Delayed Open Reduction and K-Wire Fixation of Widely Displaced Supracondylar Fractures of Humerus in Children using Medial Approach
Sanjib Waikhom1, Sagnik Mukherjee2, Irom Ibomcha3, Akoijam Digendra4, Handboy R Sohkhlet5
1 Associate Professor, Department of Orthopaedics, Regional Institute of Medical Sciences, Imphal, Manipur, India.
2 Post Graduate Trainee, Department of Orthopaedics, Regional Institute of Medical Sciences, Imphal, Manipur, India.
3 Professor, Department of Orthopaedics, Regional Institute of Medical Sciences, Imphal, Manipur, India.
4 Post Graduate Trainee, Department of Orthopaedics, Regional Institute of Medical Sciences, Imphal, Manipur, India.
5 Post Graduate Trainee, Department of Orthopaedics, Regional Institute of Medical Sciences, Imphal, Manipur, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sagnik Mukherjee, Room No.109, Gents’ Hostel 5, Regional Institute of Medical Sciences Campus, Lamphelpat, Imphal West-795004, Manipur, India.
E-mail: mukherjeesagnik134@gmail.com
Introduction
Supracondylar fractures of humerus in children are usually treated with percutaneous pinning on emergency basis. When the operating time is delayed, percutaneous pinning is difficult due to massive swelling. Late presentation is common in developing countries.
Aim
To assess the outcome of open reduction and internal fixation with K-wire of widely displaced supracondylar fracture when operated later than 2 days after the injury.
Materials and Methods
A total of 52 children (aged 3-12 years) with widely displaced supracondylar fracture of humerus (Gartland type-III) who presented later than 2 days after injury were treated with open reduction through medial approach and fixation with cross K-wires. Results were assessed with Flynn’s criteria.
Result: A total of 40 patients completed follow-up. Mean age of all (n=52) patients was 4.8 years (range 3-12 years). Mean delay of presentation was 7.5 days (range 2-14 days). Hundred percent patients had satisfactory results according to Flynn’s criteria. Two patients had pin infections.
Conclusion
Open reduction through medial approach and fixation with two cross K-wires is a reliable method of treatment for supracondylar fractures of humerus in children when the operation is delayed.
Bone wires, Child, Humeral fracture surgery
Introduction
Supracondylar fracture of humerus is one of the most common fractures in children and it constitutes about 17% of all paediatric fractures [1]. Displaced supracondylar fractures are conventionally treated with closed reduction and percutaneous pinning on emergency basis [2]. However, late presentation and delayed surgery are common in developing countries due to various reasons [3]. Late presentation is defined as fractures presenting 2 days after injury [4,5]. However, authors from developed countries define “delay” as more than 8-12 hours in their studies and there is no significant difference in the outcome of the early and delayed groups in their studies [6–9]. Their results and conclusions are not applicable in a clinical situation where the delay is in days or weeks. Only few reports are available on the treatment with delay more than two days [3–5,10]. Some similar studies are summarized in [Table/Fig-1]. Also, the necessary equipments particularly C-arm may not be available in emergency OT set up for percutaneous pinning. However open reduction and internal fixation has earned a poor reputation because of elbow stiffness and myositis ossificans that may develop later on [11].
Various studies describing delayed fixation of supracondylar fractures of the humerus in children.
| Serial No. | Study | Year | Delay in surgery | Comments |
|---|
| 1 | Iyengar et al., [6] | 1999 | Delay defined as more than 8 hours since injury. | Comparison was done between early and late pinning. |
| 2 | Mehlman et al., [7] | 2001 | Delay defined as more than 8 hours since injury. | Comparison was done between early and late pinning. |
| 3 | Leet et al., [8] | 2002 | Mean delay from injury to surgery was 21.3 hours. | Mean delay at presentation -9.8 hoursMean delay from emergency to surgery was 11.5 hours. |
| 4 | Gupta et al., [9] | 2004 | Delay defined as more than 12 hours since injury. | Author studied the Effect of surgical delay on perioperative complications and need for open reduction. |
There is some controversy related to approach. The approaches are lateral [12], medial [3], posterior [13] and anterior [1]. Posterior approach goes through uninjured triceps and posterior periosteum and is hence associated with stiffness [1]. Anterior approach is of choice when the fracture is associated with vascular injury [1]. Medial column communition and internal rotation of the distal fragment could not be managed adequately through a lateral or posterior approach in some series [1].
