Prosthetic Rehabilitation of Squamous Cell Carcinoma of Orbit: A Clinical Report
Prana Shakya1, Natdhanai Chotprasert2, Theerathavaj Srithavaj3
1 Teaching Assistant, Maxillofacial Prosthetic Clinic, Department of Prosthodontics, Faculty of Dentistry, Mahidol University, Bangkok, Thailand.
2 Lecturer, Maxillofacial Prosthetic Clinic, Department of Prosthodontics, Faculty of Dentistry, Mahidol University, Bangkok, Thailand.
3 Assistant Professor, Maxillofacial Prosthetic Clinic, Department of Prosthodontics, Faculty of Dentistry, Mahidol University, Bangkok, Thailand.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Theerathavaj Srithavaj, Maxillofacial Prosthetic Clinic, Department of Prosthodontics, Faculty of Dentistry, Mahidol University, 6 Yothi Street, Rajthevee, Bangkok-10400, Thailand.
E-mail: t-kung7@hotmail.com
Maxillofacial defect, Orbital exenteration, Orbital prosthesis
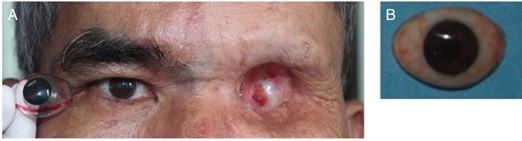
A 61-year-old male patient reported with a chief complaint of loss of left eye [Table/Fig-1a]. The patient had a history of squamous cell carcinoma involving the left orbit. Patient consent was obtained prior to treatment. Surgical treatment was conducted by orbital exenteration and external beam radiotherapy, with a total dose of 4000 cGy delivered at a dose of 200 cGy in 20 daily fractions. Thereafter, the patient was referred for fabrication of an orbital prosthesis. The patient did not present with any systemic diseases and no evidence of known allergies or recurrence of tumor was evident.
(a) Patient pretreatment; Clinical examination of the orbital defect following SCC, showing; (b) Anatomic undercut on the superior-medial aspect, fistula on central aspect of defect, soft tissue fibrosis at infraorbital rim; (c) Impression making of the orbital defect and adjacent tissues.

On clinical examination, no gross facial asymmetry was noted as revealed by the rule of fifth assessment [1]. The hard tissue examination exhibited an intact superior and inferior orbital rim and zygomatic bone, and adequate amount of anatomical undercut on the superior-medial aspect of the defect. Three fistulas were present at the superio-medial, medial and central aspect of defect, as a complication of exenteration [Table/Fig-1b]. Mild soft tissue fibrosis was observed at the infraorbital rim and no evidence of flaps placed indicated healing by spontaneous epithelialization. The depth of defect was adequate for retaining an orbital prosthesis. Loss of hair follicles at the left eyebrow was evident as a result of high dose of radiotherapy [Table/Fig-1a,1b]. The treatment plan comprised fabrication of left orbital prosthesis, utilizing superio-medial undercut for anatomical retention further aided by skin adhesive.
Impression and Working Cast: The extension of the prosthesis over the immobile tissues was marked and unfavorable undercuts blocked out. Superio-medial undercut was engaged for anatomical retention. Impression was made with irreversible hydrocolloid impression material (Kromopan, Lascod, Italy) and Type II dental plaster (Plaster Powder Gypsum, Siam Gypsum Plaster LP, Bangkok, Thailand) [Table/Fig-1c] reinforcement. The impression was immediately poured with Type IV white dental stone (Lafarge Prestia, Bangkok, Thailand).
Fabrication of Ocular Prosthesis: Subsequently, a stock conformer that best replicates the patients’ eye was selected. Measurements of the iris diameter, shade and sclera shade selection were done, ocular prosthesis was fabricated [Table/Fig-2a,b]. The initial wax-up was sculpted, tried on the patient, and precise contour, position of iris, curvature of eyelids finalized. An inadequate tissue contact at the lateral margin of the supra-orbital rim was observed during patients’ facial expression [Table/ Fig-3a]. This was corrected by scoring the cast and further wax adaptation [Table/Fig-3b-c].
(a) Selection of aesthetic conformer; (b) Final ocular prosthesis fabricated.
(a) Initial wax-up; (b) Final adaptation of the wax-up following scoring of cast, (c) Final detailing and texturing; (d) Silicone prosthesis after intrinsic staining; (e) Silicone prosthesis tried on patient after intrinsic staining.
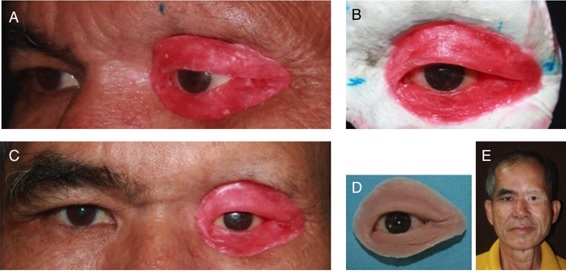
Elimination of Open Margin of Orbital Prosthesis: Scoring of the master cast was done in areas of displaceable tissue to ensure tissue contact at the margins, and better aesthetic transition between the junction of the prosthesis and adjacent skin. First the areas of deficient tissue contact were marked on the patient and transferred to the cast accordingly. Depth orientation grooves were made respectively, excess on the cast reduced, and finally sandpapered to smoothen. The wax-up was then placed on the mold and wax added along the scored cast [Table/Fig-3b]. The adjusted wax sculpture tried on patient and a smooth, well-adapted juncture of wax margin and tissue was obtained [Table/Fig-3c].
