Medicines are being purchased by patients in India with or without prescription and are stored at home. Prescription drugs are intended mainly for current use and sometimes left unused, which may get expired or may be repeated in the form of self medication. Re-use of leftover drugs for self initiated treatment is unsafe, especially antibiotics and other prescription drugs which should be used under supervision of medical professional [1].
Storage of large quantity of medications at home increases the risk of a wide range of potential drug-related problems, like errors in taking medications, accidental poisoning, adverse drug reactions, and can be considered as a waste of resources [2].
In developing countries like India, easy availability of wide range of drugs results in increased proportions of drugs used for self-medication compared to prescribed drugs [3]. So this can lead to misuse and abuse of medicines.
Availability of Over The Counter (OTC) medicines added with self medications, potentiates the chance of side effects and drug interactions which are not known to general people.
This study was aimed to explore the utilization pattern of medicines available at different houses of Anand district of Gujarat both in urban and rural setup with special objectives of: 1) availability and types of medicine with or without prescription; and 2) utilization of these medicines by the members.
Materials and Methods
This was a cross-sectional study conducted in Anand district of Gujarat, India during the year 2012-2014. This study was approved by Human Research Ethics Committee (HREC). A total of 800 houses, 400 each from urban and rural areas, were included for the study which was based on prevalence of self medication as per previous study done in India [4]. By taking the prevalence of self medication 37% in this study and considering 10% as non response, our sample size was calculated as 800.
The Anand district has eight Talukas. To get the representative data from Anand district, it was divided on the basis of eight Talukas. From each selected town and villages of each Talukas, 50 houses were selected from different areas after making five to six small clusters. So a total of 800 houses were included for the study.
Data were collected by the principal investigator using pretested self-designed study tool with questionnaire labeled as data collection form based on related studies [5,6]. To test the suitability and feasibility of it, pilot study was conducted in 50 houses and appropriate changes were made. House to house survey was carried out by the principal investigator in order to do whole study.
The participants above the age of 18 years, capable of giving information of medicine use within the family (the heads of the households or their spouses or any adult capable of delivering required information) were interviewed for the study. Presence of any health care professional amongst the family members in visited house was excluded in order to avoid biased answer.
The interview was held in local language with prior written consent, privacy and confidentiality of the members interviewed were also taken care of from ethical point of view. Each interview took around 1 hour. The eligible family member present at house was asked to show medicines available at home if any.
Data collected for the study included the details of medicines available in the house as: (i) number of homes having medicines; (ii) number of formulations with and without prescriptions; (iii) number of formulations with package inserts & expired formulations; (iv) Dosage forms of medicines; (v) pharmacological class wise distribution of medicines; (vi) status of the medicine use whether for current use, future use or leftover; and (vii) adherence of dose and duration of treatment as per prescriber’s advised in case of prescription medicines and appropriateness of dose and duration of treatment of medicine actually consumed in case of without prescription medicines. Data so collected were compiled in Microsoft excel format. Statistical analysis was done using percentage and chi- square test as applicable. The p-value less than 0.05 were considered as significant.
Results
Out of total 800 houses visited in urban area, 93.75% houses were found to have medicines either for current use, future use or left over whereas 88.50% houses in rural area were having medicines for the same. Amongst them, 38.25% and 23% of families were possessing medicines without prescription in urban and rural area respectively. In the urban area significantly more houses had medicines without prescription compared to rural area. (χ2: 21.8923, p: <0.00001).
A total of 3438 medicine formulations were available in 729 families with an average 5.11 ± 3.42 (mean±SD) in the urban houses and 4.31±3.19 in the rural houses [Table/Fig-1]. Out of these, more medicine formulations were found without prescription in urban area (16.76%) than in rural area (11.82%).
Number of formulations available per house.
