Massive Ovarian Oedema- A Case Report
Arun B Harke1, Karthik Sigamani2, Chitra Thukkaram3, Madhumittha Ramamurthy4, Manjani Sekar5
1 Professor, Department of Pathology, Karpaga Vinayaga Institute of Medical Sciences and Research Centre, Kanchipuram, Tamilnadu, India.
2 Assistant Professor, Department of Pathology, Karpaga Vinayaga Institute of Medical Sciences and Research Centre, Kanchipuram, Tamilnadu, India.
3 Professor and Head, Department of Pathology, Karpaga Vinayaga Institute of Medical Sciences and Research Centre, Kanchipuram, Tamilnadu, India.
4 Postgraduate Student, Department of Pathology, Karpaga Vinayaga Institute of Medical Sciences and Research Centre, Kanchipuram, Tamilnadu, India.
5 Postgraduate Student, Department of Pathology, Karpaga Vinayaga Institute of Medical Sciences and Research Centre, Kanchipuram, Tamilnadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Arun B Harke, Department of Pathology, Karpaga Vinayaga Institute of Medical Sciences and Research Centre, GST Road, Chinnakolambakkam, Palayanoor (po), Madhuranthagam (Tk), Kanchipuram (Dist), Tamilnadu-603308, India.
E-mail: Arun_harke@yahoo.com
Massive ovarian oedema is defined by WHO as formation of tumour like enlargement of one or both ovaries by oedema fluid. We report a case of a 18-year-old unmarried girl who presented with three months amenorrhoea and left sided lower abdominal pain with clinical and radiological diagnosis of cystic ovarian neoplasm. Patient underwent lapratomy with left salpingo-oophorectomy. A definitive diagnosis of Massive Ovarian Oedema (MOE) was offered on histopathological examination. The MOE should be differentiated from ovarian fibromatosis, ovarian fibroma, sclerosing stromal tumour and ovarian myxoma. The usual management of massive oedema of ovary is unilateral salpingo-oophorectomy, as the lesion is mistaken for primary ovarian neoplasm at laparotomy. Recognition of MOE is of great importance to prevent unnecessary oophorectomy in young patients and can be managed conservatively. We report this case of MOE for its rarity.
Cystic ovarian neoplasm, Ovarian myxoma, Salpingo-oophorectomy
Case Report
A 18-year-old unmarried girl presented with three months amenorrhoea and left sided lower abdominal intermittent, cramping pain since two months. There were no aggravating or relieving factors for the pain and it was not associated with vomiting or giddiness. She attained menarche at the age of 15 years. Her menstrual cycles were regular, with average flow and without dysmenorrhoea.
Per-abdominal examination revealed a supra-pubic nontender, mobile, cystic mass. Local examination revealed intact hymen. Per-rectal examination revealed a normal sized uterus and the same cystic mass was palpable on the left side of uterus.
Ultrasound examination of abdomen and pelvis revealed two cystic lesions in the left ovary- First cyst was a well-defined, thin walled, anechoic mass of 5×4.5 cm with no internal septations or echoes. Second cyst was a well defined, hypoechoic, thick walled mass of 10.6 × 5.7 cm with multiple internal septations and echoes- endometriotic/haemorrhagic cyst. The serum levels of Cancer Antigen 125 (CA -125), Carcinoembryonic Antigen (CEA), Alpha-Fetoprotein (AFP) were within normal limits.
Based on these findings a clinical diagnosis of cystic ovarian neoplasm was offered. Patient underwent laparotomy with left salpingo-oophorectomy.
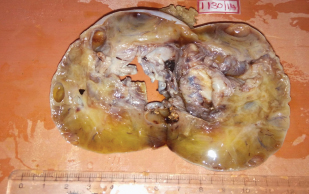
The external surface of the ovary was shiny, white and smooth [Table/Fig-1]. Cut section was pale, homogenous, soft in consistency and exuded lot of watery fluid after cutting. Cut section also showed multiple cystic areas [Table/Fig-2].