Hence, a study was designed with the objective to assess the outcome of open reduction and internal fixation with crossed K-wires of widely displaced supracondylar fracture when operated later than 2 days after injury through the medial approach.
Materials and Methods
A prospective study was conducted at Regional Institute of Medical Sciences, Imphal, India. After due approval of the protocol from the Institutional Ethical Committee, all 52 patients with widely displaced supracondylar fracture of humerus (Gartland type-III [14]) who presented later than 2 days after injury between June 2008 and December 2012 were included in the study. After taking informed consent from the guardians, patients were operated and followed up for at least 2 years. A total of 12 patients could not be traced and their data was excluded. Patients with flexion type of fracture, open fractures, neurovascular injury, history of manipulation more than once, massaging or those who presented within 48 hours of injury were excluded from this study. Patients were given an above elbow slab after a minimal manipulation, just to correct the gross deformity and admitted to the ward. Patients were operated as a routine case in the next morning by a senior consultant.
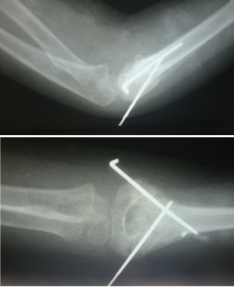
General anaesthesia and tourniquet were used in all the cases. Patients were operated in the supine position keeping the affected limb on a side table [Table/Fig-2], pre-operative radiograph show in [Table/Fig-3]. Medial approach was used in all the cases. Medial epicondyle was marked. A medial longitudinal incision of about 5 to 7cm, commencing 3 to 4cm proximal to the medial epicondyle and 0.5 to 1cm anterior to the tip of medial epicondyle was placed. Basilic vein if found, was either retracted or ligated. Deep fascia was incised along the line of skin incision. Ulnar nerve was identified but not dissected out. Proximal fragment was exposed first. Deeper dissection was already done by the injury itself. It was usually found that brachialis had been torn or split and fracture fragment was lying just below the skin. Periosteum around the proximal fragment was stripped off by the injury itself. A small bone lever was inserted anterior to the proximal fragment and fracture end was cleaned and clot thoroughly removed. Then the distal fragment was exposed. Around 5 to 10mm of common flexor muscle attachment was elevated from the bone with sharp dissection. Stripping off soft tissue from the distal fragment was minimised least it could cause avascular necrosis. With this approach, anterior and medial side of the fracture could be visualised clearly. Proximal fragment was held with a small reduction forceps. One 6mm periosteal elevator was introduced between the fracture fragments to lever out the distal fragment which was lying posteriorly. Anatomical reduction was usually achieved. Some comminution was found at the medial column but did not create a major reduction problem. Once reduced, it was fixed with two 1.5 or 2.0 mm cross K-wires. Medial K-wire was drilled through the medial epicondyle, crossed the fracture and came out at the antero-lateral surface of the proximal fragment. Power drill was always used. Lateral K-wire drilled through the lateral epicondyle, crossed the fracture and came out at the antero-medial surface of the proximal fragment [Table/Fig-4]. The surgeon kept the tip of the index finger of the non- dominant hand at the desired point of exit of K-wire so that stereognosis helped in insertion and directing the path of K-wire. In all the cases, the K-wires were crossed above (proximal to) the fracture. Fixation was checked for stability. Wires were cut and left outside the skin to facilitate easy removal without requirement of a second major procedure. Elevated common flexor origin was sutured by taking the suture around the K-wire instead of drilling into the bone. Wound was closed. Above elbow Plaster of Paris (POP) slab was applied. Suction drain was not used. From the third day, POP slab was removed during day time and arm was kept in an arm sling. Range of motion exercise was started and POP slab was used as night splint. Sutures and splint were removed on the 10th postoperative day. Patients then continued active exercises at home. Help of physiotherapist was not sought. The patient and the parents were informed about the harmful effects of massage and passive exercises. The child was allowed to attend school after suture removal, covering the exposed K-wire with dressings. K-wires were cleaned twice weekly at home by the parents according to the instructions provided by the surgeons. The K-wires were removed at 4 weeks at OPD without anaesthesia. Patients were followed every two weeks for 3 months to ensure proper exercise. By three months, fracture was usually united and function was near normal. The patients were examined at one year and two years [Table/Fig-5,6 and 7]. Elbow ROM was recorded with a goniometer. Carrying angles of both sides were measured with goniometer. The results were graded using Flynn JC et al., criteria, shown in [Table/Fig-8] [15]. In this criteria cosmetic factor was measured by loss of carrying angle which is measured clinically by using a goniometer and compare with normal side. Functional factors were measured by loss of motion as compared to normal side.
