Multiple Meningioma in a Patient of Bipolar Disorder: The Dilemma of Detecting Structural Brain Lesions in the Backdrop of a Long Standing Psychiatric Illness
Ananya Mahapatra1, Mamta Sood2, Sudhir Kumar Khandelwal3
1 Senior Resident, Department of Psychiatry, All India Institute of Medical Sciences, New Delhi, India.
2 Associate Professor, Department of Psychiatry, All India Institute of Medical Sciences, New Delhi, India.
3 Professor and Head, Department of Psychiatry, All India Institute of Medical Sciences, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ananya Mahapatra, Department of Psychiatry, 4th Floor, Teaching Block, All India Institute of Medical Sciences, Ansari Nagar, East, New Delhi-110029, India.
E-mail: nnyaa09@gmail.com
Multiple meningioma often can be clinically silent and may present with only psychiatric symptoms. We report a case of 43-year-old, right handed woman with a 23 year history of long standing bipolar affective disorder, who presented with a mixed episode with psychotic symptoms which did not respond to usual treatment and was further complicated with a different set of symptomatology. MRI brain revealed multiple dural based mass lesions identified to be multiple meningiomas. Patient’s symptoms improved after gamma knife stereotactic radiosurgery for the multiple meningioma. Our finding illustrates the need to assess for brain lesions in presence of atypical symptoms, along with unresponsiveness to traditional management with psychotropic medications in patients with bipolar affective disorders.
Psychiatric symptoms, Psychotropic medications, Stereotactic radiosurgery
Case Report
We report the case of a 43-year-old right handed woman, suffering from bipolar disorder for 23 years. She presented with an acute episode of 25 days, characterized by decreased need for sleep, irritability, anger outbursts, decreased concentration, preoccupation with adverse life events like marital separation, expression of hopelessness and crying spells, over religiosity, authoritative behaviour, auditory hallucinations second person type, decreased appetite and impaired self-care with severe socio-occupational dysfunction. She had a past history of an episodic illness characterized by five manic and three depressive episodes with psychotic symptoms. There was a family history of similar illness in paternal aunt and psychotic illness in maternal uncle. She was maintaining well on Tab lithium carbonate 900mg/day prior to the current episode. For the current episode, a provisional diagnosis of bipolar affective disorder, current episode with psychotic symptoms (ICD 10) was considered.
The psychopathological severity rating scales at the time of diagnosis scored HDRS=22 (Hamilton Depression Rating Scale), YMRS=14 (Young Mania Rating Scale), and CGI-S=6 (Clinical Global Impression Severity). This was indicative of presence of severe depressive and manic symptoms. She was treated with quetiapine 800mg followed by haloperidol 20mg in combination with Lithium carbonate 900mg respectively, over 12 weeks. Although her serum lithium level was adequate, she showed minimal improvement on either combination. Subsequently, these medications were cross tapered with carbamazepine 600mg and amisulpiride 600mg. However, during this period she developed a completely different set of symptoms characterized by agitation, frequent crying spells, incoherent speech, disorientation to time, place and person, disorganised and disinhibited behaviour in the form of crawling under the bed, rolling on floor and disrobing herself in front of others. She had unprovoked anger outbursts and was uncooperative for interview. Patient was treated with propranolol up to 80mg for possibility of akathisia, without any improvement. Subsequently, all psychotropic medications were stopped and the patient was investigated for delirium. Her routine investigations (haemogram, serum electrolytes, renal and liver function tests, ECG, Chest X ray) were within normal limits and serum CPK was 112 IU. There were no complaints of headache, seizures, urinary/fecal incontinence or any signs suggesting neurological deficit.
