Health indicators in India have not yet demonstrated a concomitant improvement parallel to the national growth rates. However, the present health system has the advantage of wide network of health facilities across the country [1]. The Government of India’s initiatives in public health has recorded noteworthy success over time. Despite this, Indian health system is ranked 118 among 191 World Health Organization (WHO) member countries on overall health performance [2]. The performance in the field of maternal health is also lagging. India, Pakistan and Bangladesh accounts for 28% of the world’s births and 46% world’s of maternal deaths [3]. India has the largest number of maternal deaths estimated at about 1,17,000 [4]. Some of the medical reasons for such high Maternal Mortality Ratio (MMR) in India are non-availability of obstetricians and skilled birth attendants in rural areas [5–7]. While globally, maternal mortality is in decline, the decline in India has not been sufficient to attain Millennium Development Goal (MDG) 5 causing a moral urgency of reinvigorating effort [8].
Balasore district was selected owing to its high percentage of women undergoing antenatal checkups, given the understanding that Antenatal Checkups (ANC) influences the health-seeking behaviour and contributes in a significant way in the reduction of MMR by promoting new born care, immunization, institutional delivery and post-partum care.
The study site, Jaleswar block of Balasore district, comes under the Central Revenue Divisional Commissioner of Odisha. It was selected due to high concentration of tribal population and inaccessibility due to its riverine geographical structure. It is bordered by Mayurbhanj district of Odisha and Paschim Medinipur district of West Bengal. Many of the health centers of the block are declared as ‘difficult’ by the National Health System Recourse Centre (NHSRC), New Delhi [10].
The broad objective of the study was to assess the health system competency for the maternal health services in Balasore district and Jaleswar block of Balasore district, Odisha, India. In addition, the specific objectives of the study were as follows;
Materials and Methods
A mixed method approach was adopted in order to understand the health system competency for maternal health services in the study area. Primary data were collected by Focus Group Discussions (FGDs) and Key Informant (KI) interview techniques. Secondary data from various government documents were analysed to understand the Government policy implications. The Health Management Information System (HMIS) data were analysed for the comparison of Odisha and Balasore district in terms of registered pregnancy, ANC, and institutional delivery. The study has been carried out during the year 2012-13.
Results
This section delineates the major findings of health system competency at two different levels. The first section delineates the district level competency of Balasore district followed by block level competency of Jaleswar block of the same district.
1. Balasore District
Balasore District Profile
Balasore is one of the most populous districts of the state having 5.50% of total population in only 2.44% of the land area. High population density (532 sq/km), huge rural population (89.11%) and poverty (about 73%) status of the district demand immediate intervention in livelihood and infrastructure development. The district is located in deltaic region, criss-crossed by a good number of rivers and rivulets. These water bodies act as physical barriers and demand huge number of bridges, culverts to make all corners of the district accessible. Natural calamities play a destructive role in the district by damaging road network almost every year. Agriculture is the backbone of the district’s economy. It provides both direct and indirect employment to 67% of the workforce [11].
Lack of Basic Civic Amenities
There is shortage of pucca road, electricity connection and piped water in the health care centers including anganwadi centers in the district. Lacks of these amenities affect inter-sectoral coordination for National Rural Health Mission (NRHM), particularly improvement of the maternal health services in the district [11]. The lack of basic amenities acts an impediment for the rolling out of public health programs.
‘My advice about health and hygiene to the pregnant mothers do not yield result due to lack of wholesome water and balanced diet in the community. Anganwadi Centres do not have stocks of sufficient food and tablets for the pregnant mothers. The muddy road acts as an impediment for availing ANC especially in rainy season.’
– (An ASHA of Balasore District)
Gaps in Health Care Infrastructure
Analysis of existing health infrastructure revealed that against required strength of 483 Sub-centers, there are 275, of which only 87 sub-centers have dedicated pucca buildings. There are 66 PHCs in the district against the required strength of 81. Even existing PHCs lack ECG and X-Ray machines for proper diagnostic services. CHCs also lack basic diagnostic and ambulance services making the tribal pockets inaccessible. [Table/Fig-1] summarizes the infrastructural gaps in the district [11].