Clinical photograph before surgery. Elbow is seen grossly swollen with blisters.

Pre-operative radiograph shows widely displaced supracondylar fracture of the humerus. Main displacement is seen to be lateral.

Postoperative photograph. Lateral view is shown in (a) and anteroposterior in (b). Fracture is seen to be fixed with crossed K-wires. Anatomical reduction has been achieved.
Clinical photograph of follow-up 24 months after surgery of the operated limb in extension. Full range of extension is seen comparable to the normal limb.

Clinical photograph of follow-up 24 months after surgery of the operated limb in flexion. Full range of flexion is seen comparable to the normal limb.

Postoperative radiograph at 2 year follow up showing anteroposterior and lateral views. Fracture resolution is noted. There is no evidence of myositis ossificans or bony bar formation. Normal anatomy is restored.

| Results | Rating | Cosmetic factor (Loss of carrying angle in degrees) | Functional factor (Loss of motion in degrees) |
|---|
| Satisfactory | Excellent | 0-5 | 0-5 |
| Good | 6-10 | 5-10 |
| Fair | 11-15 | 10-15 |
| Unsatisfactory | Poor | >15 | >15 |
Results
A total of 40 children completed follow up. Of them, 24 (60%) were boys and 16 (40%) were girls. Mean age (of the 52 cases) was 4.8 years (range 3-12 years). Right side was involved in 22 (55%) and left side was involved in 18 (45%) of the patients. The mean delay in presentation was 7.5 days (range 2 to 14 days). The mean period of hospitalization was 8.5 days (range 5 to 10 days). Puckering of skin was seen in 8(20%) of cases. Distal fragment was displaced posteromedially in 29 (72.5%) cases and posterolaterally in 11(27.5%) cases. Mean tourniquet time during surgery was 45 minutes (range 35 to 60 minutes). At 3 months, 6 patients (15%) had unsatisfactory result according to Flynn’s criteria due to loss of motion more than 15°. At 1 year, with continued supervised ROM exercises, all these patients had improved range of motion and reached the satisfactory result category according to Flynn’s criteria. They maintained this satisfactory result at 2 years. Hundred percent patients had satisfactory results according to Flynn’s criteria at two year follow up. Details of the results are tabulated in [Table/Fig-9]. Carrying angle of the normal side was 11.8°. The mean change in carrying angles in the 6 patients who were graded as “good” was 6.5° (range 5-10°). Loss of extension was the main cause of loss of motion. Two patients had superficial pin infection, which subsided with antibiotic treatment. None had myositits ossificans, gross limitation of motion, iatrogenic nerve injury, cubitus varus deformity needing surgical correction, trochlear necrosis or surgical site infection.
Discussion
Open reduction is normally done in cases with vascular injuries and failed closed reduction. Late presentation is one of the most important causes for failure of closed reduction [16]. Late presentation is common in developing countries. Operation may be further delayed due to non-availability of OT timing or shortage of manpower or equipments. Yildrim et al., had reported that closed reduction is not feasible after 3 days [17]. Gupta K et al., had to try closed reduction as many as six times in some of their cases to achieve good reduction [18]. Repeated attempts can lead to poorer results [15]. When to label closed reduction as unsuccessful in a case is not clearly defined in the literature. Open reduction has a poor reputation because of joint stiffness after the procedure. Poorer results are probably because of its use only in the worst cases where all methods have been repeatedly tried. [Table/Fig-10] summarizes the results and conclusions of some similar studies [3–5,10,12,15,19–21]. Primary concern of open reduction is joint stiffness and myositis ossificans. Myositis ossificans is reported in two studies where late cases were treated with open reduction [4,15], but it is not reported in others where the fresh cases were treated with open reduction [8,15,16]. Even in these studies, the incidence of myositis ossificans is reported as 5%. This low incidence cannot justify abandoning open reduction for supracondylar fractures of humerus. Satisfactory results for open reduction (according to Flynn’s criteria) in fresh and late cases ranges from 87.5% to 100% in various studies (as summarized in [Table/Fig-9]) excluding the results of Yaokreh et al., where posterior approach was used [5]. C-arm is not available in most district hospitals of North-East India. Similar situations may be encountered elsewhere in the world. If open reduction is routinely practiced and encouraged, more patients will get benefitted than harmed.