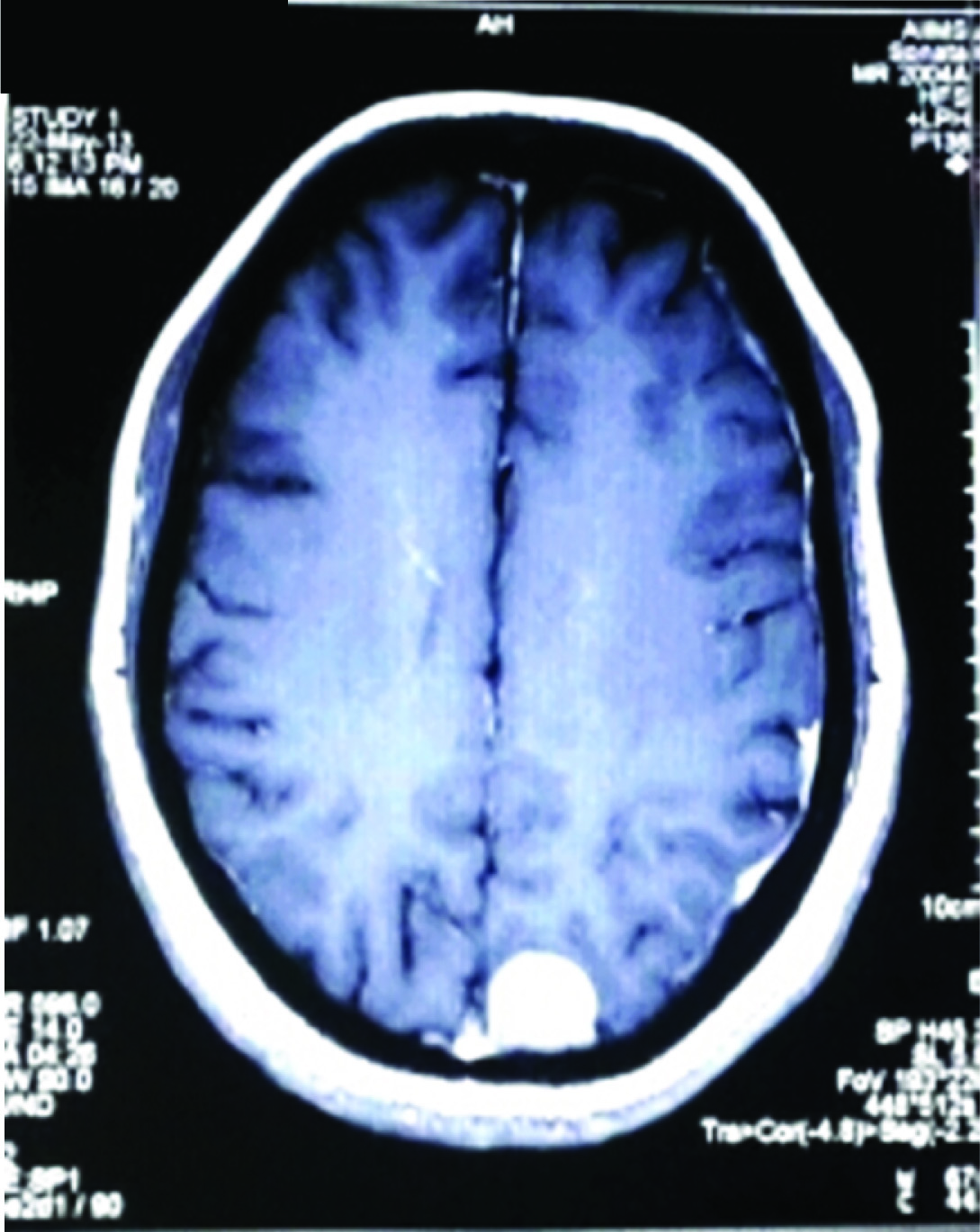
Contrast MRI of brain revealed multiple dural based mass lesions in the right fronto-parietal, temporal, and occipital regions and along the falx in the anterior interhemispheric fissure and right petrous region with buckling of adjacent cortex and peri-tumoural edema, identified as multiple meningiomas [Table/Fig-1,2]. The patient underwent gamma knife stereotactic radiosurgery following neurosurgery review. Six tumours ranging from 1.19–9.8 cc were selected and each received >=12 Gy of radiation. Patient’s restlessness, agitation and disorganized behaviour improved within a week following radiosurgery and her speech became comprehensible. Carbamazepine was restarted and optimized to 800 mg with serum levels of 10.9 ng/ml. However after patient became more communicative, she started reporting seeing her husband and his family members, in their absence. Hallucinatory behaviour was also observed in the ward. However, she would not elaborate regarding the same. Tab aripiprazole 10mg was added suspecting visual hallucinations, after which this symptom significantly improved and completely resolved over next five months. Six months post-surgery, repeat MRI brain revealed no increase in the size of the residual tumours. After maintaining well for eight months, patient developed a severe depressive episode characterized by low mood, anhedonia, fatigability, psychomotor retardation, hopelessness, crying spells and suicidal ideations. However no atypical symptoms were observed in this episode. Tab. escitalopram was added and optimized to 20mg, on which there was minimal improvement. After a six week trial of escitalopram, patient was shifted to cap.fluoxetine optimized to 60mg, on which there was improvement in psychomotor retardation, depressive cognitions, suicidal ideations and crying spells over a period of two months. However, patient continued to have residual symptoms in the form of anhedonia and lethargy. Also, there was a suggestion of cognitive deficits e.g. poor concentration, planning and calculations. Further augmentation with bupropion 150mg did not produce any significant change. A neuropsychological assessment revealed deficits in verbal working memory, visual processing speed, problem solving and executive functions. Cognitive remediation exercises were attempted by a clinical psychologist, but patient was uncooperative for the same. Patient was maintained on fluoxetine 60mg, bupropion 150mg, carbamazepine 600mg, and aripiprazole 10mg, on which she continued to have the residual symptoms. Her scores on psychopathology rating scales stabilized at HAMD=14 (Hamilton Depression Rating Scale) and CGI-S=3 (Clinical Global Impression Severity).
(1) Post contrast T1 sagittal section showing multiple meningiomas in fronto-parietal, temporal and occipital regions.