Public Health Infrastructure of Balasore district.
| Facility | Norms | Requirement as per norm | Actual Status | Gap |
|---|
| Health Sub-centre (HSC) |
| Provision of sub- centre | Provision of one Sub-centre per 5000 population | 483 | 275 | -208 |
| Human resource | 1 ANM, 1 MPW and 1 worker | 1449 | 627 | -822 |
| Medical kit | One Medical kit. | 483 | 275 | -208 |
| Working space | Dedicated pucca building | 483 | 87 | -396 |
| Primary Health Centre (single doctor PHC) |
| Provision of single doctor PHC | Provision of one PHC per 30,000 population | 81 | 66 | -15 |
| Working space | Dedicated pucca building | 81 | 66 | -15 |
| Diagnostic equipments | ECG | 81 | 0 | -81 |
| X-ray and accessories | 81 | 0 | -81 |
| Community Health Centers (CHC) |
| Provision of rural hospital | One CHC at every block headquarter | 12 | 14 | +2 |
| Working space | Dedicated pucca building | 12 | 14 | +2 |
| Diagnostic equipment | X-ray and accessories | 14 | 5 | -10 |
| Transport services | Ambulance services | 14 | 4 | -10 |
*Source: Office of the Chief District Medical Officer (2009)
Besides the infrastructural problems the district has widespread inaccessibility which has adverse impact on the provision of health care services. This is evident from the number of difficult areas identified by the NHSRC. There is one sub-divisional hospital at Nilagiri; one CHC at Baliapal; two PHCs at Pratappur and Berhampur; and nine PHC (N) at Ghantua, Langaleswar, Srirampur road, Jamakunda, Kalakad, Kansa, Betakata, Sajanagada and Ayodhya classified as difficult areas according to the NHSRC.
ANC Registration Increases but Early Registration is a Distance Dream
A comparison between registered pregnancy between the year 2010-11 and 2011-12 shows an increasing trend of total registered pregnant women for ANC, but a decreasing trend of registration within the first trimester for both state of Odisha and Balasore district. This may be due to low level of awareness in the community regarding the ANC services. The percentage increase in first trimester compared to total ANC registrations, but the percentage increase is marginal in case of Balasore district (56.3% to 57.1%) compared to the state (35.9% to 40.3%). This shows sluggish maternal health program in the district and the state as well which is far behind the national average and MDG 5. The [Table/Fig-2] enumerates the ANC registration during the year 2010-11 and 2011-2012 [12].
ANC registration during the year 2010-11 and 2011-2012.
| Total number of pregnant women Registered for ANC | Number of pregnant women registered within first trimester | Number of women registered under JSY | % 1st Trimester registration to total ANC registrations |
|---|
| 2010-11 | 2011-12 | 2010-11 | 2011-12 | 2010-11 | 2011-12 | 2010-11 | 2011-12 |
|---|
| Odisha | 854,464 | 880,334 | 306,355 | 354,836 | 779,554 | 880,314 | 35.9 | 40.3 |
| Balasore | 50,095 | 47,392 | 28,189 | 27,068 | 45,645 | 47,392 | 56.3 | 57.1 |
*Source: HMIS Portal (2013)
Increased number of Non-Skilled Birth Attendants (Non-SBA)
Number of home deliveries attended by non SBA trained birth attendants (TBA/Dai) is very high compared to number of home deliveries attended by SBA trained birth attendants (Doctor/Nurse/ANM) in both the case of the state and Balasore district as well. However the percentage of SBA attended home deliveries to total reported home deliveries are much low in Balasore (6.3% and 3.3% for the year 2010-11 and 2011-12 respectively) compared to the state average (23.2% and 14.8% for the year 2010-11 and 2011-12 respectively). In both the cases the percentage of SBA attended home deliveries to total reported home deliveries are glaringly low. This shows less penetration of the practice of skilled birth attendance in the rural area. The [Table/Fig-3] shows the number of home deliveries attended by SBA and non-SBA [12].
