Diabetes is among the most common chronic diseases in the world, with India being home to more than 65.1 million people with the disease [1,2]. Cardiovascular complication is one of the most common causes of morbidity and mortality in diabetic patients.
Studies show that diabetes is independently associated with development of heart failure. Increased myocardial vulnerability in diabetes along with other risk factors may be responsible for a distinct cardiomyopathy specific to diabetes, termed ‘diabetic cardiomyopathy’ [3].
Left Ventricular (LV) diastolic dysfunction may represent the earliest preclinical manifestation of diabetic cardiomyopathy before progressing to symptomatic heart failure [4]. Non-invasive assessment of LV function is quickly and routinely accomplished with echocardiography as a widely available bedside test. Recent studies have demonstrated up to 60% of asymptomatic, normotensive patients with type 2 diabetes have diastolic dysfunction when assessed by conventional echocardiography [5,6].
Multi-Detector-row Computed Tomography (MDCT) has been introduced as a cardiac imaging technique. Currently MDCT of heart is primarily used for detection of coronary obstruction and cardiac morphology. Since data acquisition in spiral MDCT is continuous, retrospective ECG gating allows for image reconstruction in any phase of the cardiac cycle. End-systolic and end-diastolic images can be produced to assess ventricular volumes. Global LV function parameters have been determined in good agreement with data obtained by catheter ventriculography, echocardiography and CMR in initial studies. The fast technical development of scanner hardware in the last few years has led to a rapid improvement of spatial and temporal resolution and significantly faster cardiac scans, which, as a consequence, have made coronary MDCT angiography a robust and accepted technique.
Few studies have shown good correlation of cardiac CT imaging for transmitral velocity, mitral septal tissue velocity, and estimation of LV filling pressures when compared with 2D echocardiography [7]. Present study was aimed to compare the two modalities in early diagnosis of diastolic dysfunction in asymptomatic diabetic subjects.
Materials and Methods
A total of 15 patients were selected for the study with diabetes without diabetic complications, hypertension, hyperlipidemia or features of coronary artery disease, all aged more than 25 years and less than 60 years. Detailed history and clinical examination (including fundoscopy by ophthalmologist) was done in all selected cases. Before undergoing 2D echocardiography and MDCT all the cases underwent following investigations: Complete Blood Counts (CBC), Renal Function Test (RFT), Liver Function Test (LFT), Fasting blood glucose level, HbA1c, Lipid profile, Serum electrolytes, Electrocardiogram (ECG) and Chest X-ray (PA view).
Asymptomatic, normotensive patients with type 2 diabetes were interviewed for possible participation in the clinical investigation. An arbitrary age limit of 60 years was established to avoid confounding effects of aging on LV diastolic function. All patients were asymptomatic without any history of hypertension, coronary artery disease, valvular heart disease, or congestive heart failure. For enrollment in the study, the arterial blood pressures measured in the sitting posture on separate occasions were to be consistently <130/85mmHg (Joint National Committee VIII Guidelines). Patients taking antihypertensive medications were excluded. The patients’ diabetes management included diet, oral hypoglycaemic agents, and/or insulin. Unless there was either a normal cardiac catheterization or a negative stress imaging test within the previous year, all subjects with evidence of LV diastolic dysfunction based on the echocardiogram underwent maximal exercise stress echocardiography.
Echocardiography: All studies were performed with commercially available digital platforms. Standard 2-dimensional and colour flow doppler images were obtained in all patients in the parasternal short-axis and apical views. Each patient underwent LV diastolic function assessment by conventional doppler in conjunction with the Valsalva maneuver and Tissue Doppler Imaging (TDI). LV ejection fraction was calculated using the modified Simpson’s or bullet method techniques; LV mass was determined by the area-length method.
Stress Echocardiography: Exercise or dobutamine stress echocardiography was performed and segmental LV wall motion was assessed using the standard 16-segment model.
Conventional Doppler Measurements: Blood flow velocity was recorded at the mitral inflow as well as at the entrance of the pulmonary veins into the left atrium. The following velocities and times were recorded: Early ventricular filling (E), flow related to atrial contraction (A), Deceleration Time (DT), Isovolumic Relaxation Time (IVRT), E/A ratio. Measurements were averaged from 3 end-expiratory cycles at a sweep of 100mm/s.