| No. of formulations per house | Number of house n (%) |
|---|
| Urban | Rural | Total |
|---|
| 1 | 47 (12.54) | 59 (16.67) | 106 |
| 2 | 53 (14.13) | 60 (16.95) | 113 |
| 3 | 48 (12.80) | 63 (17.80) | 111 |
| 4 | 42 (11.2) | 51 (14.41) | 93 |
| 5 | 40 (10.67) | 29 (8.19) | 69 |
| 6 | 37 (9.87) | 18 (5.09) | 55 |
| 7 | 26 (6.93) | 18 (5.09) | 44 |
| 8 | 20 (5.33) | 19 (5.37) | 39 |
| 9 | 20 (5.33) | 10 (2.82) | 30 |
| 10 | 9 (2.4) | 9 (2.54) | 18 |
| 11 | 13 (3.47) | 5 (1.41) | 18 |
| 12 | 5 (1.33) | 4 (1.13) | 9 |
| 13 | 8 (2.13) | 2 (0.56) | 10 |
| 14 | 3 (0.8) | 2 (0.56) | 5 |
| 15 | 1 (0.27) | 1 (0.28) | 2 |
| 16 | 2 (0.53) | 2 (0.56) | 4 |
| 17 | 0 (0) | 1 (0.28) | 1 |
| 18 | 0 (0) | 0 (0) | 0 |
| 19 | 0 (0) | 1 (0.28) | 1 |
| 20 | 1 (0.27) | 0 (0) | 1 |
| Total houses | 375 (100) | 354 (100) | 729 |
| Total formulations | 1915 | 1523 | 3438 |
| Mean ± SD | 5.11±3.42 | 4.31±3.19 | 4.72 |
Maximum numbers of formulations were in the form of oral dosage 3015 (87.7%), out of which tablets were found to be highest (2138) followed by syrup (586) and capsules (168). There were total 382 topical dosage forms of which eye drops (111) and creams (105) were found maximally. Rotahaler and Metered dose inhaler were also found, but in less number (21) and used only with prescription medicines.
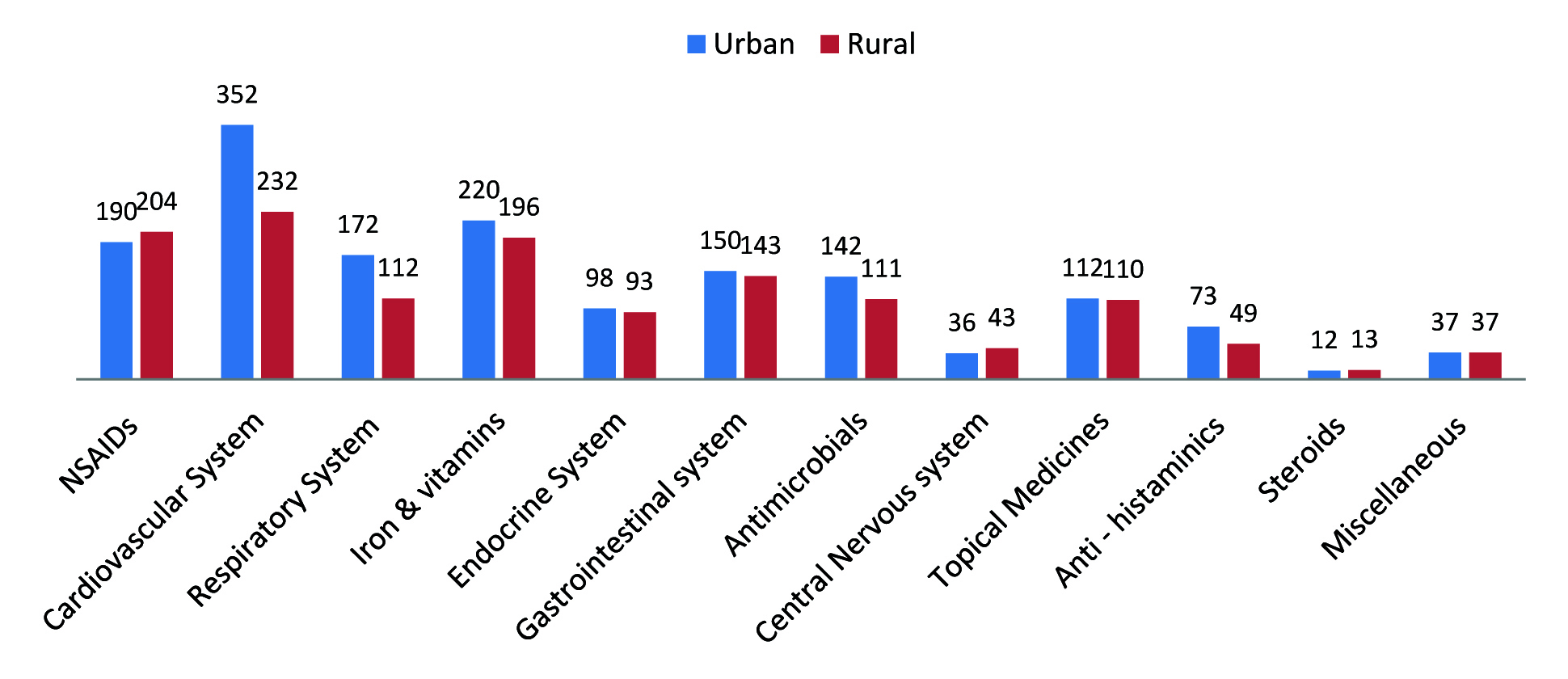