Finally, carving and characterization of details: wrinkles, grooves and surface texture were precisely replicated, and mold poured with type IV dental stone.
Silicone Mixing and Intrinsic Staining: Following dewaxing, the mold was coated with separating medium (Tinfoil Substitute, Factor II Inc, Arizona, USA) and chair-side mixing of addition-RTV silicone (Episil, Dreve-Dentamind GmbH, Unna, Germany) was done. Two shades of Episil were combined, Europa 1 and Asien 2 in the ratio of 2:3. Intrinsic staining (Factor II Inc., Arizona, USA) and flocking was incorporated to achieve the base shade in reference to the lightest skin tone of the patient. After polymerization, flash and minor irregularities were removed [Table/Fig-3d,3e].
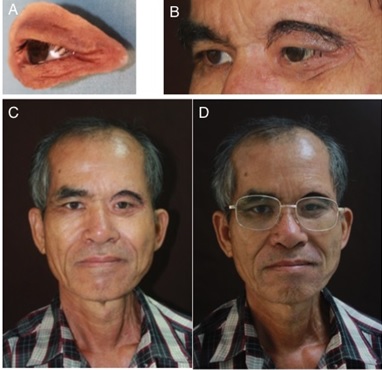
Extrinsic Staining and Prosthesis Delivery: The prosthesis was extrinsically stained (Dry Earth Pigments, Factor II Inc, Arizona, USA), and coated with acetoxy silicone adhesive (Medical Adhesive A-100, Factor II Inc, Arizona, USA), deglossed, matted and cured [Table/Fig-4a]. The eyelashes and eyebrows were incorporated by stitching donor hair onto the silicone, using a 27-gauge dental needle (Terumo Corporation, Tokyo, Japan) oriented parallel to the direction of hair. The eyebrow was precisely outlined with extrinsic stain prior to insertion of the hair, utmost care was taken to match them to the fellow orbit in terms of colour and contour [Table/Fig-4b]. The prosthesis was delivered to the patient [Table/Fig-4c, 4d] and post-insertion instructions were emphasized to the patient.
(a) Silicone prosthesis after extrinsic staining and matting, tried on patient; (b) prosthesis tried on patient after extrinsic staining and matting; (c,d) Patient post-treatment, orbital prosthesis delivered.
Discussion
The loss of hard and soft tissue from exenteration and further tissue alterations due to radiotherapy decreases vascularity, changes the quality of soft tissue causing fibrosis, edema, and that of bone causing sequestration or progressive osteonecrosis [2]. Thereby, in cases with a history of radiotherapy, the retention of orbital prosthesis is better achieved by anatomical undercuts along with medical adhesive rather than the use of craniofacial implants.
Orbital prosthesis is a safe, and a widely accepted means of orbital defect rehabilitation. The success of an orbital prosthesis depends on size and extent of defect, quality of residual hard and soft tissue, presence of a soft tissue graft and accuracy of impression technique. The prosthetic margins placed in movable tissue bed decreases the amount of retention of the prosthesis and prevent the margins from being camouflaged within the borders of the defect [3,4]. During facial expression, the primary depressors of the forehead and eyebrows: procerus, corrugator supercilii, orbicularis oculi, and depressor supercilii muscles and the frontalis raise the forehead/eyebrows [5]. The hard and soft tissue of the defect differs significantly with each patient. In this patient the superior margin of the prosthesis was placed over surrounding movable tissue. One of the challenges in orbital rehabilitation is to obtain an accurate working cast that replicates displaced soft tissue contours. In case of highly displaceable soft tissue surrounding the defect, wax incremental technique along with scoring the cast yields desirable results, as it is less time consuming and an accurate technique to obtain an adequate prosthesis-tissue seal.
[1]. Naini F B, Facial aesthetics concepts and clinical diagnosis 2011 UKWiley-Blackwell:150-164. [Google Scholar]
[2]. Cooper JS, Karen FU, Marks J, Silverman S, Late effects of radiation therapy in the head and neck regionInt J Radiation Oncology Biol Phys 1995 14(5):1141-64. [Google Scholar]
[3]. Beumer J, Rehabilitation of facial defects. In: Beumer J, Marunick MT, Esposito SJ, editorsMaxillofacial Rehabilitation 2011 3rd edChicagoQuintessence:255-313. [Google Scholar]
[4]. Kiat-Amnuay S, Lemon JC, Wesley PJ, Technique for fabrication of lightweight, urethane-lined silicone orbital prosthesisJ Prosthet Dent 2001 85:210-13. [Google Scholar]
[5]. Tan KS, OH S, Priel A, Korn BS, Kikkawa DO, Surgical anatomy of the forehead, eyelids, and midface for the aesthetic surgeon. In: G.G. Massry et al., editorsMaster Techniques in Blepharoplasty and Periorbital Rejuvenation 2011 CaliforniaSpringer:11-24. [Google Scholar]