Papillary lesions comprise of a distinct spectrum of breast lesions and their diagnosis continues to be a challenge due to their heterozygosity in morphology with benign, atypical and malignant subtypes. There is limited data in the literature that discusses their clinical presentation, detailed histopathological features including the presence of atypia or associated ductal carcinoma in situ and prognosis [1]. These lesions, even though rare compared to ductal carcinomas of breast, behave differently and the surgery plays a pivotal role. Papillary carcinoma arising from and restricted to a cystically dilated duct can be excised completely, whereas, benign papillomatosis that involves numerous branches of a duct have high rate of recurrence and also have high incidence of malignant transformation due to incomplete excision. These features are a serious impediment to the outcome based classification [2]. This study aimed at discussing the diagnostic difficulties of papillary lesions along with presence and absence of few critical histopathological findings. The objectives of the study were to analyse the different histopathological findings, both epithelial and stromal, in various papillary lesions and to identify those histopathological findings that can differentiate between benign, atypical and malignant papillary lesions. Immunohistochemical analysis was also conducted for myoepithelial cells, that aided in identifying benign, atypical and malignant papillary lesions and in analysis of hormonal and Her2neu status in all malignant cases.
Materials and Methods
A retrospective and prospective study of 34 papillary lesions of breast was conducted from January 2009 to December 2015 in the Department of Pathology of a tertiary health care hospital. Breast core biopsy specimens were excluded from the study and only those cases which fulfilled the definition of papillary lesions were included [1]. The clinical history and radiological findings were retrieved from medical archives. Macroscopic findings were noted and microscopic findings were reviewed. While reviewing, importance was given to histopathological findings such as type of lesion whether infiltrating or non-infiltrating, presence of papillary pattern, architectural complexity, presence of fibrovascular core, whether broad and sclerotic or thin and arborizing fibrovascular cores, associated benign changes in the adjacent breast tissue such as epithelial hyperplasia, fibrocystic disease, epithelial hyperplasia, adenosis, fibroadenomatous hyperplasia, sclerosis, xanthogranulomatous inflammation and columnar cell lesions. In addition, in all malignant lesions, the grade and stage of the tumour were also recorded. The malignant lesions were graded into low grade or high grade. The lesions were classified according to WHO classification of papillary lesions using 2003 WHO pathology and genetics of tumours of the breast and female genital organs [2].
Further, Immunohistochemical (IHC) staining was performed to know the hormonal and Her2neu status in all malignant cases. The immunohistochemical results of hormonal status were evaluated using Allred scoring system which takes into consideration of proportion of cells showing positivity and the intensity of staining [Table/Fig-1] [3]. Her2neu staining interpretation was done as per ASCO 2013 guidelines [4]. The tumours with an Allred score of ≤ 2 were diagnosed as negative, and with > 2 score as positive.
Allred scoring system for ER and PR immunostaining [3].
| Proportion score | Observation | Intensity score | Observation |
|---|
| 0 | None | 0 | None |
| 1 | 1% | 1 | Weak |
| 2 | 1-10% | 2 | Intermediate |
| 3 | 10-33% | 3 | Strong |
| 4 | 33-66% | | |
| 5 | 66-100% | | |
Sum of proportion score and Intensity score:
Total score of 0-2 = Negative;
Total score of 3-8 = Positive
Various histopathological features were analysed for their frequency and were compared with the final diagnosis using cross tabs and Chi-square value (χ2) with one degree freedom, wherever appropriate. A p-value of <0.05 was considered significant for all the performed tests. All tabulations and statistical analysis was done using IBM SPSS 20.0 data software.
Results
A total of 34 cases of papillary lesions were seen during the study period. The mean age of the patients was 58 years (age range: 16-72 years). The central quadrant was the most common location (66.6% cases). The most common presenting complaint was lump (76.5% cases), followed by nipple discharge (29.4% cases), mastalgia (11.8% cases) and heaviness in the breast (5.9% cases). Twenty eight cases (82.4%) presented as solitary lesion while two were multifocal. Further, these lesions were categorized into benign, atypical and malignant [Table/Fig-2].
