Oral cancer can be considered as an epidemic in the recent century. In Indian subcontinent oral cancer is either the most common cancer or second most common cancer in men, accounting up to 10% of all new cases [1]. It is the most common form of cancer and cancer-related death in men (83,000 new cases and 46,000 deaths yearly) [2]. The Kerala state records a high incidence of oral cancer in India: 20.9 for males and 12.6 for females [3]. In 2009–10, of the 13,040 new cases registered in Regional Cancer Centre, Kerala state, head and neck clinic reported 2408 new cases [3]. These higher rates of oral cancer in India can be easily attributed to high prevalence of tobacco use [4].
Review of previous published literature reveals that a large proportion of oral cancers are preceded by pre-existent, long-standing Oral Leukoplakia (OL). OL is a relatively common lesion of the oral mucosa, affecting 0.2% to 4.9% of the world population [5]. Leukoplakia is defined as “A white plaque of questionable risk having excluded (other) known diseases or disorders that carry no increased risk for cancer” [6]. The term “leukoplakia” is usually later replaced by the diagnosis obtained after histopathological examination of the tissue. The histopathological aspects of OL may vary from atrophic epithelium to hyperplasia with or without hyperkeratosis and dysplasia. Conventionally, dysplasia is divided into grades: mild, moderate, and severe. The presence of moderate or severe dysplasia has been accepted to have the greatest likelihood for malignant transformation [7].
Previous literature suggests that malignant transformation rates of OL range from 0.13 to 17.5% [8,9]. The rates of malignant transformation of OL are different in different parts of the world, probably as a result of diversity in cultural and environmental factors like tobacco habits, dietary habits, pollution, etc. Many factors have been possibly associated with an increased risk of malignant transformation. Nevertheless, the histopathological grading of epithelial dysplasia remains one of the most clinically important predictors of malignant potential [10,11]. In a population with high prevalence of tobacco use even though the rate of malignant transformation of OL over a period of time has been studied before, little is known about carcinomatous foci within OL at the time of initial diagnosis of leukoplakia [12,13]. Thus, this study aims to determine the prevalence along with risk factors for carcinoma within OL lesions at the time of initial clinical presentation and the prevalence and risk factors for dysplasia in these lesions.
Materials and Methods
Total 600 cases of OL were retrieved from the archives of the Department of Oral Pathology, Government Dental College, Thiruvananthapuram, India in between a period of 11.5 years (January 2000 to June 2011). The definition of OL was in accordance with World Health Organization criteria [14]. In our institution, all cases of OL after the elimination of suspected etiological factors were routinely advised to receive tissue biopsy or surgical excision to get an accurate diagnosis before they were further managed or followed. Of the total, 54 cases were excluded from the study since data was incomplete. Clinical information of patients regarding sex, age, site, tobacco use and appearance were collected. The data was cross checked by two investigators so as to avoid repetition of the cases. The slides were retrieved and the final definitive diagnosis was made based on histopathological examination after confirmation by two oral pathologists. Grading of epithelial dysplasia was also based on the WHO guidelines [14]. Whenever the OL lesions showed the presence of Verrucous Carcinoma (VC), or Invasive Squamous Cell Carcinoma (SCC), regardless of the extent, they were recorded as positive for the presence of carcinomatous foci within OL. The data was analyzed and the distribution of these clinical variables between males and females was examined. Prevalence rates of malignancy and Epithelial Dysplasia (ED) within OL were determined further according to different clinical subgroups.
Statistical Analysis
The data were tabulated and analyzed statistically using the Statistical Package for the Social Sciences software. The pearson chi-square test was used to compare differences between groups, which were regarded as significant when the p-value was less than 0.05. Logistic regression analysis was also conducted to calculate odds ratio with 95% confident intervals for these parameters in relation to the presence of ED or malignancy.
Results
Among the 546 cases of OL, there were 181 females (33.2%) and 365 males (66.8%), with a male to female ratio of 2:1. The age of the patients ranged from 16 to 87 years old with peak of occurrence of OL in the fifth and sixth decades of life. There was statistically significant difference between the gender and the age distribution of patients in the study. Among the females 68% of the patients presented with OL who were greater than 50 years of age where as in males 50% cases were below 50 years of age [Table/Fig-1].