Mothers receiving services of SBA and non-SBA for home delivery.
| Number of Home deliveries | Number of home deliveries attended by SBA trained (Doctor/Nurse/ANM) | Number of home deliveries attended by Non SBA trained (trained TB/Dai) | % SBA attended home deliveries to Total Reported Home Deliveries |
|---|
| 2010-11 | 2011-12 | 2010-11 | 2011-12 | 2010-11 | 2011-12 | 2010-11 | 2011-12 |
|---|
| Odisha | 119,220 | 111,543 | 27,632 | 16,546 | 91,588 | 94,997 | 23.2 | 14.8 |
| Balasore | 3,194 | 2,553 | 200 | 85 | 2,994 | 2,468 | 6.3 | 3.3 |
*Source: HMIS Portal (2013)
Non-payment of Incentives to Mothers for Home Delivery
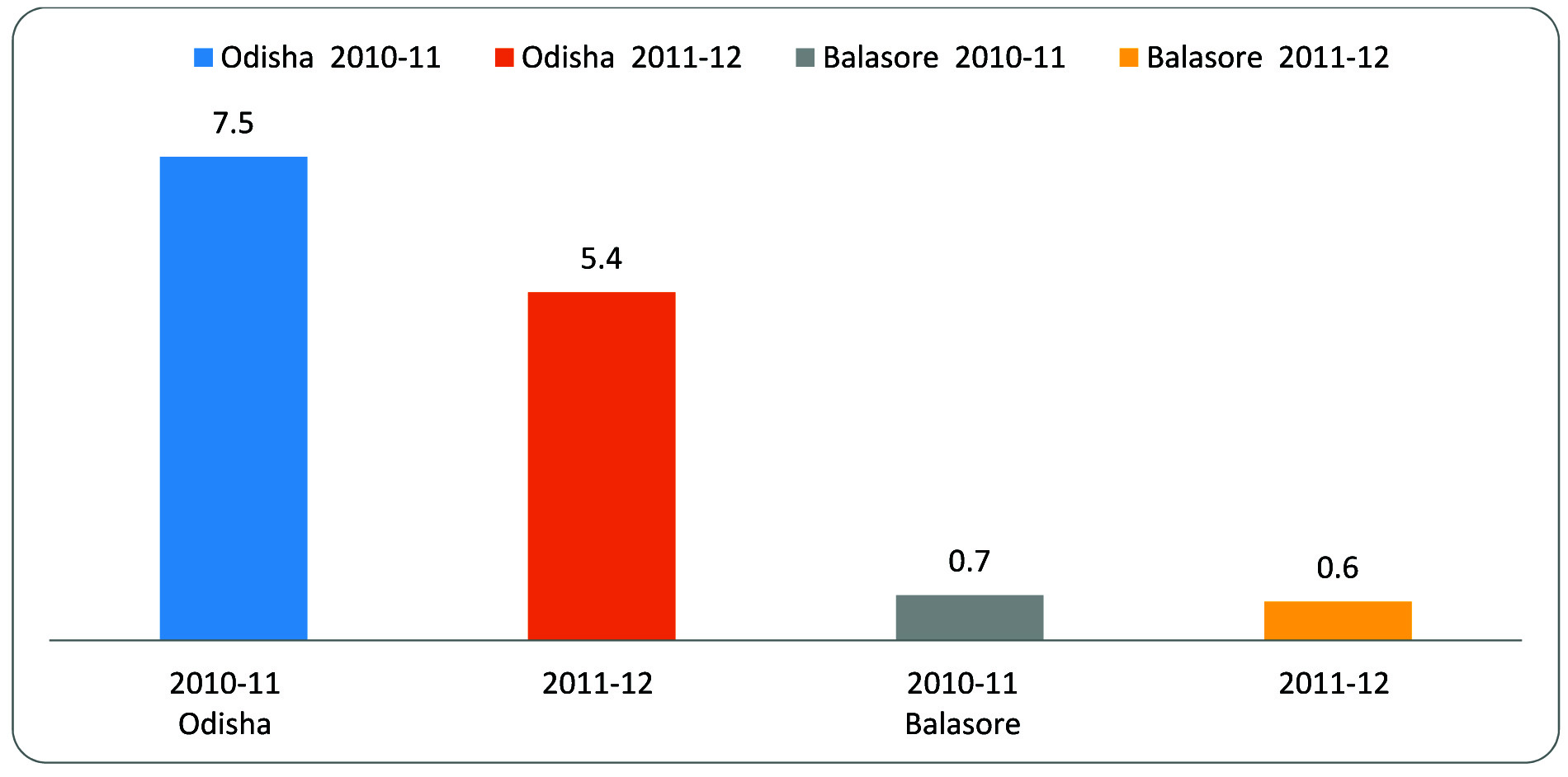
The percentage of mothers paid of JSY incentive for home deliveries to total reported home deliveries is very low in the case of both Balasore and Odisha. Though there is provision for JSY incentives for the home delivery, there is lack of proper mechanism for payment of JSY incentive for those deliveries. This further jeopardizes the health of both mother and child especially in tribal districts. The condition is much serious in Balasore (0.7% and 0.6% for the year 2010-11 and 2011-12 respectively) in comparison to State average (7.5% and 5.4% for the year 2010-11 and 2011-12 respectively) [12] [Table/Fig-4].