Post contrast T1 axial section showing meningiomas along the falx in the anterior interhemispheric fissure with buckling of adjacent cortex.
Discussion
The term ‘multiple meningioma’ was first used by Cushing and Eisehardt to describe the occurrence of multiple tumours in the absence of neurofibromatosis or acoustic neuromas [1]. They are defined as at least two spatially separated meningiomas occurring at the same time, or more than two meningiomas arising sequentially from two clearly distinct regions [2]. They constitute about 1.1% of all meningioma cases and can present with a wide variety of clinical symptoms including seizures and focal neurological deficits [3]. They may also often be clinically silent and present with only psychiatric symptoms [4]. Hence, detection of meningiomas presenting primarily with psychiatric symptoms in a patient suffering from chronic psychiatric illness is often fraught with diagnostic dilemmas [5].
Psychiatric symptoms caused by meningiomas vary and are usually related to the location and size of the mass and the time-course over which the tumours develop. Most meningiomas grow very slowly and are asymptomatic. A retrospective study of 72 meningioma cases showed that 21% present with only psychiatric symptoms [6]. Affective disorders were a common presentation and no correlation was found between brain laterality and psychiatric comorbidity. Lampl et al., re-examined patients with proven intracranial tumours and reported that 44% of those with convexity meningiomas had psychiatric comorbidity, whereas no psychiatric disorders were diagnosed in the non-convexity meningiomas. A statistically significant correlation was found between edema volume and the presence of coexisting psychiatric disorders, but not between the tumour’s mass volume and the psychiatric symptoms [7]. It is difficult to detect meningiomas because they grow slowly; the tumour is often located in a non-functional region, with a deficiency of localizing signs. Neurobehavioural changes observed in patients with intracranial meningiomas may appear as mood disturbances, changes in behaviour or decreased adaptability (e.g., drowsiness, apathy, loss of spontaneity, fatigue) [8]. WHO Grade I meningioma patients compared to healthy controls demonstrated a neurocognitive sequelae in the form of lower psychomotor speed, working memory and lower levels of self-perceived general health and vitality [9].
Our patient, who was a case of long standing bipolar disorder, presented with a completely different set of symptoms which could not be explained by her illness. Also, her symptoms were resistant to the treatment, on which she had previously shown satisfactory response. After receiving treatment for the multiple meningiomas, such atypicalities were not observed in the subsequent episodes. However, her subsequent depressive episode was more difficult to treat than her previous ones and she continued to show residual symptoms, in spite of adequate treatment.
Conclusion
These findings illustrate the need to assess for brain lesions in presence of atypical symptom presentation and unresponsiveness to traditional management with psychotropic medications in patients of long standing psychiatric illness. The findings also highlight the adverse effects of the structural lesion on further course and management of the primary psychiatric illness.
[1]. Cushing H, Eisenhardt L, Meningiomas: Their Classification, Regional Behaviour, Life History and Surgical End Result 1938 SpringfieldCharles C Thomas [Google Scholar]
[2]. Granger A, Sainsbury R, Wilkinson T, Macfarlane M, Multiple meningiomas: case report and review of the literatureJ Clinical Neurosci 2000 7(2):222-28. [Google Scholar]
[3]. Domenicucci M, Santoro A, D’Osvaldo DH, Delfini R, Cantore GP, Guidetti B, Multiple intracranial meningiomasJ Neurosurg 1989 70(1):41-4. [Google Scholar]
[4]. Moise D, Madhusoodanan S, Psychiatric symptoms associated with brain tumours: a clinical enigmaCNS Spectr 2006 11(1):28-31. [Google Scholar]
[5]. Kaur D, Ajinkya S, Nabi J, Manzoor A, Ghildiyal R, Meningioma masquerading as acute psychosis with symptoms of schizophreniaBombay Hospital Journal 2012 54(2):316-18. [Google Scholar]
[6]. Gupta RK, Kumar R, Benign brain tumours and psychiatric morbidity: a 5 years retrospective data analysisAust NZ J Psychiatry 2004 38(5):316-19. [Google Scholar]
[7]. Lampl Y, Barak Y, Achiron A, Sarova-Pinchas I, Intracranial meningiomas: correlation of peritumoural edema and psychiatric disturbancesPsychiatry Res 1995 58(2):177-80. [Google Scholar]
[8]. Pawełczyk A, łojek E, Rabe-Jabłotiska J, Pawełczyk T, Godlewski B, Radek M, Depression or apathy? A diagnostic trap: a huge right frontal lobe meningioma diagnosed and treated as mild atypical depression episode-a case studyPsychiatr Pol 2012 46(5):903-13. [Google Scholar]
[9]. van Nieuwenhuizen D, Ambachtsheer N, Heimans JJ, Reijneveld JC, Peerdeman SM, Klein M, Neurocognitive functioning and health-related quality of life in patients with radiologically suspected meningiomasJ Neurooncol 2013 113(3):433-40. [Google Scholar]