibular condyles. Patient was retrospectively evaluated for any symptoms related to bilateral Temporomandibular Joint (TMJ). Patient was found to be asymptomatic with no complaints in the TMJ region. TMJ movements were normal on palpation. No reduction in mouth opening or deviation of mandible was noted. CT scan showed multiple sessile, dense bony protuberances from the postero-medial aspect of the neck of bilateral mandibular condylar processes (left>right) which showed continuity with the cortex and medulla. It measured approximately 1.3cm X 0.9cm on right side and 1.4cm x 1.5cm on left side. These bony protuberances seemed to be projecting away from the TMJ with no involvement of the joint. Bony protuberances on both sides were attached to lateral pterygoid muscles of their respective sides [Table/Fig-1,2,3, 4 and 5]. Thus, on the basis of incidental radiographic and clinical features, a diagnosis of OC affecting bilateral mandibular condyles was given. Patient was asymptomatic till five months follow up and then he was lost to follow up.
Axial section of CT scan showing pathognomonic feature of osteochondroma with a lesion composed of cortical (arrow) and medullary (5-point star) bone protruding from the postero-medial aspect of neck of bilateral mandibular condylar processes (left > right) showing continuity with the cortex and medulla.
In coronal CT scan bony protuberance (5-point star) project away from the TMJ/ Condylar head (arrow) i.e., epiphysis with no involvement of it. Margins of this lesion appear to be calcified and show continuity with cortex. Lesion showing continuity (arrowhead) with medullary canal.
3D CT scan showing coronoid process (arrow) and head of mandibular condyle (arrowhead) appear normal.

3D CT scan showing head of mandibular condyle (arrow head) and left side and right side lesion (arrows).
3D CT scan showing lesion on the medial aspect of left mandibular condyle (arrow). The lateral side of ramus on right side appears normal.
Discussion
OC is a slow growing tumour of bone constitute 20%-50% of benign bone tumour and 10%-15% of all bone tumour [1]. In 2002, WHO defined OC as a cartilage capped bony projection arising from the outside surface of bone containing a marrow cavity that is continuous with that of the underlying bone appears close to the growth plate at the end of long bones [2]. It has its own growth plate and stops growing with skeletal maturity. Only about 1% of these occur within the head and neck region [3]. In oral and maxillofacial region, it usually affects the condyle followed by coronoid process i.e., extracondylar involvement. Involvement of posterior maxilla, zygomatic arch, maxillary sinus, body and symphysis of mandible have also been reported [4].
In condylar region, it is seen on medial aspect 52%, 20% on anterior location and 1% on lateral position [2]. Etiopathogenesis of OC can be explained by different theories neoplastic, developmental, reparative, and traumatic. Theory of aberrant foci of epiphyseal cartilage on the surface of the bone believes that formation of these tumours in the condyle is due to stress in the tendon insertion in region of lateral pterygoid muscle mainly where focal cumulation of cells with cartilaginous potential prevail. Consistent stimulation of lateral pterygoid muscle tendons during lateral excursions is also the reason for their growth along the medial aspect of condyle. Cases of traumatically and surgically induced OC known as secondary OC have also been reported [4,5].
The OC of mandibular condyle is extremely unusual. Very few cases of mandibular condylar OC have been reported in the literature [4]. A total of 108 cases were reported in English literatures until 2011. Revising the literature, Zhou Q et al., found about 215 cases of mandibular condylar OC. Bilateral involvement of condylar process is even rare. In 2015, Zhou Q et al. reported the first case of multiple OC of the bilateral condyle [2]. To best of our knowledge this is the second case we report where both condyles are involved.
Condylar osteochondroma usually occurs early in life affecting young adults between 10-30years of age but the craniofacial OCs are frequently seen in older women [6]. Males are three times more commonly affected than females [5]. Left condyle is more commonly affected than the right one [7]. Our case was a 23-year-old male patient who also had left side more affected than the right side. Usually it presents as a non-tender, painless cosmetic deformity related to the slowly enlarging exophytic mass. Facial asymmetry, cross-bite on contra-lateral side and lateral open-bite on the ipsilateral side, malocclusion, deviation on opening, hypomobility, pain and clicking are findings seen in cases of condylar OC [4,6,7]. Increase in height of condylar neck and ramus on affected side may occur [4]. Complications of OC are osseous deformity, fracture, vascular compromise,bursa generation and malignant transformation [5]. Our patient was found to be asymptomatic with no clinical signs. A diagnostic and pathologic characteristic of this lesion often reflects on radiographic appearance. Continuity of lesion with bone cortex and medullary canal is characterstic feature of OC which can be optimally depicted on three-dimensional imaging capability of CT [5].