Mothers paid JSY incentives for home delivery
*Source: HMIS Portal (2013)
Decrease in Home Deliveries
Percentage of home deliveries to total reported deliveries is low in case of Balasore district (9% and 6.3% for the year 2010-11 and 2011-12 respectively) in comparison to State average (17.8% and 15.2% for the year 2010-11 and 2011-12 respectively). The percentage of home deliveries over the years has been decreasing showing more emphasis on institutional deliveries but the desired improvement in total institutional delivery is still a distant dream [12] [Table/Fig-5].
Home deliveries in Balasore.
| Institutional deliveries (Public +Private) | % of Institutional Deliveries to total ANC registration | Total reported deliveries | % of Institutional deliveries to Total Reported Deliveries | % of Safe deliveries to Total Reported Deliveries | % of Home deliveries to Total Reported Deliveries |
|---|
| 2010-11 | 2011-12 | 2010-11 | 2011-12 | 2010-11 | 2011-12 | 2010-11 | 2011-12 | 2010-11 | 2011-12 | 2010-11 | 2011-12 |
|---|
| Odisha | 549,012 | 735,648 | 64.3 | 70.9 | 668,232 | 624,105 | 82.2 | 84.8 | 86.3 | 87.1 | 17.8 | 15.2 |
| Balasore | 32,162 | 40,277 | 64.2 | 79.6 | 35,356 | 37,724 | 91 | 93.7 | 91.5 | 93.9 | 9 | 6.3 |
*Source: HMIS Portal (2013)
Irregularity in Post-Partum Care
Postpartum care in both Balasore District and Odisha has increased during the year 2010-11 and 2011-12. Balasore district is performing well in terms of women getting post-partum checkup between 48 hours to 14 days (71.1% in 2010-11 to 81.7% in 2011-12). However, the percentage of women receiving post-partum check-up within 48 hours of delivery to total reported deliveries have decreased (72.4% in 2010-11 to 66.7% in 2011-12) [12] [Table/Fig-6].
Post-partum care in Balasore.
| Women received post-partum check-up within 48 hours of delivery | Post-Natal Care / Women got a post-partumcheckup between 48 hours and 14 days | % Women receiving post-partum check-up within 48 hours of delivery to Total Reported Deliveries | % Women getting Post-Partum Checkup between 48 hours and 14 days to Total Deliveries |
|---|
| 2010-11 | 2011-12 | 2010-11 | 2011-12 | 2010-11 | 2011-12 | 2010-11 | 2011-12 |
|---|
| Odisha | 436,490 | 479,092 | 435,770 | 538,848 | 65.3 | 65.1 | 65.2 | 73.3 |
| Balasore | 25,580 | 26,843 | 25,140 | 32,895 | 72.4 | 66.7 | 71.1 | 81.7 |
*Source: HMIS Portal (2013)
2. Jaleswar Block
Basic Facts of Jaleswar Block
Jaleswar (384.11 Sq km) is a thickly populated block (population 1,13,329) of Balasore District having 256 villages and 34,138 households and has high concentration of SC (22.7%) and ST (27.9%) population. The block is also plagued by low literacy rate of 66.21% [11].
Inequitable Distribution of Health Infrastructure
Geographically, the Subarnarekha River divides the Block into 2 parts, i.e. Jaleswar and Hatigarh. In comparison to Hatigarh, the Jaleswar region is better placed in terms of infrastructure (14 out of 26 Sub-centres), manpower (99 out of 177 Ashas). The only First Referral Unit (FRU) (Gopi Kissan Bhattar) of the block is also situated in Jaleswar.