The external surface of the ovary was shiny, white and smooth.

Cut section: Pale, homogenous, soft with multiple cystic areas.
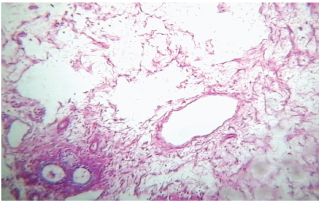
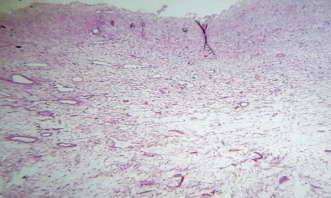
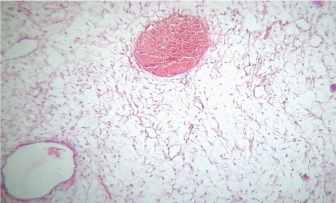
Multiple sections from the left ovary showed marked diffuse stromal oedema that surrounded the entrapped follicles [Table/Fig-3]. The periphery of the cortex showed normal ovarian stroma [Table/Fig-4]. The section also showed dilated vascular and lymphatic channels [Table/Fig-5]. Based on these findings a diagnosis of massive ovarian oedema (MOE) of the left ovary was offered.
Shows marked diffuse stromal oedema with entrapped follicles (H&E, 10x).
The periphery of the cortex shows normal ovarian stroma (H&E, 10x).
Shows dilated vascular and lymphatic channels (H&E, 10x).
Following surgery, patient had symptomatic improvement and was discharged with the advice of review after 15 days. However, the patient did not turn up for follow- up.
Discussion
MOE was first described by Kalstone et al., in 1969 and is defined by WHO as formation of tumour like enlargement of one or both ovaries by oedema fluid [1]. It usually occurs in young women between the age group of 6-33 years with an average age of 21 years [2].
The patients usually present with acute abdominal pain. Rarely, irregular menstruation can be a presenting feature. A palpable adnexal mass or virilisation can also be seen [3–5]. Our patient presented with 3 months of amenorrhea with intermittent lower abdominal pain and supra-pubic mass. There were no signs of virilisation.
Majority of ovarian oedema are unilateral (85%) & most involve right ovary [6]. Present case was also unilateral, however it involved left ovary. Massive ovarian oedema can occur as primary or secondary condition [7]. Primary oedema occurs when the ovary is not diseased and when there is torsion or twisting of the ovarian pedicle to the extent that it interferes with the venous drainage leading to oedema and does not affect the arterial blood flow [7]. Secondary ovarian oedema occurs in a diseased ovary such as ovarian mass & cyst, malignancy, fibromatosis, polycystic ovaries or following ovulation induction drugs [7].
In a meta-analysis done by Praveen et al., from 1969 – 2011, a total of 177 cases of massive ovarian oedema were identified [8]. Out of these cases 151 (85.3%) were primary massive ovarian oedema; secondary massive ovarian oedema was identified in 26 (14.7%) cases [8].
In spite of advanced technology it is difficult to diagnose massive oedema of ovary pre-operatively with imaging techniques. Ultra-sonographically the lesion usually appears solid, however it can also show cystic areas [6]. Majority of cases were reported as non-specific heterogenous complex ovarian mass ultrasonographically mimicking a neoplastic condition [6,9]. However, when a solid ovarian mass with multiple peripheral ovarian follicles is noted ultrasonographically, the possibility of massive ovarian oedema should be considered as suggested by Umesaki et al., [10]. The lesion in the present case was reported as multicystic lesion, ultrasonographically.
Morphological recognition of massive ovarian oedema, by and large, is an easy affair. On cut section, MOE appears gray in colour, soft in consistency with fluid oozing out due to the internal pressure of oedema [11].