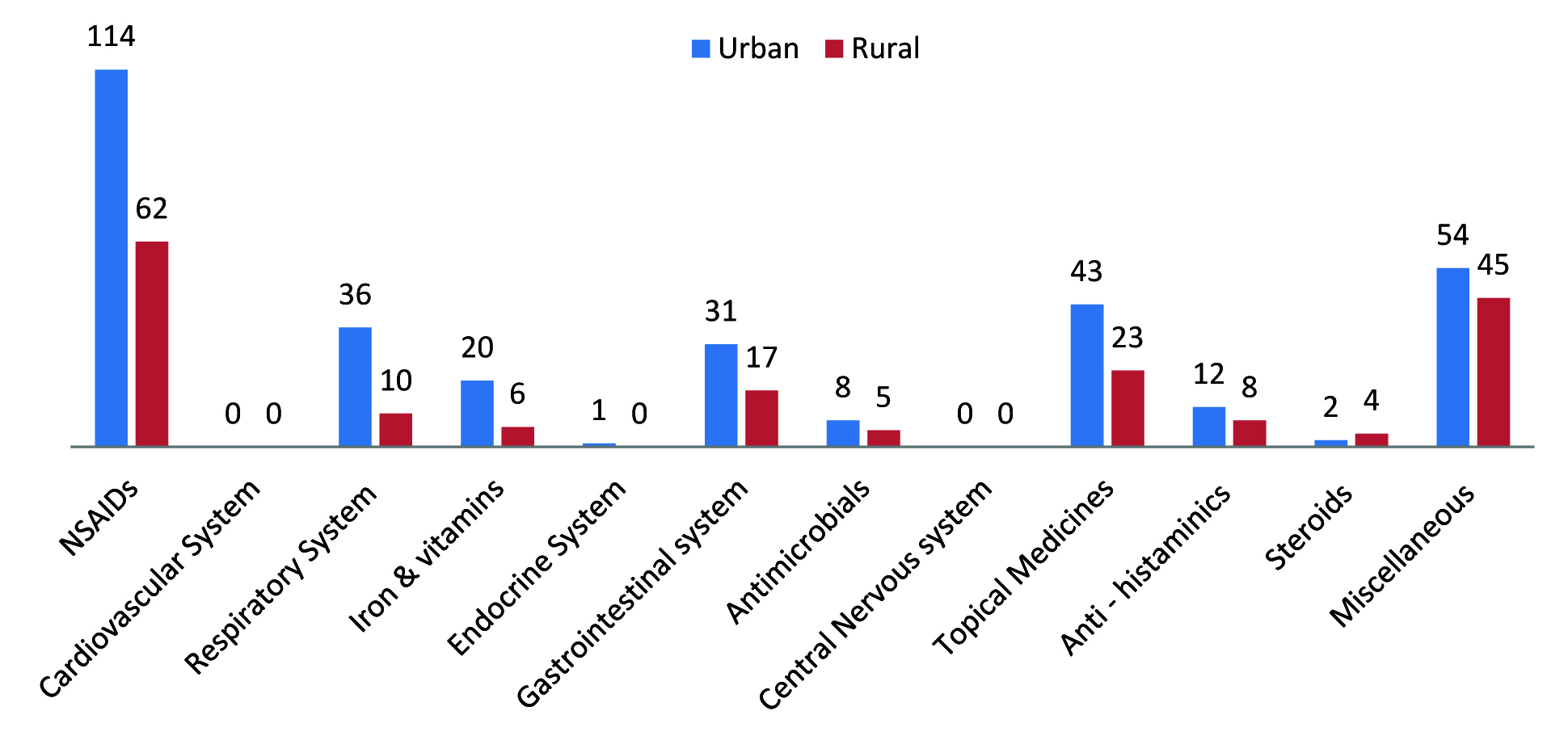
Considering the availability of medicines according to systemic morbidity, 19.88% medicines were found to be from cardiovascular system, 13.42% were that of (Non Steroidal anti-inflammatory Drugs) NSAIDs and 14.16% were Iron preparations & vitamins having the status with prescriptions. Other less commonly available class of prescribed medicines were for gastrointestinal disorders (9.98%), respiratory disorders (9.67%), antimicrobials (8.61%), topical preparations (7.56%) medicines, endocrine disorders (6.50%), antihistaminic (H1) preparations other than respiratory use (3.85%), medicines for CNS (Central Nervous System) disorders (2.69%), miscellaneous preparations (2.28%), steroids (0.85%) and drugs for arthritis (0.24%) [Table/Fig-2]. NSAIDs were the major group available without prescription (35.13%) followed by miscellaneous preparations which includes other system medicines (19.76%), topical preparations (13.17%), medicines for gastrointestinal disorders (9.58%), for respiratory disorders (9.18%), Iron preparations & vitamins (5.19%), antihistaminic (H1) preparations other than respiratory use (3.99%), steroids (1.2%) and endocrine disorders (0.2%) which can be seen in [Table/Fig-3]. Antimicrobials were found in very less number (2.59%) among the without prescription medicines.
