The decision of whether or not to extract permanent teeth in proposing the treatment plan of an orthodontic case especially in border line cases is a critical moment for every clinician. Space analysis quantifies the amount of crowding within the arches and estimates the severity of space discrepancy.
Correction of many malocclusions requires space like crowding, retraction of proclined teeth, levelling a steep curve of spee, and correction of unstable molar relation [1]. The space gaining procedures include extraction and non-extraction. The non-extraction procedures generally carried out are arch expansion, proximal stripping and molar distalization.
Extraction as a space gaining procedure has been a controversial subject for as long as the speciality of orthodontics has existed. If the case selection is improper, the extraction of premolars might lead to over retraction, lingual tipping of maxillary incisors and dishing of profile, premature anterior contacts, distal displacement of mandible and its condyle [2].
The current orthodontic treatment goals focus on soft tissue assessment and management. The paradigm shift from hard tissues to soft tissues makes the face as the most important determinant during treatment planning. Evolution of mechano-therapy now minimizes the need for extraction even in severe space discrepancies [3].
One of such non-extraction methods of space gaining is molar distalization and the present study focuses on the same with the aim to identify the pattern of features seen in such cases.
Materials and Methods
The study was a retrospective one with the sample size of 20 subjects which were treated with molar distalization. Study models and lateral cephalograms of the subjects were collected. The study was conducted in the Department of Orthodontics, Mamatha Dental College, Khammam, Telangana, India, from 2011 to 2013. The ethical committee clearance was obtained. Informed consent was obtained from all the subjects to use their records.
Inclusion criteria: The criteria included border line cases with crowding in the upper arch not more than 4mm, end–on or Class II molar relation and well balanced face with straight profile.
Exclusion criteria: The criteria included severe overjet of more than 4mm, crowding exceeding 4mm, Class I molar relation and Convex/Concave profiles.
The treatment plan was decided based on clinical, study model and cephalometric analysis by panel of three Orthodontists whose experience in the field of speciality was 20, 7 and 5 years consecutively.
The study models and lateral cephalograms were obtained. All the lateral cephalograms were hand traced to obtain the Naso labial angle, Frankfort Mandibular Angle (FMA), Mandibular plane angle, Gonion–Gnathion to Sella- Nasion (GOGN-SN) and the Lower incisor long axis Incisor Mandibular Plane Angle (IMPA) [4].
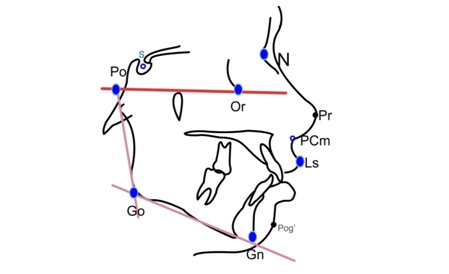
The Cephalometric landmarks marked were Sella, Nasion, Porion, Orbitale, Gonion, Gnathion, Posterior Columella point (PCm): the most posterior point of the lower border of nose at which it begins turn inferiorly to merge with the philtrum of the upper lip and Labrale superius (Ls): the point indicating the mucocutaneuos border of the upper lip [Table/Fig-1] [4].
Cephalometric landmarks used in the study [4].
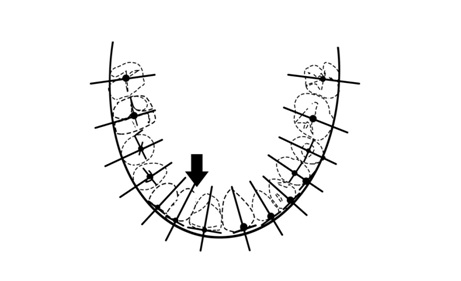
Using an Occlusogram, the first order discrepancy, molar and premolar rotations were measured. The occlusogram was obtained by transferring the occlusal surfaces from the cast on to the tracing paper which was later traced on to a graph paper and measurements were carried out by using metal ruler and a divider manually [5,6] [Table/Fig-2].
Occlusogram – To check the parameters for dental cast measurements [5,6].
Model analysis was carried out to check the Bolton’s discrepancy [7].
Error analysis: To estimate the reliability of cephalometric analysis, five randomly selected lateral radiographs were traced twice at an interval of one week. Measurement accuracy was obtained by calculating the error of the method and Houston coefficient of reliability.
Statistical Analysis
Descriptive statistics like mean, standard deviation, standard error, range, minimum and maximum values were obtained and tabulated.
Results
The dental cast measurements and cephalometric measurements have been depicted in [Table/Fig-3].