Valsalva Maneuver: As diastolic dysfunction progresses and left atrial pressure increases, the impaired relaxation pattern in the mitral inflow velocities in patients with an E/A ratio progresses to a pseudonormalized pattern that resembles a normal conventional doppler mitral inflow. The purpose of performing the Valsalva maneuver is to abruptly and transiently reduce LV preload by reducing left atrial pressure, thereby causing the mitral inflow pattern to revert to an E/A ratio ≤1. There are limitations with regard to the Valsalva maneuver; however, previous studies have shown that there is a significant elevation in LV end-diastolic pressure when there are large changes in the E/A ratio provoked by the Valsalva maneuver compared with baseline. Therefore, diastolic dysfunction was considered present in the current study if the change in the E/A ratio was ≥40% from baseline after the Valsalva maneuver. The Valsalva maneuver was performed by instructing subjects to forcibly exhale against a closed glottis after deep inspiration.
Mitral inflow measurements (E and A) were obtained during phase II (straining) of the Valsalva maneuver. The maneuver was considered valid only if there was a 10% decrease in E velocity compared with baseline.
Tissue Doppler Imaging: Assessment of early diastolic mitral annular velocity was performed by pulsed wave TDI of both the septal and lateral walls in the apical 4-chamber view. Doppler echocardiograms were recorded at a sweep of 50mm/s; the mean value of 3 cardiac cycles was obtained. Diastolic LV dysfunction was considered present if both septal and lateral walls were ≥8 cm/s.
Criteria for the Diagnosis of Diastolic Dysfunction: As previously described, we assessed diastolic function by 4 different echocardiographic approaches: conventional doppler, the effects of the Valsalva maneuver on transmitral flow velocities and TDI. Each one of these approaches has been independently validated for the diagnosis of diastolic dysfunction. If there was a diastolic abnormality present with any of these approaches, the patient was considered to have diastolic dysfunction. Criteria for the patient echocardiographic approaches used to determine the presence of LV diastolic dysfunction and enrollment of patients in the present study are summarized in [Table/Fig-1].
Echocardiographic diastolic parameters used in the study.
| Early peak transmitral velocity (E) |
| Peak transmitral velocity at atrial systole (A) |
| Mitral E/A ratio |
| Annular tissue Doppler velocity at any site (cm/s) |
Multidetector CT: MDCT imaging was performed with a 64-slice scanner. Before imaging, patients were monitored for blood pressure and heart rate. Metoprolol 50 to 100mg orally was given to patients with heart rate >65 beats/min.
Our 64-slice MDCT divided each cardiac cycle into 10 phases by retrospective ECG-gating and LV volume and LV length were calculated for each phase of cardiac cycle. This LV volume was plotted against time.
Then, we calculated the difference in LV volume for each consecutive phase per second, which was again plotted against time. This graph gave us the value of early peak transmitral velocity (E) and late peak transmitral velocity (A). These values were divided with respective transmitral area in E phase and A phase which gave us values of E and A comparable to 2D echocardiography. By the ratio of E and A (E/A) we calculated diastolic dysfunction as mentioned above.
Likewise, we plotted a graph of LV length v/s time. We then plotted change in LV length per second v/s time. This graph gave us the value of Ea. By calculating E/Ea we could estimate diastolic dysfunction as mentioned above.
For evaluation of the accuracy of 2D echocardiography and MDCT to detect diastolic dysfunction, diastolic function was graded in 4 categories using the following criteria:
1) Normal diastolic function (≥ 1 E/A <2 and E/Ea≤ 8);
2) Impaired relaxation pattern (diastolic dysfunction grade I; E/A <1 and E/Ea≤ 8);
3) Pseudo normal pattern (diastolic dysfunction grade II; ≥ 1 E/A <2 and ≥ 9 E/Ea ≤ 12); and
4) Restrictive filling pattern (diastolic dysfunction grade III; E/A ≥ 2 and E/Ea ≥ 13).
Results
A total of 15 diabetic patients were included in the study. There were 8 males and 7 females. The mean age was 48.20 years. The baseline characteristics of these patients are shown in [Table/Fig-2].