Lack of Awareness
A preliminary analysis of Block statistics for the month of August 2013 shows its low performance in ANC service. Although 309 women had registered for JSY, only 163 women registered within first trimester which shows lack of awareness. The number of pregnant women having hypertension and anaemia was 25 and 103 respectively. These predisposing factors for high risk pregnancy are widely prevalent in this block. Although JSY popularizes deliveries at home by trained birth attendants in remote area but there were no such cases for the month under consideration. Eight deliveries took place at home by traditional birth attendants (TBA). Although the block has witnessed a high emphasis on institutional deliveries, there has been no single case of caesarian delivery, in the FRU, which shows high referral rate to higher centers due to lack of functional manpower and technology (NRHM, 2012) [9].
‘It is difficult to identify the pregnancy cases at the earliest for provision of health care services. Pregnancy many a time detected and registered at advance stage due to lack of basic awareness in the tribal community. Even after training to the grass root level workers, it becomes difficult to educate the tribal community due to dialectical barriers, translation of medical terminology to layman’s understanding and frequent monitoring of the pregnant mothers.’
– (A block level administrator of Jaleswar Block)
Reluctance to Adhere to the Norms of 4 Mandatory ANC Checkups
The low level of availability of health care facilities is evident from poor OPD and IPD services. While OPD facilities are available at all health centers, IPD facility is only available at one CHC located at Hatigarh. The ANC services of Jaleswar Block need better improvement. The [Table/Fig-7,8] shows poor performance of Jaleswar block in terms of total ANCs (only 77%) of expectant mothers. There is a gradual decrease of ANC percentage from first to fourth (86% to 84% to 79% to 77%) [12].
ANC and Deliveries reported in Jaleswar Block for the year 2012-13.
| ANC1 | ANC2 | %ANC2 | ANC3 | %ANC3 | ANC4 | %ANC4 | Total ANC’s | %All ANC’s | Deliveries Reported | % Deliveries Reported |
|---|
| Hatigarh CHC | 5,043 | 4,242 | 84 | 3,992 | 79 | 3,586 | 71 | 3,502 | 69 | 3,443 | 68 |
| PPC-Jaleswar | 3,082 | 2,817 | 91 | 2,817 | 91 | 2,817 | 91 | 2,817 | 91 | 2,817 | 91 |
| Total Jaleswar | 8125 | 7059 | 86 | 6809 | 84 | 6403 | 79 | 6319 | 77 | 6260 | 77 |