Statistical analysis showing mean, standard deviation, standard error and maximum and minimum values with range.
| S.No. | Variable | Mean(n=20) | Standard Deviation (SD)(n=20) | Stan-dard Error (SEM) | Maxim-um Value(n=20) | Minimum Value(n=20)Range(n=20) | Range(n=20) |
|---|
| 1. | First order discrepancy | 5 | 1.95 | 0.56 | 10mm | 3mm | 7 |
| 2. | Premolar rotation | 16.58 | 5.12 | 1.48 | 24 | 99 | 75 |
| 3. | Molar rotation | 7.66 | 2.26 | 0.653 | 11 | 5 | 6 |
| 4. | Nasolabial angle | 101.25 | 8.79 | 2.53 | 115 | 90 | 25 |
| 5. | Bolton’s discrepancy | 1.56 | 1.07 | 0.31 | 3.5 | -0.8 | 4.3 |
| 6. | FMA | 20.66 | 4.00 | 1.15 | 27 | 11 | 16 |
| 7. | GOGN-SN | 27 | 2.55 | 0.736 | 30 | 24 | 6 |
| 8. | IMPA | 101.41 | 5.74 | 1.65 | 114 | 92 | 22 |
Discussion
Oppenheim and Renfroe advocated mandibular distalization [8]. Renfroe reported that lip bumper primarily is a device to hold a hyper tonic lower lip away from the teeth. He observed that reaction of the lip caused movement of the molars sufficient to change their relationship from Class I to Class II malocclusion [8]. Gould was the first person to discuss about unilateral distalization of molars with extra-oral force [9].
The indications for molar distalization include straight profile, normal healthy temporomandibular joint, Class I skeletal normal or short lower face height, maxilla-normal transverse width, skeletal closed bite, Class II molar relationship, deep overbite, maxillary first molar mesially inclined, preferably prior to eruption of second molar, maxillary cuspids labially displaced, loss of arch length due to premature loss of second deciduous molar [10,11].
The advantages of molar distalization include reduction in amount and duration of appliance therapy, facilitation of treatment using removable appliance, good functional occlusion and natural contact area from canine to first molar retained [10–12].
Molar distalization is a unique procedure and yields excellent results when attempted on appropriate cases. The case selection is of utmost importance. Whenever we attempt to correct cases with obtuse nasolabial angle, with procedures like extractions, we end up giving a dished in profile to the patient. So alternative procedures like expansion and molar distalization also has to be kept in mind when handling such cases [13,14].
Borderline cases many a times call for a confusion whether the case to be done by extraction or non-extraction. Livas stated that, Class II treatment with extraction of two maxillary premolars exhibited retroclined maxillary central incisors after treatment compared to those with premolar extractions in both jaws and non-extraction therapy [15].
In the present study all the 20 patients were treated with molar distalization to further establish some more features seen in the malocclusion which can swing the treatment option to molar distalization rather than opting towards extraction of premolars (at least preventing the extraction of first premolars in patients having a good soft tissue). First order discrepancy between upper central and lateral incisors, rotation of premolars and molars and Bolton’s discrepancy in anterior dentition were found to be useful in considering molar distalization as a valid treatment plan.
Andrews in his study on aesthetically acceptable models and actors of Hollywood had established a pattern by dropping a parallel to true vertical line from the soft tissue glabella on smiling profile taken in Natural Head Position (NHP) and called it Goal Anterior Limit Line (GALL). This is to coincide with the most prominent point of central incisors in smiling profile. Space analysis chart was formulated using the concept of “SIX ELEMENTS TO OROFACIAL HARMONY” to be incorporated in devising the treatment plan [16].
Though this study has not incorporated those above parameters, further studies are required in order to get a perfect set of diagnostic features in order to end the controversy whether to perform extraction or do the case with non – extraction as a valid treatment plan in a given case.
Limitation
The limitation of the study was that the study was a retrospective one and only patients treated with molar distalization were the subjects with no control or pre-molar extraction group.
Conclusion
In the present retrospective study the following six features were studied with molar distalization cases. They include first order discrepancy between upper central and lateral incisor, rotation of premolars and molars, Bolton’s discrepancy in anterior dentition, average to horizontal growth pattern, proclined lower incisors and obtuse nasolabial angle.
Though the last three points were deemed to be already established indications, a combination of these six features in a particular case can be taken as a pattern seen in molar distalization and considered as the valid treatment plan.
The study can be extended by incorporating a control group and/or premolar extraction group and by incorporating GALL line as one of the parameters.