On histopathological examination, the lesion shows widely separated ovarian stromal cells by copious oedema fluid. Caught in the oedema fluid are atretic follicles. The tunica albugenia and superficial cortical zones are uninvolved [12]. The stroma also shows dilated lymphatic & vascular channels. The MOE should be differentiated from ovarian Fibromatosis, ovarian fibroma, Sclerosing stromal tumour and ovarian myxoma [12]. In ovarian fibromatosis, the tumour shows proliferation of spindle cells producing collagen with focal storiform pattern enveloping the follicles [11]. Ovarian fibroma has uniform firm solid white cut surface and microscopically there is diffusely arranged spindle shaped cells forming collagen, at places arranged in storiform pattern with the follicle at the periphery. In sclerosing stromal tumour, there is well demarcated solid white mass with few yellow areas & oedema, cyst formation and microscopically there are two types of cells, spindle shaped cells and round cells arranged in pseudolobules. Ovarian myxoma has soft and cystic consistency and microscopically there is spindle shaped & stellate cells in myxoid background [12].
On review of literature it is observed that unilateral salpingo-oophorectomy is done for most cases of ovarian oedema as they are mistaken for ovarian tumours at laparotomy [8]. Conservative treatment must be the rule since the disorder is non-neoplastic [8]. However, most cases are over treated and this entity should be suspected in women in fertile age group with solid enlargement of ovary. When condition of MOE is suspected at the time of surgery, the appropriate treatment is wedge resection, removing 30% or more of ovary to exclude secondary causes of the condition [8]. Frozen section is valuable during the time of surgery [8]. In our case MOE was not suspected and hence unilateral salpingo-oophorectomy was performed.
Conclusion
Recognition of MOE is of great importance to prevent unnecessary oophorectomy in young patients and can be managed conservatively.
[1]. Kalstone CE, Jaffe RB, Abell MR, Massive oedema of the ovary simulating fibromaObstet Gynecol 1969 34:564-71. [Google Scholar]
[2]. WHO classification of tumours, Tumours of Breast and Genital Organs 2003, IARC Press, page 190 [Google Scholar]
[3]. Mohan H, Mohan P, Bal A, Tahlan A, Massive Ovarian Oedema: Report of two casesArch Gynecol Obstet 2004 270:199-200. [Google Scholar]
[4]. Rosai J, Rosai and Ackerman’s Surgical Pathology 2004 9th edPhiladelphiaElsevier Inc:1649-1736. [Google Scholar]
[5]. Clement PB, Non neoplastic lesions of ovary. In Kurman R J (Ed)Blaustin’s Pathology of the Female Genital Tract 2002 5th edNew YorkSpringer-Verlag New York Inc:699-703. [Google Scholar]
[6]. Roberts CL, Weston MJ, Bilateral Massive Ovarian Oedema: a case reportUltrasound Obstet Gynecol 1998 11:65-67. [Google Scholar]
[7]. Daboubi MK, Khreisat B, Massive ovarian oedema: literature review and case presentationEastern Mediterranean Health Journal 2008 14(4):972-79. [Google Scholar]
[8]. Praveen RS, Pallavi VR, Rajashekar K, Usha A, Umadevi K, Bafna UD, A clinical update on massive ovarian oedema – a pseudo tumour?E cancer medical science 2013 7:318 [Google Scholar]
[9]. Shirk JO, Copas PR, Kattine AA, Massive Ovarian oedema in a menopausal woman. A case reportJ Reprod Med 1996 41(5):359-62. [Google Scholar]
[10]. Umesaki N, Tanaka T, Miyama M, Kawamura N, Sonographic characteristics of massive ovarian oedemaUltrasound Obstet Gynecol 2000 16(5):479-81. [Google Scholar]
[11]. Mills SE, Carter D, Greenson JK, Sternberg’s Diagnostic Surgical Pathology 2010 5th edPhiladelphiaWolters Kluwer/ Lippincott Williams & Wilkins:2315-2316.:2364-65. [Google Scholar]
[12]. Roth LM, Deaton LM, Sternberg WH, Massive ovarian oedema. A clinicopathological study of five cases including ultra structural observations and review of the literatureAmerican journal of surgical pathology 1979 3(1):11-21. [Google Scholar]