Clinicopathologic correlation of the cases in relation to gender.
| Age (years) | Male | Female |
|---|
| < 30 | 29 | 2 |
| 7.90% | 1.10% |
| 30 - 49 | 151 | 55 |
| 41.40% | 30.40% |
| ≥ 50 | 185 | 124 |
| 50.70% | 68.50% |
| Mean ±SD | 51.62 ±17.85 | 56.2 ±12.76 |
| Chi square: 20.632; p <0.001 |
| Site |
| Buccal Mucosa | 168 | 63 |
| 46.00% | 34.80% |
| Lateral Tongue | 108 | 66 |
| 29.60% | 36.50% |
| Palate | 22 | 13 |
| 6.00% | 7.20% |
| Dorsum of Tongue | 10 | 12 |
| 2.70% | 6.60% |
| Floor of Mouth | 12 | 8 |
| 3.30% | 4.40% |
| Retromolar Trigone | 13 | 8 |
| 3.60% | 4.40% |
| Gingiva | 12 | 7 |
| 3.30% | 3.90% |
| Lip | 20 | 4 |
| 5.50% | 2.20% |
| Chi square: 13.906; p<0.05 |
| Tobacco Use |
| No | 40 | 21 |
| 11.00% | 11.60% |
| Yes | 325 | 160 |
| 89.00% | 88.40% |
| Chi square: 0.50; p: NS |
| Clinical Appearance |
| Homogenous | 297 | 136 |
| 81.40% | 75.10% |
| Non Homogenous Speckled | 51 | 34 |
| 14.00% | 18.80% |
| Non Homogenous Verrucous | 17 | 11 |
| 4.70% | 6.10% |
| Chi square: 2.868; p: NS |
| Histology |
| Hyperplasia with No Dysplasia | 98 | 31 |
| 26.80% | 17.10% |
| Mild Dysplasia | 114 | 50 |
| 31.20% | 27.60% |
| Moderate Dysplasia | 72 | 37 |
| 19.70% | 20.40% |
| Severe Dysplasia | 35 | 33 |
| 9.60% | 18.20% |
| Invasive Cancer | 34 | 20 |
| 9.30% | 11.00% |
| Verrucous Hyperplasia | 6 | 5 |
| 1.60% | 2.80% |
| Verrucous Cancer | 6 | 5 |
| 1.60% | 2.80% |
(Chi square: 14.525; p <0.05)
Buccal mucosa (42.3%) was the most commonly affected oral site followed by lateral border of the tongue (31.8%). Other less commonly involved sites were palate (6.4%), floor of the mouth (3.7%), dorsum of tongue (4%), retro-molar trigone (3.8%), gingiva (3.4%) and lips (4.3%). There was statistically significant difference between patient gender and the site of the lesion with buccal mucosa having the highest predominance among males (46%) followed by the lateral border of the tongue (29.6%). Whereas in females, pattern of distribution on tongue and buccal mucosa was almost similar (36% and 34% respectively). Of the less commonly involved anatomic sites considered in this study, all sites except lips had female predilection [Table/Fig-1].
Although tobacco use is considered to be more in males, there was no statistically significant association between gender of the patients presented with leukoplakia and tobacco use. Nearly 90% of the males as well as females had a history of tobacco use.
Of the total, 79.3% (433) of the lesions manifested as homogeneous white patches, while 20.7% (113) presented as non-homogenous lesions. Among non-homogenous patches 75% cases were speckled and rest were verrucous in appearance. There was no statistically significant association between patient gender and clinical appearance of the lesion.