Baseline characteristics of diabetic cases.
| Characteristics | Diabetics (n=15) |
|---|
| Age | 48.20 ± 9.283 |
| Pulse rate (/min) | 71.33 ± 5.473 |
| SBP (mmHg) | 116.53 ± 11.963 |
| DBP (mmHg) | 70.53 ± 5.041 |
| BMI (kg/m2) | 21.120 ± 1.063 |
| Hb (g/dL) | 12.90 ± 2.12 |
| Creatinine (md/dl) | 0.94 ± 0.22 |
| FBS (mg/dl) | 124.73 ± 38.54 |
| HbA1c (%) | 9.53 ± 1.98 |
| Triglycerides | 120.13 ± 28.46 |
| LDL | 71.67 ± 29.79 |
| HDL | 57.00 ± 10.98 |
| Total cholesterol | 139.27 ± 31.18 |
The diastolic dysfunction in study population as detected by echocardiography and MDCT is shown in [Table/Fig-3]. Total 73.3% people had diastolic dysfunction either on echocardiography or MDCT which ranged from grade I to grade II diastolic dysfunction. None had grade III diastolic dysfunction.
Diastolic dysfunction as detected by echocardiography vs MDCT.
| Diastolic Dysfunction (Grade) | Echoardiography (n=15) | MDCT (n=15) |
|---|
| Normal | 4 (26.7%) | 4 (26.7%) |
| Grade I DD | 10 (66.67%) | 10 (66.67%) |
| Grade II DD | 1 (6.67%) | 1(6.67%) |
| Diastolic Dysfuntion | 11 (73.3) | 11 (73.3%) |
| Total | 15 (100%) | 15 (100%) |
The various parameters used for assessing diastolic dysfunction in these patients were studied individually by either echocardiography or MDCT. The [Table/Fig-4] shows that peak transmitral velocity in early diastole (E) values show significant difference between echocardiography and MDCT. This may be explained by the systemic underestimation of E by MDCT due to sampling rate as demonstrated by previous studies [7]. Other diastolic parameters are not significantly different by the two modalities.
Diastolic function parameters for echocardiography and MDCT.
| Diastolic Parameters | Echocardiography (mean ± SD) | MDCT (mean ± SD) | t-value | p-value |
|---|
| E | 71.10 ± 19.17 | 68.47 ± 18.85 | 4.27 | 0.001 |
| A | 76.10 ± 20.07 | 75.58 ± 20.99 | 1.86 | 0.112 |
| E/A | 1.00 ± 0.36 | 1.02 ± 0.41 | -1.23 | 0.236 |
| Ea | 9.95 ± 2.09 | 9.83 ± 2.14 | 1.04 | 0.314 |
| E/Ea | 7.25 ± 1.72 | 7.22 ± 1.72 | 1.256 | 0.247 |
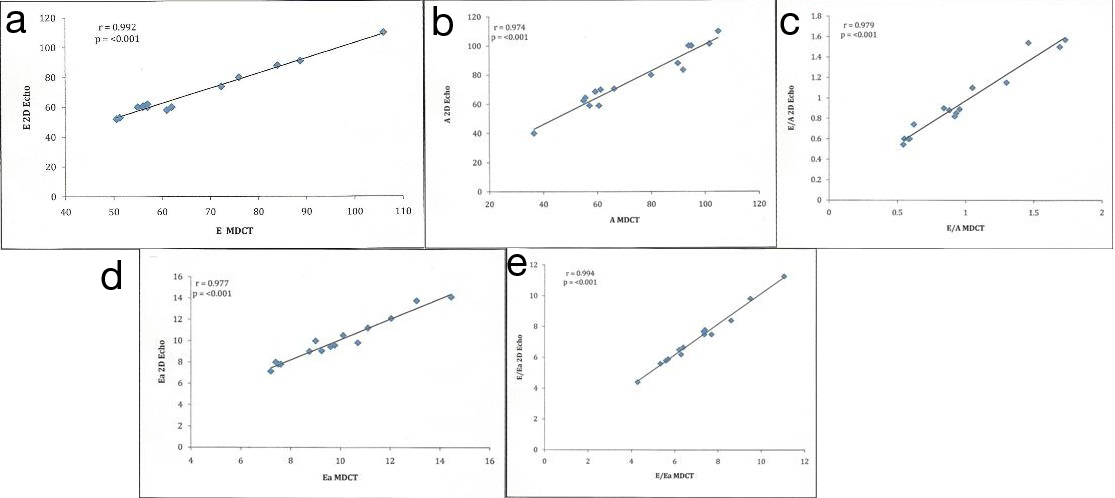
[Table/Fig-5] Shows the correlation between diastolic parameters of echocardiography and MDCT in the diabetic patients. All the diastolic parameters have good correlation between echocardiography and MDCT in these patients.