Overall rating using Flynn’s criteria.
| Result | Rating | OverallNo of patients (Percentage) | Cosmetic factor (loss of carrying angle)No of patients (Percentage) | Functional factorNo of patients (Percentage) |
|---|
| Satisfactory | Excellent | 28 (70%) | 34 (85%) | 28 (70%) |
| Good | 12 (30%) | 6 (15%) | 12 (30%) |
| Fair | 0 | 0 | 0 |
| Unsatisfactory | Poor | 0 | 0 | 0 |
The lower of the two gradings, cosmetic factor and functional factor was taken in the overall grading.
| Serial no. | Study | Year | No of cases | Mean delay and range of days | Methods | Approach | No of patients with satisfactory results (Flynn’s criteria) | Complications (no of patients as percentage) | Remarks |
|---|
| 1 | Flynn et al., [15] | 1974 | 52 | Fresh cases | CRPP | - | 98% | MO- 2%CV-4% | |
| 2 | Kamath et al., [19] | 2003 | 54 | Fresh cases | ORIF with K-wire | Medial, lateral, posterior | 95% | MO-5%PI-6.5%SSI-2% | |
| 3 | Tiwari et al., [4] | 2007 | 40 | 4.5 (2-12) | CRPP- 64%ORIF-36% | Mediolateral, triceps sparing | 87.5% | MO-5%PI-6.5%TN-5% | Results of CRPP and ORIF is combined |
| 4 | Eren et al., [3] | 2008 | 31 | 6 (2-19) | ORIF with cross K- wire | medial | 100% full range of motion | CV-22.5%PI-6.5%SSI-7.8%IN-3.4% | Flynn criteria not used |
| 5 | Yaokreh et al., [5] | 2012 | 89 | 4.5 (2-17) | ORIF with cross K- wire | posterior | 83.2% | CV-3.4%Loss of ROM-12.4% | |
| 6 | Tahir et al., [10] | 2012 | 40 | 5 (2-14) | ORIF with cross K- wire or lateral K- wire | lateral | 95% | Mo-5%PI-6.5% | |
| 7 | Aslan et al., [20] | 2014 | 54 | Fresh cases | ORIF with cross K- wire | Lateral, medial, posterior, anterior | 90% | PR-7.4%CV-9.3% | |
| 8 | Hussain et al., [12] | 2014 | 52 | Fresh cases | ORIF with cross K- wire | Lateral | 90.4% | PI-10% | Gartland TypeII fractures also included |
| 9 | Khan et al., [21] | 2015 | 79 | Fresh cases | ORIF with cross K- wire | Medial | 97.5% | - | |
| 10 | Present study | 2016 | 40 | 7.5 (2-14) | ORIF with cross K- wire | Medial | 100% | PI- 5% | |
Abbreviations:-CRPP- Closed reduction and percutaneous pinning; ORIF- Open reduction and internal fixation; MO- Myositis ossificans; TN- Trochlear necrosis; IN- Iatrogenic nerve injury.; CV- Cubitus varus.; SSI- Surgical site infection.
Limitation
This was not a comparative study between closed and open reduction. Case series or prospective studies cannot substantiate the harmful effects of open reduction compared to closed reduction and percutaneous pinning. A matched pair comparative study between closed reduction and open reduction in late cases will better highlight whether open reduction can be continued to be used or to be abandoned.
Conclusion
The authors do not recommend using open reduction in all cases of supracondylar fractures of humerus in children, but it is a reliable method of treatment when the operation is delayed due to any reason or when C-arm is not available.
The lower of the two gradings, cosmetic factor and functional factor was taken in the overall grading.
Abbreviations:-CRPP- Closed reduction and percutaneous pinning; ORIF- Open reduction and internal fixation; MO- Myositis ossificans; TN- Trochlear necrosis; IN- Iatrogenic nerve injury.; CV- Cubitus varus.; SSI- Surgical site infection.