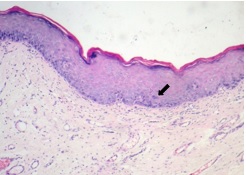
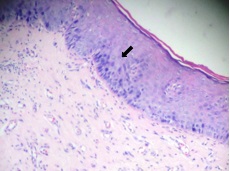
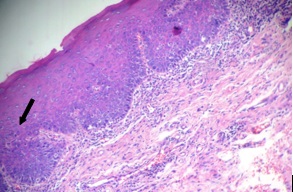
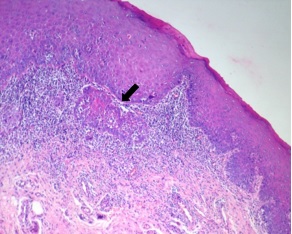
The histological aspects of the biopsied or surgical specimens are also shown in [Table/Fig-1]. In 129 cases only epithelial hyperplasia and/or hyperkeratosis (EH) were noted. In 164 cases mild dysplasia was noted [Table/Fig-2]. Moderate dysplasia and severe dysplasia were noted in 109 and 68 cases respectively [Table/Fig-3,4]. Verrucous hyperplasia was present in 11 cases. Invasive SCC was present in 54 cases and VC was present in 11 OL cases, resulting in an 11.9% prevalence rate of carcinoma among all OL lesions [Table/Fig-5]. There was significant difference between males and females regarding histology of the lesion with female sex being associated with higher grades of dysplasia.
Epithelial hyperplasia with mild dysplasia.
Epithelial hyperplasia with moderate dysplasia.
Epithelial hyperplasia with severe dysplasia.
Epithelial hyperplasia turning into invasive carcinoma.
After the exclusion of cases with carcinoma and verrucous hyperplasia the remaining OL cases were examined for risk factors associated with the presence of ED by univariate analysis [Table/Fig-6]. Since lot of controversies and difficulties still persists in diagnosing benign verrucous lesions, verrucous hyperplasia was not included in this analysis [14,15]. Although not significant those aged greater than 30 years had twice the risk of presence of dysplasia in an OL. Female sex showed a mild increase in risk when compared to males (OR=1.3). Among the sites taken into consideration, Floor of the Mouth (FOM) had significantly higher risk (OR=4.29) when compared to the other sites. Use of tobacco was strongly correlated with the presence of epithelial dysplasia within OL with tobacco users showing six times the risk of presenting with dysplasia with an OL. Regarding clinical appearance non homogenous speckled OL cases presented with very high risk (OR=12.63) when compared with homogenous variant.
Univariate analysis of dysplasia within OL related to clinical variables.
| Gender | Non Dysplasia | Epithelial Dysplasia | Odds ratio [95% CI] |
|---|
| Male | 89 | 221 | 1 |
| 64.80% |
| Female | 40 | 120 | 1.282 |
| 35.20% | [0.883-1.861] |
| Chi square: 0.939; p: NS |
| Age (years) |
| < 30 | 9 | 16 | 1 |
| 4.70% |
| 30 - 49 | 35 | 125 | 1.72 |
| 36.70% | [0.819-3.613] |
| ≥ 50 | 85 | 200 | 1.189 |
| 58.70% | [0.826-1.711] |
| Chi square: 2.510; p: NS |
| Site |
| Buccal Mucosa | 72 | 131 | 1 |
| 38.40% | |
| Lateral Tongue | 38 | 127 | 1.527 |
| 37.20% | [0.628-3.709] |
| Palate | 5 | 18 | 0.74 |
| 5.30% | [0.297-1.843] |
| Dorsum of Tongue | 4 | 7 | 1.889 |
| 2.10% | [0.643-5.545] |
| Floor of Mouth | 2 | 15 | 4.286 |
| 4.40% | [1.246-14.735] |
| Retromolar Trigone | 2 | 13 | 0.667 |
| 3.80% | [0.178-2.498] |
| Gingiva | 3 | 14 | 1.231 |
| 4.10% | [0.362-4.182] |
| Lip | 3 | 16 | 0.714 |
| 4.70% | [0.189-2.695] |
| Chi square: 24.654; p <0.01 |
| Tobacco Use |
| No | 55 | 38 | 1 |
| 11.10% | |
| Yes | 74 | 303 | 5.924 |
| 88.90% | 3.647- 9.628 |
| Chi square: 58.48; p: <.001 |
| Clinical Appearance | | | |
| Homogenous | 116 | 280 | |
| 82.10% | |
| Non Homogenous Speckled | 2 | 61 | 12.635 |
| 17.90% | [3.052-52.031] |
| Non Homogenous Verrucous | 11 | - | |
| Chi square: 20.620; p <0.001 |
Regarding the carcinomatous foci the analysis showed that lesion site, clinical appearance and tobacco use were strongly correlated with the presence of carcinoma within OL (all p<0.05) [Table/Fig-7]. Tongue and FOM had significantly higher risk for the presence of carcinoma when compared to other sites. Non homogenous lesions presented with significantly higher risk (OR=8.94) when compared with homogenous variant. When different subtypes of non homogeneous OL were further analyzed, the risk was highest in the verrucous (OR=25.22) followed by speckled lesions (OR = 6.05) when compared with homogeneous OL. Tobacco users had a four times risk (OR=4.4) compared to non tobacco users to have a malignant foci within the leukoplakia.
