Bronchoesophageal Fistula Repair with Intercostal Muscle Flap Followed by Occlusion of Residual Diverticula with N-butyl Cyanoacrylate (NBCA) Glue: A Case Report
Manuj Kumar Saikia1, Jyoti Prasad Kalita2, Akash Handique3, Noor Topno4, Kalyan Sarma5
1 Professor and Head, Department of Cardiothoracic and Vascular Surgery, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, Meghalaya, India.
2 Assistant Professor, Department of Cardiothoracic and Vascular Surgery, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, Meghalaya, India.
3 Associate Professor, Department of Radiology & Imaging, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, Meghalaya, India.
4 Professor and Head, Department of Surgery, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, Meghalaya, India.
5 PG Resident, Department of Radiology & Imaging, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, Meghalaya, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jyoti Prasad Kalita, Assistant Professor, Department of Cardiothoracic and Vascular Surgery, North Eastern Indira Gandhi Regional Institute of Health and Medical Science, Shillong-18, Meghalaya, India.
E-mail: atojpk@gmail.com; j.p.kalita17@gmail.com
The incidence of bronchoesophageal fistula in presence of benign pathology of tracheal tree or oesophagus is rare. It is encountered in thoracic diseases like tuberculosis, syphilis or histoplasmosis due to erosion by infected lymph node or abscess to adjoining structures. The source of primary pathology has to be eliminated followed by appropriate steps of fistula tract closure is essential for optimal result. We report a 25-year-old patient with left sided bronchoesophageal fistula. He had a past history of pulmonary tuberculosis. A left lower lobectomy followed by repair of oesophageal fistula opening was performed by primary closure and reinforcement with an intercostal muscle flap based on posterior intercostal artery. Postoperative oesophagogram showed short diverticula, which was occluded with n-butyl cyanoacrylate (NBCA) glue under radiological guidance. Feeding was started one week after application of glue without further complication. Reports on intercostals muscle flap repair and intervention of residual oesophageal diverticula with n-butyl cyanoacrylate (NBCA) glue under radiological guidance are scanty.
Lobectomy, Oesophagus tomography, Tracheal tree
Case Report
A 25-year-old man from a remote area presented with complaints of recurrent cough mostly after intake of liquid food. He had history of pulmonary tuberculosis four years back. A barium swallow oesophagus imaging was done in local hospital and a fistula between oesophagus and left lower lobe of lung was identified. He was advised to avoid oral food completely by local physician and feeding was started through a jejunostomy only. He was on exclusive jejunostomy food for last three years. A barium swallow oesophagogram showed two fistula tract originating at the level of mid oesophagus and terminating in left lower lobe bronchial tissues {[Table/Fig-1a] red arrow}. An oesophagoscopy confirmed the diagnosis showing two fistula openings in oesophagus at 34-35cm from incisor teeth {[Table/Fig-1b] red arrow}. A feeding tube was tried to pass across the oesophageal opening with an aim to act as a guide at the time of operation. A contrast computed tomography of chest showed destroyed bronchiactatic left lower lobe {[Table/Fig-1c] red arrow}.
(a) Barium oesophagogram shows fistula tracks (Red arrow) originating in midoesophagus and directing towards left lower lobe of lung. (b) Oesophagoscopy shows two fistulas (Red arrow) opening at 34-35 cm from incisior teeth. (c) Contrast enhanced computed tomography of chest shows collapsed and bronchiectatic (Red arrow) left lower lobe.

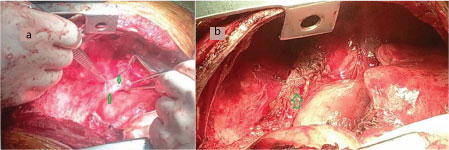
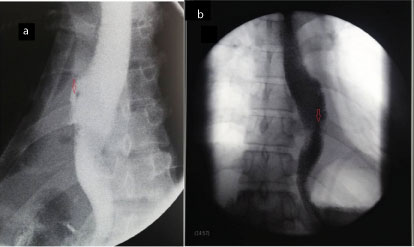
Patient was taken up for surgery. Left sided chest cavity was approached through fifth intercostal space and an intercostal muscle pedicle based on posterior intercostals artery was isolated. The left lower lobe was found to be collapsed and destroyed. A left lower lobectomy was performed. Two fistula opening in oesophagus were identified {[Table/Fig-2a] green arrow} which was further confirmed by occluding the distal oesophagus with a soft aortic cross clamp and forced injection of saline through a proximally placed feeding tube. Oesophageal openings were primarily closed with 5-0 prolene sutures. The intercostal muscle pedicle was used to reinforce the closure of fistula openings {[Table/Fig-2b] green arrow}. Chest was closed in layers with an intercostal tube in situ. A repeat barium swallow oesophagogram was performed at three weeks, showed small diverticula at the previous fistula site {[Table/Fig-3a] red arrow} which was occluded with n-butyl cyanoacrylate (NBCA) glue under radiological guidance [Table/Fig-3b] red arrow}. Oral feeding was started one week after application of glue. The patient has been on periodic follow-up for last 1 year without any further complication.
(a) Intaroperative picture shows fistula openings in oesophagus (Green arrow). (b) Intercostal muscle pedicle based on posterior intercostals artery in situ (Green arrow).
(a) Postoperative contrast oesophagogram showing diverticula at lower mid oesophagus (red arrow). (b) Post n-butyl cyanoacrylate (NBCA) glue application oesophagogram showing complete occlusion of mouth of diverticula (red arrow).
Discussion
The bronchoesophageal fistula formation in acquired diseases like tuberculosis, syphilis or histoplasmosis due to erosion of infected lymph node to adjoining structures or abscess formation has been reported in literature [1,2]. Swallow-cough sequence (Ono’s sign) is the classical presentation and it should raise the suspicion of the diagnosis in patient those who had previous history of pulmonary infection [2].