Correlation between cardiac CT and 2D echocardiography for assessment of E (r = 0.992; p < 0.001), A (r = 0.974, p < 0.001), E/A (r = 0.979; p < 0.01), Ea (r = 0.977; p < 0.001), and E/Ea (r = 0.994; p < 0.001)
Discussion
The present study was conducted for early diagnosis of diastolic dysfunction in asymptomatic diabetic patients. Doppler echocardiography represents the most commonly used approach for evaluation of diastolic function. Cardiac Computed Tomography (CT) is an important non-invasive imaging modality for the evaluation of coronary atherosclerosis. Multiphase CT can also be used for LV systolic function analysis. However, very little information is available on the feasibility of cardiac CT imaging to assess diastolic LV function especially in diabetic patients.
The present study was undertaken to evaluate the feasibility of cardiac CT for assessment of diastolic function in a direct comparison with 2D echocardiography using TDI in diabetic subpopulation.
The prevalence of LV diastolic dysfunction in asymptomatic, normotensive patients with type 2 diabetes mellitus without evidence of coronary heart disease in our study was significantly high. A previous study using conventional doppler performed in normotensive patients with type 2 diabetes suggested a prevalence of diastolic dysfunction of 30% [8]. This may have represented as an underestimation, because diagnosing diastolic dysfunction by conventional doppler is limited in the setting of elevated LV end-diastolic pressure and an apparently normal transmitral flow velocity spectral doppler pattern.
Thus, we can expand the diagnostic armamentarium of cardiac ultrasound by using TDI and the response of conventional doppler parameters to the Valsalva maneuvre to determine occult diastolic dysfunction at an earlier preclinical stage in normotensive asymptomatic type 2 diabetics. This has been confirmed in earlier studies also [9]. In one study diastolic dysfunction was found in 43 of 57 patients (75%) when these echocardiographic techniques were used [10].
In diabetic patients, for 2D echocardiography and MDCT we found good correlation between peak transmitral velocity in early diastole (E) (Correlation coefficient r=0.992, p-value<0.001). Similarly, there was also good correlation between peak transmitral velocity in atrial systole (A) (Correlation coefficient r=0.974, p-value<0.001), E/A ((Correlation coefficient r=0.979, p-value<0.001), early peak transmitral septal velocity (Correlation coefficient r=0.977, p-value<0.001) and E/Ea (Correlation coefficient r=0.994, p-value<0.001).
Hence, all diastolic parameters measured had good correlation between 2D echocardiography and MDCT for diabetic subpopulation.
Thus, we can conclude that our study showed good correlation between diastolic parameters of 2D echocardiography and MDCT for diabetic patients which was statistically proven so that diastolic dysfunction as measured by 2D echocardiography and MDCT are comparable and MDCT seems feasible for measurement of diastolic function. Boogers et al., who evaluated 70 patients with cardiac CT imaging also showed good correlations of diastolic parameters with 2D echocardiography [7].
This represents an important finding because the assessment of diastolic dysfunction provides important diagnostic, therapeutic, and prognostic information in patients with cardiovascular disease. Additionally, it has been shown that normotensive, asymptomatic patients with diabetes and normal LV systolic may already exhibit diastolic dysfunction. Accordingly, additional post processing for diastolic dysfunction may have the potential to enhance the clinical evaluation derived from cardiac CT. Moreover, the feasibility of cardiac CT for assessment of diastolic function is of particular interest because of recognition of diastolic dysfunction as the earliest event in the pathogenesis of diabetic cardiomyopathy and the importance of heart failure with normal ejection fraction.
Limitation
A major limitation of our study is low sample size. Additionally, transmitral velocity may be influenced by other parameters that could influence transmitral velocity measurements, including filling pressures, degree of LV relaxation, and myocardial elastic recoil and stiffness. For overcoming these limitations, additional measurements have been proposed, including the evaluation of pulmonary venous velocity and M-mode echocardiography flow velocity curves. In the current study, however, these measurements were not performed.
Multiphase CT datasets acquired in this study for measurement of diastolic function indexes were without tube current modulation. Its impact on diastolic function parameters needs to be further studied.
Conclusion
In conclusion, there is a high prevalence of LV diastolic dysfunction with preserved systolic function in cardiac-asymptomatic diabetic patients and MDCT can be used for assessment of LV diastolic function in patients with diabetes.