Univariate analysis of carcinomatous foci within OL related to clinical variables.
| Non Carcinoma | Carcinoma | Odds ratio |
|---|
| Male | 325 | 40 | |
| 67.60% | 61.50% | 1.302 |
| Female | 156 | 25 | [0.763-2.222] |
| 32.40% | 38.50% | |
| Chi square: 0.939; p: NS |
| Age (yrs) |
| < 30 | 30 | 1 | 1 |
| 6.20% | 1.50% |
| 30 - 49 | 186 | 20 | 4.981 |
| 38.70% | 30.80% | [0.662-37.465] |
| ≥ 50 | 265 | 44 | 1.544 |
| 55.10% | 67.70% | [0.881-2.706] |
| Chi square: 4.780; p: NS |
| Site |
| Buccal Mucosa | 210 | 21 | 1 |
| 43.70% | 32.30% |
| Lateral Tongue | 153 | 21 | 3.654 |
| 31.80% | 32.30% | [1.252-8.456] |
| Palate | 29 | 6 | 2.863 |
| 6.00% | 9.20% | [0.912-5.998] |
| Dorsum of Tongue | 15 | 7 | 3.115 |
| 3.10% | 10.80% | [1.521-5.845] |
| Floor of Mouth | 16 | 4 | 2.987 |
| 3.30% | 6.20% | [1.112-6.781] |
| Retromolar Trigone | 17 | 4 | 1.857 |
| 3.50% | 6.20% | [0.112-3.478] |
| Gingiva | 17 | 2 | 1.035 |
| 3.50% | 3.10% | [0.137-4.578] |
| Lip | 24 | | |
| 5.00% | | |
| Chi square: 16.532; p <0.05 |
| Tobacco Use |
| No | 59 | 2 | |
| 12.30% | 3.10% | 4.404 |
| Yes | 422 | 63 | [1.050-18.474] |
| 87.70% | 96.90% | |
| Chi square: 4.872; p <0.05 |
| Clinical Appearance |
| Homogenous | 408 | 25 | |
| 84.80% | 38.50% | |
| Non Homogenous Speckled | 62 | 23 | 8.942 |
| 12.90% | 35.40% | [5.117-15.629] |
| Non Homogenous Verrucous | 11 | 17 | |
| 2.30% | 26.20% | |
| Chi square: 97.738; p <0.001 |
Discussion
Oral cancer is almost always preceded by premalignant lesion or related visible changes in the mucosa, which allow clinicians to detect and effectively treat early intraepithelial stages of oral carcinogenesis. However, as far as the situation in Indian subcontinent is considered, most oral cancers are currently detected at a late stage with very poor survival. Oral cancer has many attributes in comparison with other malignancies - easy access to a health care provider, presence of detectable precursor lesion and very good survival rate if treated in early stages. The reason for the delay in detection of oral cancer in spite of apparent existence of easily detectable premalignant lesions remains poorly understood [1,2,16,17].
The OL is the most common premalignant lesion of the mouth. The crucial factor regarding OL is that, when the malignancy develops in these lesions the clinical appearance in the initial stages may remain the same. They may not present with the classic characteristics of a malignancy such as ulceration or induration. Understanding the prevalence of carcinomatous foci in clinically non suspicious OL and the associated risk factors is beneficial as it may help in identification of high-risk lesions in the oral cavity.