Distribution of papillary lesions of the breast.
| Type of papillary lesions | Number of cases | Percentage of cases |
|---|
| Benign1. Intraductal papilloma- Solitary2. Intraductal Papillomatosis | 141301 | 41.2%38.2%2.9% |
| Atypical1. Intraductal papilloma with atypical hyperplasia a. Solitary b. Atypical Papillomatosis2. Intraductal papilloma with ductal carcinoma in situ | 0602010104 | 17.6%5.9%2.9%2.9%11.8% |
| Malignant1. Intraductal papillary carcinoma a. Intracystic papillary carcinoma b. Solid intraductal papillary carcinoma c. Micropapillary intraductal carcinoma2. Invasive papillary carcinoma3. Invasive micropapillary carcinoma | 14050301010504 | 41.2%14.7%8.8%2.9%2.9%14.7%11.8% |
Papillary lesions were categorized on the basis of fibrovascular cores as broad sclerotic type or the thin arborizing type. In 92.9% cases of benign lesions, broad sclerotic fibroepithelial cores were observed and the remaining 7.1% of cases had a thin arborizing fibrovascular core. In comparison, 83.3% of atypical and 100% of malignant lesions predominantly showed thin, arborizing fibrovascular cores.
We observed a higher degree of association of epithelial proliferation and architectural complexity in atypical (66-100% cases) and malignant lesions (70-100% cases) compared to benign tumours (10-15% cases). However, the atypical lesions showed the complex architectural pattern involving only a portion of the tumour compared to the malignant lesions that had a wide complex architecture involving most or all of the lesion. A solid pattern of epithelial growth was observed in 71.4% cases of malignant lesions. The histopathological findings associated with papillary lesions are tabulated in [Table/Fig-3].
Histopathological findings of papillary lesions of the breast.
| Histopathological findings | BenignNumber (%) | AtypicalNumber (%) | MalignantNumber (%) |
|---|
| Fibrovascular cores | Broad | 13 (38.2%) | 02 (5.9%) | 00 |
| Thin | 01 (2.9%) | 04 (11.8%) | 14 (41.2%) |
| Location | Central | 13 (38.2%) | 04 (11.8%) | 10 (29.4%) |
| Peripheral | 01 (2.9%) | 02 (5.9%) | 04 (11.8%) |
| Number | Solitary | 13 (38.2%) | 04 (11.8%) | 09 (26.5%) |
| Multifocal | 01 (2.9%) | 02 (5.9%) | 05 (14.7%) |
| Solid pattern | 00 | 00 | 10 (29.4%) |
| Epithelial changes:1. Fibrocystic disease2. Adenosis3. Epitheliosis4. Epithelial hyperplasia, usual type5. Sclerosing adenosis6. Fibroadenomatous hyperplasia7. Columnar lesions | 08 (23.5%)05 (14.7%)04 (11.8%)02 (5.9%)02 (5.9%)01 (2.9%)13 (38.2%) | 06 (17.6%)06 (17.6%)06 (17.6%)06 (17.6%)NilNil04 | 14 (41.2%)08 (23.5%)09 (26.5%)14 (41.2%)07 (20.6%)03 (8.8%)14 (41.2%) |
| Stromal changes:1. Fibrosis2. Hyalinization3. Sclerosis4. Myxoid5. Xanthogranulomatous 6. Haemorrhagic Infarction | 07 (20.6%)05 (14.7%)04 (11.8%)01 (2.9%)08 (23.5%)04 (11.8%) | Nil05 (14.7%)06 (17.6%)Nil05 (14.7%)Nil | 13 (38.2%)14 (41.2%)14 (41.2%)06 (17.6%)08 (23.5%)04 (11.8%) |
The most common papillary lesion accounting for 43% of the cases was intraductal papilloma. This benign tumour was usually solitary and was mostly well circumscribed nodular lesion that was located more commonly in the subareolar region. Intraductal papillomas exhibited various types of metaplasias most common being apocrine (30.8%) followed by squamous (23.1%), mucinous (15.4%) and clear cell (7.7%) types. Papillomas had broad sclerotic fibrovascular core [Table/Fig-4a-c]. In 23.1% cases, there was a suspicion of invasion and hence p63 was used to identify myoepithelial cells, which was strongly positive in the suspicious areas [Table/Fig-5a-c]. A single case of papillomatosis was encountered in a 51-year-old female. Histopathological findings were similar to intraductal papilloma, but the attachment to the duct wall was discerned only focally.