[1]. Mazzini JP, Martin JR, Esteban EMA, Surgical approaches for open reduction and pinning in severely displaced supracondylar humerus fractures in children: a systematic reviewJ Child Orthop 2010 4(2):143-52. [Google Scholar]
[2]. Loizou C, Simillis C, Hutchinson J, A systematic review of the early versus delayed treatment for Type III supracondylar humeral fractures in childrenInjury 2009 40(3):245-48. [Google Scholar]
[3]. Eren A, Güven M, Erol B, Cakar M, Delayed surgical treatment of supracondylar humerus fractures in children using a medial approachJ Child Orthop 2008 2(1):21-27. [Google Scholar]
[4]. Tiwari A, Kanojia RK, Kapoor SK, Surgical management for late presentation of supracondylar humeral fracture in childrenJ Orthop Surg (Hong Kong) 2007 15(2):177-82. [Google Scholar]
[5]. Yaokreh J, Odehouri-Koudou T, Tembely S, Dieth AG, Kouame B, Ouattara O, Delayed treatment of supracondylar elbow fractures in childrenOrthopaedics and Traumatology: Surgery & Research 2012 98(7):808-12. [Google Scholar]
[6]. Iyengar S, Hoffinger S, Townsend D, Early versus delayed reduction and pinning of Type 3 displaced supracondylar fractures of the humerus in children: A comparative studyJ Orthop Trauma 1999 13(1):51-55. [Google Scholar]
[7]. Mehlman CT, Strub WM, Roy DR, Wall EJ, Crawford AW, The effect of surgical timing on the perioperative complications of treatment of supracondylar humeral fractures in childrenJ Bone Joint Surg Am 2001 83:323-27. [Google Scholar]
[8]. Leet A, Frisancho J, Ebramzadeh E, Delayed treatment of Type 3 supracondylar humerus fractures in childrenJ Pediatr Orthop 2002 22(2):203-07. [Google Scholar]
[9]. Gupta N, Kay R, Leitch K, Femino JD, Tolo VT, Skaggs D, Effect of surgical delay on perioperative complications and need for open reduction in supracondylar humerus fractures in childrenJ Pediatr Orthop 2004 24:245-48. [Google Scholar]
[10]. Tahir A, Majid F, Ali MN, Qureshi MA, Treatment of old supracondylar fractures of humerus in childrenJ Surg Pakistan (International) 2012 17(4):135-38. [Google Scholar]
[11]. Gowda PM, Mohammed N, A study of supracondylar fractures of humerus in children by open reduction and internal fixation with Kirschner wiresIndian J Clin Pract 2014 25(6):572-76. [Google Scholar]
[12]. Hussain S, Ahmad M, Muzaffur T, Open reduction and internal fixation for displaced supracondylar fractures of the humerus in children with crossed K-wires via lateral approachChin J Traumatol 2014 17(3):130-35. [Google Scholar]
[13]. Sibly T, Briggs P, Gibson M, Supracondylar fractures of the humerus in childhood; range of movement following the posterior approach to open reductionInjury 1991 22(6):456-58. [Google Scholar]
[14]. Gartland JJ, Management of supracondylar fractures of the humerus in childrenSurg Gynecol Obstet 1959 109(2):145-54. [Google Scholar]
[15]. Flynn JC, Matthews SJG, Benoit RL, Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years ‘experience with long-term follow-upJ Bone Joint Surg Am 1974 56(2):263-72. [Google Scholar]
[16]. Walmsley PJ, Kelly MB, Robb JE, Annan IH, Porter D, Delay increases the need for open reduction of type III supracondylar fractures of the humerusJ Bone Joint Surg Br 2006 88(4):528-30. [Google Scholar]
[17]. Yildirim A, Unal V, Oken O, Gulcek M, Qzsular M, Ucaner A, Timing of surgical treatment for type III supracondylar humerus fractures in paediatric patientsJ Child Orthop 2009 3(4):265-69. [Google Scholar]
[18]. Gupta K, Gupta M, Kutty S, Displaced supracondylar fractures of the humerus in children: a modified technique of closed reductionIndian J Orthop 2006 40:108-10. [Google Scholar]
[19]. Kamath SU, Open reduction and internal fixation of severely displaced humeral supraconddylar fractures in childrenIndian J Orthop 2003 37:9 [Google Scholar]
[20]. Aslan A, Konya MN, Ozdemir A, Yorgancigil H, Maralcan G, Uysal E, Open reduction and pinning for the treatment of Gartland extension type III supracondylar humeral fractures in childrenStrategies Trauma Limb Reconstr 2014 9(2):79-88. [Google Scholar]
[21]. Khan RDA, Yousaf MN, Rehman MZ, Fareed MI, Yasin A, Outcome of open reduction internal fixation with cross K-wires for supracondylar fractures of humerus in terms of Flynn’s criteria in childrenJ Pak Med Assoc 2015 65(11):186-89. [Google Scholar]