Prosthetic Rehabilitation of Lower Limb with RTV Siliconee Using Prosthodontic Clinical and Laboratory Techniques - A Case Report
Pradeep C. Dathan1, T. Mohan Kumar2, Smitha Ravindran3, K. Chandrasekharan Nair4, Aswini Kumar5
1 Professor, Department of Prosthodontics, Sri Sankara Dental College, Thiruvananthapuram, Kerela, India.
2 Professor and Head, Department of Prosthodontics, Sri Sankara Dental College, Thiruvananthapuram, Kerela, India.
3 Senior Lecturer, Department of Prosthodontics, Sri Sankara Dental College, Thiruvananthapuram, Kerela, India.
4 Professor Emeritus, Vishnu Dental College, West Godavari District, Andra Pradesh, India.
5 Reader, Department of Prosthodontics, Amrita School of Dentistry, AIMS Campus, Cochin, Kerela, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pradeep C Dathan, Professor, Department of Prosthodontics, Sri Sankara Dental College, Thiruvananthapuram, Kerela, India.
E-mail: pdathan704@gmail.com
Amputation of all or part of a limb may be due to systemic disease, vascular disease, infection, local injury or trauma. Partially amputated lower limbs present a variety of unique clinical and prosthetic challenges, because of distinctly different amputation levels of the lower limb. A female patient with history of Partial Foot Amputation (PFA) surgery at metatarsophalangeal joint level, due to crush injury reported for prosthetic rehabilitation. This case was successfully rehabilitated using room temperature vulcanizing (RTV) medical grade silicone for fabrication of foot prosthesis. Though limited in its function, it amply proves that the clinical and laboratory techniques used in fabrication of maxillofacial prosthesis can be effectively adapted for the fabrication of body prosthesis like toes and feet to enhance the quality of life of the patients. The patient was reviewed every year for three years.
Foot prosthesis, Metatarsophalangeal disarticulation, Prosthesis, Prosthetic treatment, Silicone
Case Report
A 40-year-old female patient reported to the dental private practice with amputated phalanges and metaphalanges of the right foot for prosthetic rehabilitation. History reveled surgical resection was done following a crush injury six months back. On examination it was found that the amputated site was grafted and healed completely. There was no restriction of movement in the ankle joint [Table/Fig-1]. It was planned to fabricate a siliconee prosthesis which could be retained with a foot wear to restore the aesthetics and function. The treatment plan was discussed with the patient and she readily consented to the same.
Affected and unaffected feet.

Step by Step Fabrication of the Silicone Prosthesis
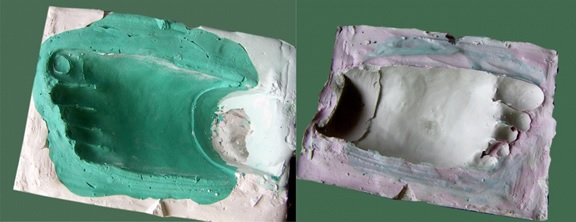
Impression making: Affected and the unaffected feet were cleaned using aseptic technique before making the impression. The impression was made using irreversible hydrocolloid (Zelgum, DPI, Mumbai, India). The irreversible hydrocolloid was mixed as per manufactures instructions and painted on to the surface of one foot at a time. The irreversible hydrocolloid impression was covered by surgical gauze [Table/Fig-2]. To reinforce the whole assembly it was covered with a layer of dental plaster (White gold, Asian Chemicals, Vadodara, India). After the dental plaster had completely set, the impression was removed using slow rocking movements. Dental stone (Gyprock, Asian Chemicals, Vadodara, India) was poured into impression of the affected foot and master cast was obtained free of voids or detects. The impression of the unaffected foot was made to serve as a mould to depict the morphology and aid in the fabrication of the wax pattern.
Impression of the affected foot.

Fabrication of wax pattern: The anterior aspect of the cast was covered with two sheets of modeling wax and a wax coping (sleeve) was made [Table/Fig-3]. In order to duplicate the toes, molten wax was poured into the impression of the unaffected foot [Table/Fig-4] and a wax pattern was fabricated. Each toe was then sectioned and modified to adapt to the affected side [Table/Fig-5]. Each toe was then attached to the posterior margin of wax sleeve coping extending up to the ankle of the amputed foot. A try in was carried out and necessary adjustments were made to match with the unaffected foot to alter and match the appearance as right toe, consent was obtained for the finished wax pattern [Table/Fig-6].