*Adapted from HMIS Portal (2013)
Declining trend of ANC checkups and delivery in Jaleswar block
*Adapted from HMIS Portal (2013).
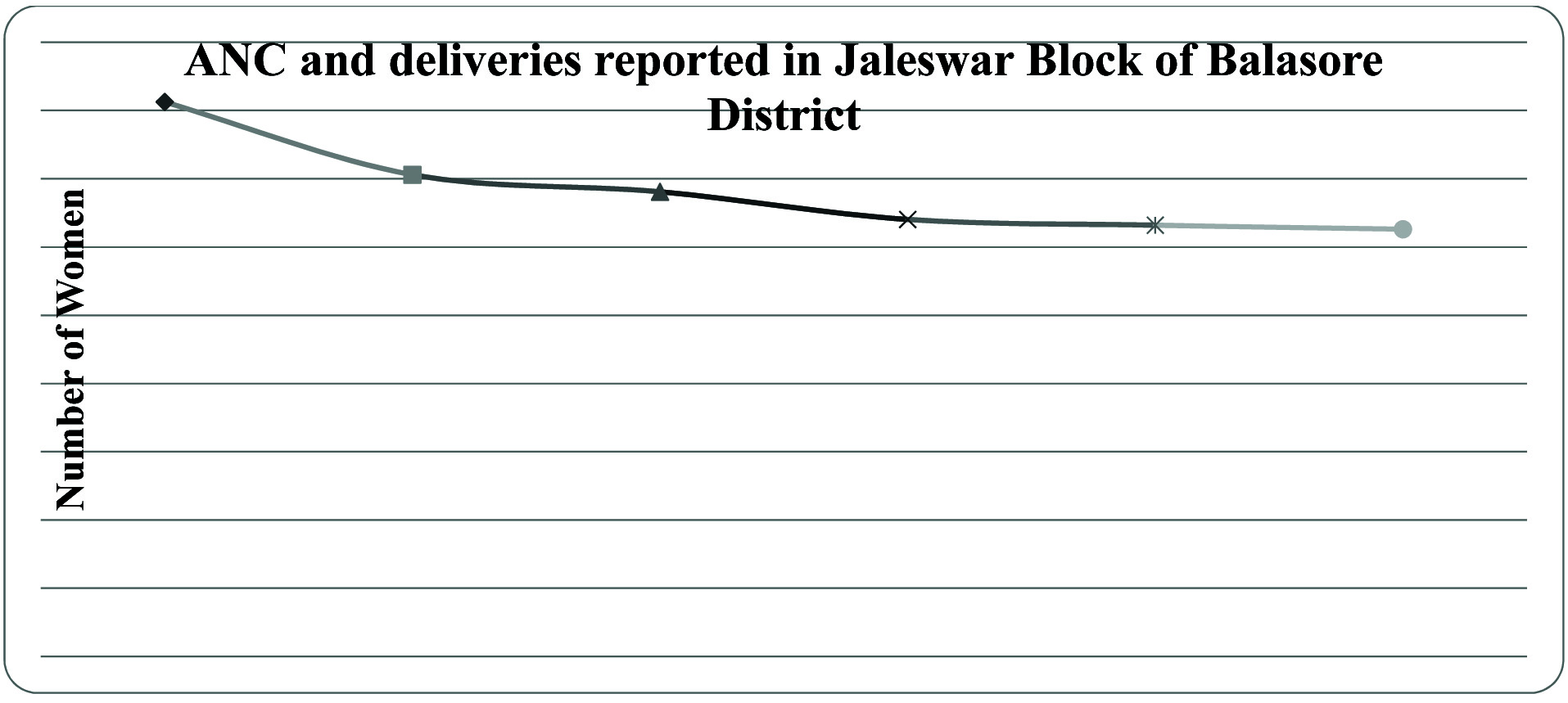
There is constant drop out of the cases in subsequent ANC visits due to lack of infrastructural and institutional problems in health care system.
‘Despite reaching out to the pregnant women for availing services of the health Centres it becomes difficult to ensure an institutional delivery. Sometimes they migrate for occupation to the nearby districts which results non-compliance with the ANC. Tribal beliefs and culture also hinder the utilization of biomedical services.’
– (An ASHA of Jaleswar Block)
Discussion
Poor transportation facility is a major barrier for women beneficiaries to avail institutional care. This is evident from low turnout in OPD and IPD services. Women fallout from regular ANC visits due to several reasons. Compliance with IPHS standards needs serious attention to ensure safe delivery. The IPHS standards provide enough scope for availability of quality services in public health institutions. The study recommends continuous tracking and follow-up of ANC at individual level. Similar findings are also found in Odisha by Mahapatra and Kumar and Shi et al., [13,14]. Further, they suggest improvement of basic infrastructure and referral network that could help in achieving better health of the vulnerable population. Hence, improving access of tribal communities to the health centers by strengthening communication facilities could improve the health status.
Additional efforts are required for capacity building of front line workers (ASHAs, ANMs, health workers, etc.) to track ANC progress by the help of HMIS. This will make home visits regular, effective and meaningful particularly in remote tribal communities. There is a need of flexible cash transfer schemes, particularly for tribes, understanding their difficulties in maintaining all records and documents.
Similar studies are consistent with our current findings reported by Joshi & George and Bhatia regarding the operational challenges in Maharashtra [15,16]. In addition to sufficient incentive, they suggest provision of regular training to grass root level workers to minimize attrition. Further, there is requirement of simplifying the procedures of reporting and monitoring of pregnant mothers. The ASHAs need to be given with sufficient drugs in ASHA kit to provide prompt care in the community.