Previous literature across the world suggests that 3.1% to 12.9% of OL had at least one focus of SCC in the initial biopsy [16–18]. In a country like India where oral cancer is one of the most common cancers, this focus of SCC is something to be carefully followed upon. In our series, carcinoma was concurrently present in 11.9 % of the 546 OL cases, in accordance with those reported previously [19–21]. Nevertheless we believe that the actual prevalence of carcinoma in leukoplakia would be even much more as some lesions included in this study were only subjected to incisional biopsy and patients had not returned for an excisional biopsy. It is always possible that carcinomatous foci have been missed in some of these cases. The importance of histological evaluation of the entire OL lesion has also been emphasized in a study by Vedtofte et al., in which four out of 61 OL lesions had superficial carcinomas in their excision specimen which were undiagnosed in the previous preoperative biopsy [19]. In a study by Cheisa et al., 10% of lesions were malignant in excision biopsy which was undetected in incisional biopsy [20]. Pentenero et al., found out eight cases of carcinoma which were also under diagnosed in the initial biopsy of 46 oral mucosal dysplastic lesions [17]. In a recent series by Lee et al., in Taiwan, 12% of carcinoma cases remained undetected by single incisional biopsy [21]. As we can see that high prevalence of carcinomatous foci in OL is a constant finding in all these studies, we recommend that excision biopsy is mandatory for OL at least in country like India where oral cancer is one of the most common cancers.
The age of presentation is an important clinical parameter which has got a definite role in diagnosis as well as management. In our study, the age range was 16 to 82 years with majority of the patients in the fifth and sixth decade. The males who presented with leukoplakia were significantly younger than women. Half of the men were less than 50 years with a significant proportion presenting at a much younger age, i.e., < 30 years. Only 16 among the 25 patients below 30 years of age presented with various grades of dysplasia. This finding is quite significant as there is a recent trend of rise in the premalignant and malignant lesions in young age group [22]. The youngest patient in our study was 16 years who presented with a lesion on the lateral border of tongue with moderate dysplasia.
The male to female ratio in this study was 2:1. Majority of the patients irrespective of sex had a history of tobacco use. It was not possible to analyze the type of tobacco and the duration of use because the investigation was retrospective and was made with medical records, many of them lacking this information. Alcohol was also not included in the study due to the same reason. Although in Indian scenario tobacco use is much more common in males when compared to females we could not find any significant difference in tobacco use between males and females in our study [4]. So even though the number of female patients was lesser, 90% of them were tobacco users thus depicting the fact that tobacco users among females have significant higher risk of developing leukoplakia when compared to the male counterparts. Of the total 18% of the females included in the study had severe dysplasia, where as only 9.6% of the males included in the study had severe dysplasia. Prevalence of carcinomatous change in the OL was more in females (13.8%) where as only 11% of the males presented with malignant changes in the OL. This again emphasizes the fact that females with tobacco use are high risk cases which should alert the clinician at the time of initial presentation itself.
With regard to lesion site, 46% of OL in men were located on buccal mucosa, whereas in women lateral border of the tongue as well as buccal mucosa had similar prevalence (36.5% and 34.8% respectively). This may be due to the tobacco related habits especially in India where the betel quid is in intimate contact with the buccal mucosa and the lateral border of tongue.
Univariate analysis revealed that lesion site, clinical appearance, and tobacco use have significant influences on the presence of carcinomatous foci in OL lesions. It is also significant to note that these same factors (lesion site, clinical appearance and tobacco use) are also risk factors for dysplastic change in OL. In the study we found that the chance of having carcinoma and ED were respectively 3.52 and 1.52 fold higher in OLs on lateral border of tongue, compared to those on buccal mucosa. FOM has even higher risk (4.2 fold) of developing ED. Similar results were found in earlier studies, which showed that oral ED, especially severe ED, is prone to occur on the lateral borders of tongue and FOM and OLs in these locations have a higher potential of malignant transformation [8,23,24]. This similarity between risk sites associated with carcinoma and dysplastic change in OL lesions implies that carcinomatous lesions are preceded by a stage of dysplastic change [16]. According to Lee et al., the higher risk in FOM and ventrolateral tongue may be attributed to more exposure from carcinogens pooled in saliva than other areas of the oral cavity [16]. Even though there is lack of evidence based literature supporting the concept of trauma being an etiologic factor for oral cancer it has been considered so for quite a long time by many clinicians. Most of the people in their fifth and sixth decade may have sharper cusps due to attrition. So trauma from these teeth can also be considered as a cofactor for the lesions developing at the ventrolateral surface of tongue and FOM. The lower degree of keratinization and higher permeability of the mucosa in these regions as indicated in human studies may also enhance the effect of local carcinogens [16]. In our study palate and retromolar trigone were also having a higher risk of presence of concomitant carcinoma in OL (OR=2.8 and 1.8 respectively) when compared to buccal mucosa. One possible explanation for the higher risk in these regions is that these areas are substantially more exposed to carcinogens from the tobacco smoke which is usually directed towards posterior parts than other areas of the oral cavity.