The usual etiology of tracheo-oesophageal fistula in adults is malignancy [3]. The benign causes of tracheo-oesophageal fistula are delayed presentation of congenital trachea-oesophageal fistula or rupture of congenital trachea-oesophageal membrane, post- traumatic, post-inflammatory secondary to trauma, oesophagitis, caustic injury and mediastinitis, post-operative conditions like vagotomy for hiatus hernia and pulmonary resection [3–5]. Chronic infective diseases like tuberculosis, syphilis or histoplasmosis are other important causes of benign trachea-oesophageal fistula in which infected lymph nodes erodes adjacent structures [1].
The usual presentation is bouts of cough and choking after eating and the symptoms are more with the liquids then solid [6]. The initial workup in a suspected case is contrast enhanced swallow study of oesophagus, which almost in all cases demonstrate the fistula tract. An upper gastrointestinal endoscopy and brochoscopy further helps to visualise the fistula or a diverticula [2]. An appropriate scopy helps in visualizing the fistula opening, mucosa of the tracts and it can be used to seal the fistula tract by interventional procedure. A contrast enhanced computed tomography scan of chest is emerging as an essential tool of diagnosis [7]. It helps in evaluation of fistula, luminal condition of tracheal tree and oesophagus and also helps to evaluate the status of diseased lobe of lung, lymph node or any mass lesion.
Appropriate preoperative planning is essential for better outcome. Antibiotics aimed at control of lung infection and chest physiotherapy to improve the pulmonary function and measures to improve the nutritional status including feeding jejunostomy should be considered [5]. Conservative management of tracheo-oesophageal fistula is hardly successful and hence direct surgical repair is the procedure of choice [3,5].
The preferred approach for thoracic tracheo-esophaseal fistula is right posterolateral thoracotomy which gives adequate exposure of oesophagus and right tracheal tree [3]. If the fistula tract terminates in left bronchial tree then the approach should be left posterolateral thoracotomy. A cervical approach is preferred in cases of tracheo-oesophageal fistula above the level of clavicle [3,5].
A ‘three layer repair’ is advisable whenever feasible [5,8]. A primary closure of the defect in oesophagus followed by reinforcement of repair site with intercostal or any other locally available muscle interposition flap is positioned. Intercostal muscle flap is posterior intercostal artery based flap. The defect in tracheal tree is closed primarily with nonabsorbable suture like prolene. The interposition graft supports the healing and acts as barrier between tracheal tree and oesophagus thus preventing recurrence. Again if the underlying lung is destroyed and is brochiectatic because of the primary disease process like in tuberculosis and if that particular area is not contributing to ventilation, it should be resected so that the chance of recurrence is minimised as it was done in our case. The left lower lobe was completely destroyed in our patient with areas of dilated and saccular changes in bronchioles. Gastric pull through or oesophageal bypass with transverse colon is done in presence of irreparable damaged oesophagus or oesophageal stricture [3].
There are few reports on successful endoscopic occlusion of idiopathic benign oesophago-bronchial fistula using fibrin sealant agent in certain patient where surgery is contraindicated for co-morbidities [9]. However; the literature for radiological guided application of sealant agent for obliteration of oesophegeal diverticula is limited.
Conclusion
A bronchoesophageal fistula should be considered in patients with suggestive symptomatology with underlying acute or chronic pulmonary diseases. An aggressive approach should be pursued for early diagnosis with all indicated investigative modalities if needed. An appropriate plan of management to be thought for primary surgical closure of fistula opening followed by interposition intercostals muscle flap should be considered. Patients with muscle interposition have lower morbidity and mortality and better long-term results. For residual diverticula, the possibility of radiological or endoscopic guided application of sealant agent should be kept in mind once primary pathology is eliminated.
[1]. Ramo OJ, Salo JA, Isolauri J, Luostarinen M, Tuberculous fistula of the oesophagusAnn Thorac Surg 1996 62:1030-32. [Google Scholar]
[2]. Gerzic Z, Rakic S, Randjelovic T, Acquired benign oesophagorespiratory fistula: report of 16 consecutive casesAnn Thorac Surg 1990 50:724-27. [Google Scholar]
[3]. Anshuman D, Abhishek S, Shekhar T, Non malignant tracheo-oesophageal fistula : our experienceIJTCVS 2005 21:272-76. [Google Scholar]
[4]. Holman WL, Vaezy A, Postlethwait RW, Bridgman A, Surgical treatment of H-Type tracheoesophageal fistula diagnosed in an AdultAnn Thorac Surg 1986 41:453-54. [Google Scholar]
[5]. Mathisen DJ, Grillo HC, Wain JC, Management of acquired nonmalignant tracheoesophageal fistulaAnn Thorac Surg 1991 52:759-65. [Google Scholar]
[6]. Singh G, Kele AS, Congenital broncoesophageal fistula presenting in adults. research & reviewsJournal of Surgery 2012 1(2) [Google Scholar]
[7]. Sakamoto Y, Seki Y, Tanaka N, Nakazawa T, Tracheoesophageal fistula after blunt chest trauma: successful diagnosis by computer tomographyThorac Cardiovasc Surg 2000 48:102-03. [Google Scholar]
[8]. Lee LM, Razi A, Three-layer technique to close a persistent tracheo-oesophageal fistulaAsian J Surg 2004 27:336-38. [Google Scholar]
[9]. Yellapu RK, Gorthi JR, Kiranmayi Y, Endoscopic occlusion of idiopathic benign oesophago-bronchial fistulaJournal of Postgraduate Medicine 2010 56(4):284-86. [Google Scholar]