Innovative methods may be adopted to empower tribal communities to identify important parameter of maternal morbidity: preventive measures, danger signs, referrals. This would ensure health seeking behaviours in the tribal communities. Social determinants of health in tribal area, especially improvement of living conditions, women leadership, education, money and other resources should be taken into consideration while rolling out JSY program in more inclusive manner. Besides focusing exclusively on increasing JSY coverage, a deeper insight is required to understand how the cash is spent at family level to reap the targeted benefit. Mahapatra & Kumar reported similar findings in tribes of Odisha [13]. They recommend improvement of living conditions by various government programs which ultimately promote the health of the tribal communities.
Rath and Acharya confirmed the importance of social determinants of health in tribal communities to gain health [17]. Further, their arguments are directed toward creating awareness about different tribal beliefs and practices that affect health in reproductive age. Emphasis on social determinants of health is a focus area for the improvement of health in the vulnerable community.
In addition, the findings of some of the similar studies have been evaluated regarding the maternal health situation and the utilization of services in different part of India in [Table/Fig-9].
Findings of various similar studies across India on utilization of services for maternal health.
| Authors | Journal | YOP | Study title/ Objective | Study type | Methodology and Setting | Major findings |
|---|
| Kohli, C., Kishore, J., Sharma, S., &Nayak, H. | J Family Med Prim Care. 2015; 4(3): 359–363. | 2015 | Knowledge and practice of Accredited Social Health Activists for maternal healthcare delivery in Delhi. | A descriptive cross-sectional study | The study was conducted in North-East district of Delhi among 55 ASHAs. Data were collected by semi-structured schedules which consist of socio-demographic profile of ASHAs and the measures for knowledge and practices regarding maternal health. | ASHAs were aware of their work of providing ANC services to the mothers, counseling to adopt family planning, distribution of 100 IFA tablets during pregnancy, and accompanying them for institutional delivery. In addition, shortage of staffs at health center, lack of transportation facility and lack of money for emergency services were the problems reported by ASHAs in Delhi [18]. |
| Singh A, Kumar A, Pranjali P. | Peer J | 2014 | Utilization of maternal healthcare among adolescent mothers in urban India: evidence from DLHS-3. | Cross- sectional study | Analysis of DLHS-3 data about the factors affecting utilization of health care services among pregnant mothers. | Socioeconomic and demographic factors have an influence for the utilization of services among the pregnant mothers of the nation. Age at marriage, religion, caste, wealth of household, parity, vulnerable social groups have an influence on the institutional delivery [19]. |
| Singh A, Padmadas SS, Mishra US, Pallikadavath S, Johnson FA, Matthews | PLoS ONE. 2012;7(5): e37037 | 2012 | Socio-Economic Inequalities in the Use of Postnatal Care in India. | Cross- sectional study | District Level Household Survey conducted in India in 2007–08. | Low level of PNC utilization is found in the data set. There is evidence that the utilization of PNC services helps in reduction of maternal and child mortality. Socio-economic inequalities have a great role in utilization of PNC services [20]. |
| Chaudhary AK, Chaudhary A, Tiwari SC, Dwivedi R. | Journal of Obstetrics and Gynaecology of India. 2012;62(3): 286-290. | 2012 | Can Community-Based, Low-Cost Antenatal Care in the Third Trimester of Pregnancy Reduce the Incidence of Low Birth Weight Newborns? | Descriptive study | Pregnant women of Banganga urban slum area situated near J.P. Hospital, which is the district hospital of Bhopal were studied for the utilization of services during the 3rd trimester. | The number of low birth weight babies can be reduced by availing low-cost care to the pregnant women mostly in last trimester of pregnancy in their community [21]. |
ANC- Ante natal care/check up, ASHA- Accredited Social Health Activist, IFA-Iron Folic Acid, DLHS-District Level Health Survey, PNC-Post natal care
Conclusion
The assessment at both the district level and block level in Balasore district showed a gloomy picture and provides ample room for improvement of the health system for the delivery of maternal health services in the region. The six health system building blocks depicted by the World Health Organization undoubtedly do not match the requisite standards of maternal health service delivery at both levels. All these six building blocks need to be strengthened in order to improve the maternal health services of the district. Considering the unusual physiography and socio-cultural context of the region specific strategies need to be devised for the delivery of desired maternal health services.
ANC- Ante natal care/check up, ASHA- Accredited Social Health Activist, IFA-Iron Folic Acid, DLHS-District Level Health Survey, PNC-Post natal care