Clinical subtype is another major indicator for carcinoma and ED in OL. In the study, compared with homogeneous OL, non homogeneous lesions were at an 8.9 fold greater risk to contain foci of carcinoma and had a 12.63 fold higher chance of having ED. in The non homogenous type verrucous variant had much fold greater risk (22 fold) than the speckled variant (6.05 fold) to contain a foci of carcinoma. The frequencies of having ED were 85% for non homogeneous lesions and 70% for the homogeneous OL. Previous studies had similar results for non-homogenous leukoplakia [16, 18]. But the frequency of dysplasia in homogenous leukoplakia is much higher than those reported previously. This high prevalence of dysplasia in Leukoplakia may be due to many reasons. It may be attributed to the high tobacco use in India. However, it may also be due to a sampling bias since the study was a hospital-based study. Patients seeking help at a medical centre may have more awareness about the mucosal alterations than those patients with OL identified in a community survey. Nevertheless, further studies at community level are needed to clarify the influence of sampling basis on the clinical characteristics of oral leukoplakia.
In this study we found that when compared with the abstainers, patients who used tobacco were having a six fold higher risk to present with dysplastic foci and four fold higher risk to present with carcinomatous foci within their OL lesions. Numerous studies have indicated a definitive link between tobacco (smoking as well as smokeless) and oral cancer. It is also considered to be an etiologic factor in the development of OL. Our study also support the concept that tobacco plays a significant role in all stages of progression of leukoplakia i.e., OL-dysplasia-invasive carcinoma spectrum. This finding also signifies the importance of excisional biopsy and strict follow-up in OL patients who are absolute tobacco users.
Our study has tried to address the prevalence and risk factors for epithelial dysplasia as well as carcinoma within OL lesions at the time of initial clinical presentation in South Indian population where the prevalence of tobacco use is quite high. However, a government hospital based sample may not signify an authentic prevalence of carcinoma in OL of the general population, risk factors identified in the study can still alert clinicians to take appropriate precautions for high-risk cases.
Conclusion
In summary, it can be stated that few white lesions of oral cavity which are provisionally diagnosed as OLs may contain a malignant foci. Lesions presenting with a non-homogeneous appearance, on tongue or FOM in patients with tobacco use are at a significantly higher risk. However, it should be noted that homogeneous lesions at other sites of the oral cavity also have the possibility to harbour carcinomatous foci within the bland looking lesion. It is also possible that these foci might have been missed the initial incision biopsy.
Mass population screening has been advocated for breast and cervical cancer by WHO using mammography and cytology screening since cancer screening is the vital element for early cancer detection. Several studies are currently trying low cost methods for screening different types of cancer and precancerous lesions. But in comparison with other malignancies oral cancers can be recognized at an early stage as they are easily accessible to visual and tactile examination as well as surgical exploration under local anesthesia. In such a scenario the high prevalence of carcinomatous foci in a bland looking “oral white lesion” gains significance. Moreover there is no evidence for the concept that any treatment would prevent the possibility. Also the efficacy of long term follow up of oral leukoplakia patients in the presence of dysplasia is not well established. It is also very difficult to ensure that patients are coming for follow up in developing countries like India where data management and record keeping is not at par with the western countries. Furthermore patients may not always be able to see the same doctor for their follow up. Seems wise to suggest that all OLs should undergo excisional biopsy and histopathologic examination rather than longterm follow up so that we can detect all the carcinomatous foci in early stage itself and proceed with management accordingly.
(Chi square: 14.525; p <0.05)