Pouring molten wax into the impression of unaffected foot.



Shade matching of silicone prior to packing: The siliconee base and activator paste was mixed in equal proportion, intrinsic stains (Factor II Staining Kit, Arizona, USA) were added to the mix, first white color was added to make the mix opaque then red followed by yellow colour which was added to achieve the colour of flesh, finally burnt umber was added to mimic the skin colour. Lightness and dark colour was achieved by altering the burnt umber. This was compared with the patient skin. Different shade of the color of the skin was identified and marked to make the skin light and dark to help in layering the siliconee during packing. Siliconee was mixed with different pigments to match the dorsal and ventral portion of the foot separately. While packing, the two mixes were appropriately placed and they were allowed to cure together. A separate addition of acrylic nail was not planned and placed as the nail was also planned to be layered during packing to match color in siliconee prosthesis.
Fabrication of the silicone prosthesis: A flask less mold was planned for investing the wax pattern. A two piece mold was made in dental plaster and dental stone was used as coring to record the finer details. A key and keyway was placed on two sides in the two piece mould for checking complete re seating of the two half during packing. After complete setting of the plaster the two pieces of the mold were separated wax pattern was removed. Separating medium was applied on both the halves of the mold [Table/Fig-7]. Room Temperature Vulcanization (RTV) siliconee (Factor II A 2000, Arizona, USA) was mixed in equal proportion; and the mold was packed with the stained siliconee [Table/Fig-8]. The mold was kept under compression for 24hours as per the manufacturer’s instructions. After 24hours the mold was opened and the prosthesis was retrieved [Table/Fig-9]. It was then finished by trimming the excess material. External staining was not done and the nails were also in siliconee. This was done by packing clear siliconee into the nail bed and finally the stained siliconee was layered on top to mimic the natural nail. The foot wear was custom made to accommodate the amputated foot and the silicone prosthesis.


The retention of the prosthesis was insured by close approximation of the silicone prosthesis to the tissues and the suction generated between the prosthesis and the amputated foot. It was further reinforced by the custom made foot wear. The patient was instructed to wear the prosthesis along with the foot wear [Table/Fig-10]. The patient was followed up for three-five years after the prosthesis was fabricated.