An isolated case of solitary intraductal papilloma with atypical hyperplasia was seen in a 29-year-old female that displayed focal proliferations of a mildly atypical, uniform cell population.
Intraductal papilloma with ductal carcinoma in situ constituted for 11.8% of cases. There was more than 90% involvement of the lesion with intermediate (50% cases) to high (50% cases) nuclear grade. The lesions were moderately differentiated [Table/Fig-4d-f].
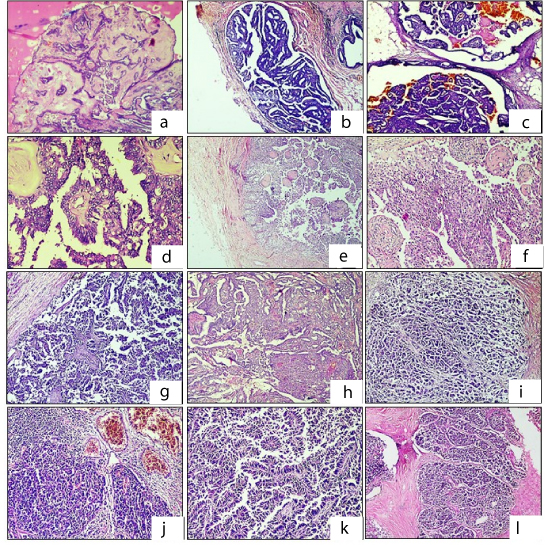
Histopathological findings in various papillary lesions of the breast:
a-c: Intraductal papilloma: A: Benign papilloma exhibiting broad sclerotic fibrovascular cores. [H&E; x100] b,c: Cystic spaces with tumour composed of papillary fronds. (H&E; x40)
d-f: Intraductal Papilloma with DCIS: Almost 30% of the entire lesion shows proliferation of a uniform cell population with ductal carcinoma in situ. (d:H&E; x200, e:H&E;x40, f:H&E;x100)
g: Micropapillary Carcinoma: Tumour cells in micropapillary pattern lacking true fibrovascular cores. (H&E; x100)
h-j: Invasive papillary carcinoma: The papillary lesion with a solid proliferation (H). [h: H&E;x100, i: H&E;x200, j: H&E,x40]
k,l: Intracystic Papillary carcinoma: Tumour composed of arborizing papillary fronds projecting into the lumen with absence of myoepithelial cells. [k,l: H&E;x200]
Immunohistochemical analysis of papillary lesions of the breast:
a-c: P63 staining in papillary lesions: a= Intraductal papilloma with continuous myoepithelial cells showing p63 positivity (IHC; x400), b = Atypical Papilloma with discontinuous myoepithelial cells showing p63 positivity (IHC; x100), c = Papillary carcinoma with absent myoepithelial cells showing p63 negativity (IHC; x100)
d-f: ER, PR and Her2neu staining in papillary carcinoma: d =ER Positivity (IHC; x200), e: PR positivity (IHC; x40), f: Her2neu negativity (IHC; x40)

Four cases of invasive micropapillary carcinoma with age of presentation ranging from 30-65 years were seen. The average mitosis was 5/10HPF. The histological grade of 1 and 2 constituted for 50% cases each [Table/Fig-4g].
Intraductal papillary carcinomas and invasive papillary carcinoma comprising of 5 cases each accounted for 16.6% of total number of cases respectively [Table/Fig-4h-j]. The age of presentation of these lesions was 29-62 years. Apocrine metaplasia was noted along with associated lesions like microcalcification, hyalinization, atypical ductal hyperplasia and necrosis. The mitoses ranged from rare to 7/10 HPF. The histological grade was Grade 2 in all intraductal carcinomas.