CT can provide excellent anatomy of the lesion and demonstrate calcification in the cartilage cap whereas; MRI confirms the diagnosis by demonstrating the cartilaginous cap. Preoperative CT assessment can play an important role in the treatment planning of these tumours [4]. In CT scans soft tissue changes due to tumour growth and atrophy of masticatory muscles can be well seen [6].
The globular and lobulated mass may be found which often distorts the normal shape of the mandibular condyle and can be differentiated from the elongated condylar process seen in unilateral hyperplasia. Even after the termination of skeletal growth, OC may continue to grow progressively but growth ceases in condylar hyperplasia. However, treatment plan varies for both [4].
When considering the differential diagnosis of mandibular condylar osteochondroma, one must also consider other lesions like osteoma, condylar hyperplasia, OC, giant cell tumour, and metastatic disease in the list. Osteoma and osteochondroma appear similar but osteoma may be uniformly opaque and they are composed of compact bone or may show internal trabecular structure whereas OC usually has connection with medullary part of bone. Condylar hyperplasia shows an increased size of the condyle while maintaining its normal shape, but osteochondroma appears irregular. OC may show internal calcification which may assume the sunray pattern. Giant cell tumours are mostly present in anterior part of jaw and shows ill-defined wispy septa which are at right angles to the periphery. Metastatic diseases are usually destructive lesions in contrast to the well defined mushroom shaped appearance in OC [8,9].
Treatment includes supportive care with follow-up for minimally symptomatic small lesions and resection for larger ones [5]. When the OC involves the mandibular condyle, total condylectomy or local resection of the lesion and condylar replacement can be done. However, if the tumour affects only a limited part of the condylar surface, preservation of the remaining part of the condyle and reshaping can be done [6]. Follow-up was advised in our case as the patient was asymptomatic.
Recurrence rate after resection is about 2% and malignant transformation is extremely rare. Surgical resection of benign OC can lead to complications which are rare and is reported to occur in only 13% of patients. The complications include neuropraxia, arterial laceration, compartment syndrome, and fracture [8].
Conclusion
Osteochondroma of bilateral mandibular condyle presenting as asymptomatic mass is a rarity. Improved understanding of the clinical spectrum of this entity is essential. CT plays a crucial role in the correct diagnosis, timely execution of treatment plan and to prevent possible complications of malignant transformation.
[1]. Karras SC, Wolford LM, Cottrell DA, Concurrent osterchondroma of the mandible condyle and ipsilateral cranial base resulting in TMJ ankylosis. Report of a case and review of the literatureJ Oral Maxillofac Surg 1996 54:640-46. [Google Scholar]
[2]. Zhou Q, Yang C, Chen MJ, Osteochondroma of bilateral mandibular condyle: a case reportInt J Clin Exp Med 2015 8(2):2989-92. [Google Scholar]
[3]. Samir K, El-Mofty, Diagnostic Surgical Pathology of the Head and Neck 2009 2nd editionPhiladelphia, Pa, USASaunders [Google Scholar]
[4]. Andrade NN, Gandhewar TM, Kapoor P, Thomas R, Osteochondroma of the mandibular condyle–report of an atypical case and the importance of computed tomographyJ Oral Biol Craniofac Res 2014 4(3):208-13. [Google Scholar]
[5]. Murphey MD, Choi JJ, Kransdorf MJ, Flemming DJ, Gannon FH, Imaging of osteochondroma: variants and complications with radiologic-pathologic correlationRadiographics 2000 20(5):1407-34. [Google Scholar]
[6]. Utumi ER, Pedron IG, Perrella A, Zambon CE, Ceccheti MM, Cavalcanti MG, Osteochondroma of the temporomandibular joint: a case reportBraz Dent J 2010 21(3):253-58. [Google Scholar]
[7]. Gaines RE, Lee MB, Crocker DJ, Osteochondroma of the mandibular condyle: case report and review of literatureBr J Oral Maxillofac Surg 1992 50:899-903. [Google Scholar]
[8]. Morton KS, On the question of recurrence of osteochondromaJ Bone Joint Surg Br 1964 46:723-25. [Google Scholar]
[9]. White Stuart C, Pharoah M J, Oral radiology: principles and interpretation 2009 6th edSt. Louis, MoMosby Elsevier [Google Scholar]