Discussion
Amputation is the removal of all or part of a limb or any other portion of the body by trauma or surgery [1]. The surgical removal is necessary when there is interruption of blood supply due to systemic or vascular disease, infection, local injury or trauma. Partially amputated lower limbs presents a variety of clinical challenges, because of distinctly different levels of amputation. The various levels of amputation were based on the type of surgical resection as longitudinal and ray resection or transverse section techniques. The transverse amputation of the foot as per the levels is metatarsophalangeal disarticulation, transmetatarsal, tarsometatarsal (LISFRANC) and trans tarsal level (CHOPART) [2,3].
Medical literature suggest various interventions for managing different residual limbs using prosthetic, orthotics techniques and relevant materials [Table/Fig-11] [4,5]. These devices were fabricated using wood, leather, metal and recently foam that did not permit any movement. Polypropylene, polyester and polyurethane that were rigid with less weight were also used. Siliconee elastomers used for prosthetic rehabilitation are soft and resilient material providing comfort (relieving pressure from sensitive areas), aesthetic (restoring the foot length) and provide a psychological sense of wholeness compared to the other materials [6–8]. The emphasis was always towards rigidity and prosthetic failure which occurred mainly due to skin breakdown. One of the major challenges when treating PFA is to provide a prosthesis that balances the often conflicting requirements of walking function, skin protection, user comfort, and cosmetics. In addition, creating an appropriate prosthetic foot for different levels of amputation presents technical challenges.
Various prosthetic materials used along with advantages and disadvantages.
| S.No. | Material | Advantage | Disadvantage |
|---|
| 1 | Siliconee | • Non-reactive • Thermally stable/ Non-combustible • Electrically insulating • Optical clarity • High permeability to gases • Radiation resistant • High purity • High elongation (typically 600 - 1000%) • Good tear strength • Unique modulus at typical elongation • Controllable softness • Low compression set • Oxygen permeability • Bio-inert | Deterioration of properties on continued use |
| 2 | Carbon | High strength, Light weight, Chemically inert | Brittle, Expensive, low impact strength low shear modulus |
| 3 | Polyethylene | Low cost, Easy processibility, Freedom of odour and toxicity, Very good chemical resistance, Excellent insulator | Environmental stress cracking, poor scratch resistance, low tensile strength |
| 4 | Polyurethane | Excellent, tear and abrasion resistance, Low resilience, comparative, low cost | Difficult to pigment, Subject to attack by solvents, Poor thermal capability |
| 5 | Polystyrene | Free from odour and taste, Low cost, Good moldability, Low moisture absorption | Poor thermal stability, Environmental stress cracking, Subject to attack by solvents, Brittleness |
Partially amputated limb is not easily rehabilitated because of its functional and aesthetic specificities. The material used should be easily mouldable and should not change the dimensions of the limb. Hence, siliconee was used in this case. Stronger materials like titanium and carbon are used for total replacement of foot or the limb. The siliconee material used in this case has not been tried before for similar situations.
To avoid the limb length inequality, a customized prosthetic shoe is to be fabricated owing to limited space between distal end and the regular shoe [9].
A well-crafted custom siliconee prosthesis cannot only aid in scar tissue management and residuum protection but it can also restore the patients’ self -confidence and psychosocial well-being [10]. The use of siliconee improved the comfort of wearing the prosthesis. However, limited in function the prosthesis was well accepted by the patient.
The case was followed up for a considerable period of time (6 months). Techniques employed in this case are exclusively those commonly used in any dental clinic. Patients who cannot afford expensive prosthesis can be rehabilitated by a willing prosthodontist.
Conclusion
In this case report the prosthodontic clinical and laboratory techniques have been adapted to fabricate foot prosthesis. Rehabilitation of PFA defect with the prosthesis not only resulted in improved social interaction, function and comfort of the patient it also contributed to the physical and mental well being of the individual in improving the quality of life of the patient.
[1]. Maheswari U, Mohamed K, Deora N, Elavia U, Padmanabhan TV, Flexible cosmetic siliconee toe and foot prostheses in developing countries–case reportsJ Prosthet Orthop 2011 23(4):204-10. [Google Scholar]
[2]. Berke GM, Rheinstein JCP, Michael JW, Stark GE, Biomechanics of ambulation following partial foot amputation: a prosthetic perspectiveJ Prosthet Orthop 2007 19(3S):85-88. [Google Scholar]
[3]. Dillon MP, Partial Foot Amputation: Aetiology, Incidence, Complications, Prosthetic Intervention and a characterization of gait. In Stone JH, Blouin M. editorsInternational Encyclopedia of Rehabilitation 2010 NewyorkSpringerAvailable Online : http://cirrie.buffalo.edu/encyclopedia/en/article/154/ accessed on January 9, 2016 [Google Scholar]
[4]. Siliconee in prosthetics – Properties and Use. Available online : http://www.ru.is/media/tvd/skjol/Siliconee-in-prosthetics-HR-2016.pdf Accessed online may 26, 2016 [Google Scholar]
[5]. Prosthetic Foot Design. Available online: www.monash.edu.au/rehabtech/research/footmult.pdf. Accessed online may 26, 2016 [Google Scholar]
[6]. Strait E. Prosthesis in developing countries. Prosthetic Resident 2006 (January). www.oandp.org/publication/resident/pdf/Developing-Countries.pdf. Accessed January 9,2016 [Google Scholar]
[7]. Craig J, Prosthetic feet for low-income countriesJ Prosthet Orthop 2005 17:47-49. [Google Scholar]
[8]. Stills ML, Partial foot prostheses/orthosesClin Prosthet Orthot 1988 12:14-18. [Google Scholar]
[9]. Fillauer K, A prosthesis for foot amputation near the tarsal-metatarsal junctionOrthot Prosthet 1975 29:02-09. [Google Scholar]
[10]. Putnam RD, Exploring the applications of semi custom siliconee partial foot prostheses in a pediatric amputee populationACPOC News 2009 15(3):18-37. [Google Scholar]