Intracystic papillary carcinoma also called as encapsulated papillary carcinoma is a variant of intraductal papillary carcinoma. These lesions exhibit cystic spaces that surrounds papillary proliferation and lie within a dilated duct [Table/Fig-4k,l].
The age of presentation of invasive papillary carcinoma ranged from 43-73 years with the average tumour size of 6.2x5x3cm. Mitoses was frequent (10-12mitoses/10HPF). Lymphovascular and perineural invasion were noted in all cases. The histologic grade were Grade 1 in 40%, Grade 2 in 20% and Grade 3 in 40% cases. They were found strongly positive for hormonal receptors and negative for Her2neu marker on immunostaining [Table/Fig-5d-f].
On statistical analysis the variables such as age, location, laterality, focality, epithelial change, stromal change, nuclear pleomorphism and presence or absence of broad sclerotic fibrovascular cores, only nuclear pleomorphism and presence or absence of broad sclerotic fibrovascular cores were found to be statistically significant with a p-value of <0.05. These two variables were also considered the reliable parameters on histopathology review of the slides.
Discussion
Papillary lesions of the breast include different entities based on clinical and morphological evaluation [5]. They are defined as those lesions of the breast that are characterized by the presence of papillary, arborizing epithelial proliferation that are supported by fibrovascular stalks with or without an intervening myoepithelial layer [1]. The diagnosis of precise type of papillary lesion continues to be one of the most challenging aspects. Identification of whether the lesion is benign or malignant has a great impact on therapy [1]. In this study, the diagnostic issues in various types of papillary lesions encountered in our hospital are discussed.
Intraductal papillomas are the most common type of papillary lesions and presents as solitary lesions in the subareloar region in most of the cases [5,6]. The most common clinical finding is the presence of palpable mass followed by presence of nipple discharge that can be either bloody, serous or serosanguinous in nature [7]. The diagnosis is usually straight forward with lesion characterized by arborizing papillae exhibiting fibrovascular stalks that are covered by myoepithelial cells [8]. In cases with florid epithelial hyperplasia or atypical ductal hyperplasia the diagnosis is difficult as these findings obscure the papillary nature of the lesion [1]. But, generally these changes are focal. Stromal changes such as diffuse sclerosis can also create confusion mimicking invasion. These papillomas are usually subjected to various morphological changes such as torsion with secondary haemorrhagic infarction of the papillae [5]. We encountered various epithelial and stromal changes like columnar cell change, fibrocystic disease, adenosis, epitheliosis, fibrosis, hyalinization, xanthogranulomatous inflammation, sclerosis and haemorrhagic infarction. In difficult cases, immunohistochemistry for identifying the myoepithelial cells proves the benign nature of these lesions [1].
Multiple papillomas or papillomatosis is a disease of younger age group when compared to papilloma. Multiple papillomas most commonly affect the peripheral terminal duct-lobular units or distal portions of the terminal ducts unlike their solitary counterpart that affects almost always central ducts [7,9]. The morphology of papillomatosis is similar to that seen in intraductal papillomas. Ueng et al., describes that papillomatosis generally have focal attachment to the duct wall [1]. However, there is enough evidence of multiple points of attachment of several papillae in papillomatosis [1,9]. WHO states the term papillomatosis is confusing and should be avoided as this term has also been used for usual ductal hyperplasia and multiple papillomas [8].
Most of the benign papillary lesions pose less diagnostic problems. Diagnosis of low grade papillary lesions such as intraductal papilloma with atypical hyperplasia or papillomas with Ductal Carcinoma Insitu (DCIS) also termed as atypical papilloma requires expertise [8]. Atypical ductal papilloma are defined as presence of a focal proliferation of atypical epithelial cells with low nuclear grade (WHO). Ueng et al., termed such lesions as low grade Ductal Intraepithelial Neoplasia (DIN) and described that these changes are seen only focally [1]. Different authors use different terminologies and criterias to identify these lesions [1,10,11]. Page et al., termed a lesion as papilloma with DCIS when it had morphology similar to non-comedo DCIS with a size greater than 3mm [10]. However, the same authors term those papillomas that are more than 3mm in size with epithelial proliferation as papillomas with atypia. In contrast, Collins et al., stated that the extent or the size of atypical epithelial proliferation in the lesion is not required for diagnosis of atypical papillomas [12]. However, the diagnosis is made when there is morphological evidence such as architectural and cytological features of atypical proliferation in these lesions [12,13].
Atypical papillomas exhibit decreased number of myoepithelial cells that can be proved by immunohistochemistry. The management of both intraductal papilloma with atypical hyperplasia and papilloma with DCIS is by complete excision and a stringent follow-up.
Intraductal papillary carcinomas are rare and accounts for 2% of all breast cancers [14]. Intraductal papillary carcinomas affect women in their fifth and sixth decade of life [14]. Intraductal carcinoma is distinguished by other types of intraductal carcinoma by the presence of a fibrovascular stalk of the lesion [15]. Morphologically, these lesions are similar to DIN and show near complete or complete absence of myoepithelial cells in the papillae [1].
Papillary carcinomas as described above are generally non-invasive. However, some papillary carcinomas can have stromal invasion that displays morphological features of infiltrating ductal carcinoma [1]. The invasive nests can be either micro-invasive or grossly evident [16]. Invasive papillary carcinoma accounts for less than 2% of all the breast cancers [16].
Invasive Micropapillary Carcinoma (IMPC) is an aggressive yet rare form of breast cancer with a very high rate of lymph node metastasis. It is characterized by micropapillary clusters of neoplastic cells lacking true, central, fibrovascular cores and lying within fairly prominent clear empty stromal lacunae [1]. These tumours are of higher grade and exhibit higher nuclear pleomorphism. Often they show lymphocytic infiltration along with inverse polarity of tumour cell clusters with exposed basal layer. Foci of intraductal carcinoma are seen almost in all cases of micropapillary carcinoma [17]. This should not be confused with micropapillary DCIS; wherein the ducts are dilated and lined by very small tumour cells. Micropapillary DCIS is often multifocal and multicentric in contrast to IPMC which often presents as palpable mass.
Myoepithelial cell continuity was noted in all the benign papillary lesions. In atypical papillomas and intraductal carcinoma with DCIS cases, there was a definite reduction in the myoepithelial cells, whereas in malignant lesions, there was complete absence of the myoepithelial cells. Morphology of the papillae differed in benign, atypical and malignant lesions. The papillae had broad and sclerotic fibrovascular cores in benign lesions, thin and arborizing fibrovascular cores in most of the atypical lesions and all malignant cases had typical thin, arborizing fibrovascular cores. This morphological difference was of great help in most of the difficult cases to arrive at the diagnosis and was found statistically significant (p-value <0.05). Similar findings were also described by Pathmanathan et al., [18].
Limitation
An important gap in the literature related to papillary lesions of the breast is the lack of universality in classifying the various lesions. This is due to use of various terminologies and criteria to categorize them. To the best of our knowledge, we have incorporated WHO classification to define these lesions, however, the classification is limited by certain overlapping features. The category of intraductal papilloma with atypical hyperplasia and intraductal papilloma with ductal carcinoma in situ has also been classified as papilloma with ductal carcinoma in situ (DIN 1-3) in published literature. 1 Other limitations of the present study were the small size of population and lack of follow up. Larger studies and a stringent follow up especially in those cases where only lesional excisions were performed may throw a better insight into the various prognostic factors of papillary lesions.
Conclusion
To conclude, diagnosis of papillary lesions of the breast is challenging due to its varied clinical, radiological and pathological features that has direct impact on management. The continuity of myoepithelial layer and presence of broad and sclerotic fibrovascular cores are consistent features in benign papillary lesions.
Sum of proportion score and Intensity score:Total score of 0-2 = Negative;Total score of 3-8 = Positive