Class wise distribution of medicines with prescription available at home.
Class wise distribution of medicines without prescription available at home.
Out of the total 3438 medicine formulations, 100 (2.91%) had been found with package inserts, and 101 (2.94%) were expired. More prescription medicines found with package inserts in rural area (3.2%) than in urban (1.2%) while more number of without prescription medicines was found expired in urban (3.39%) than in rural area (2.86%).
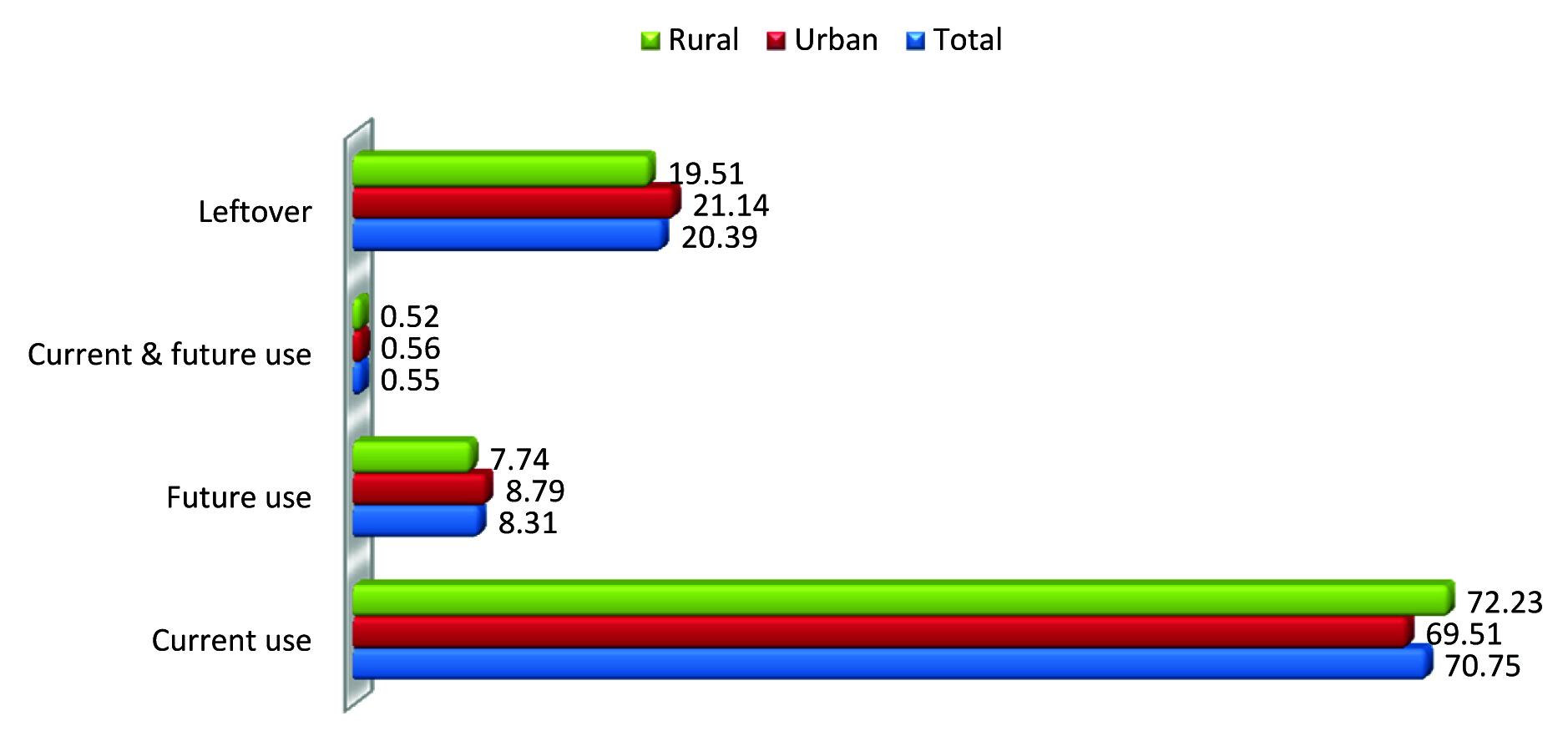
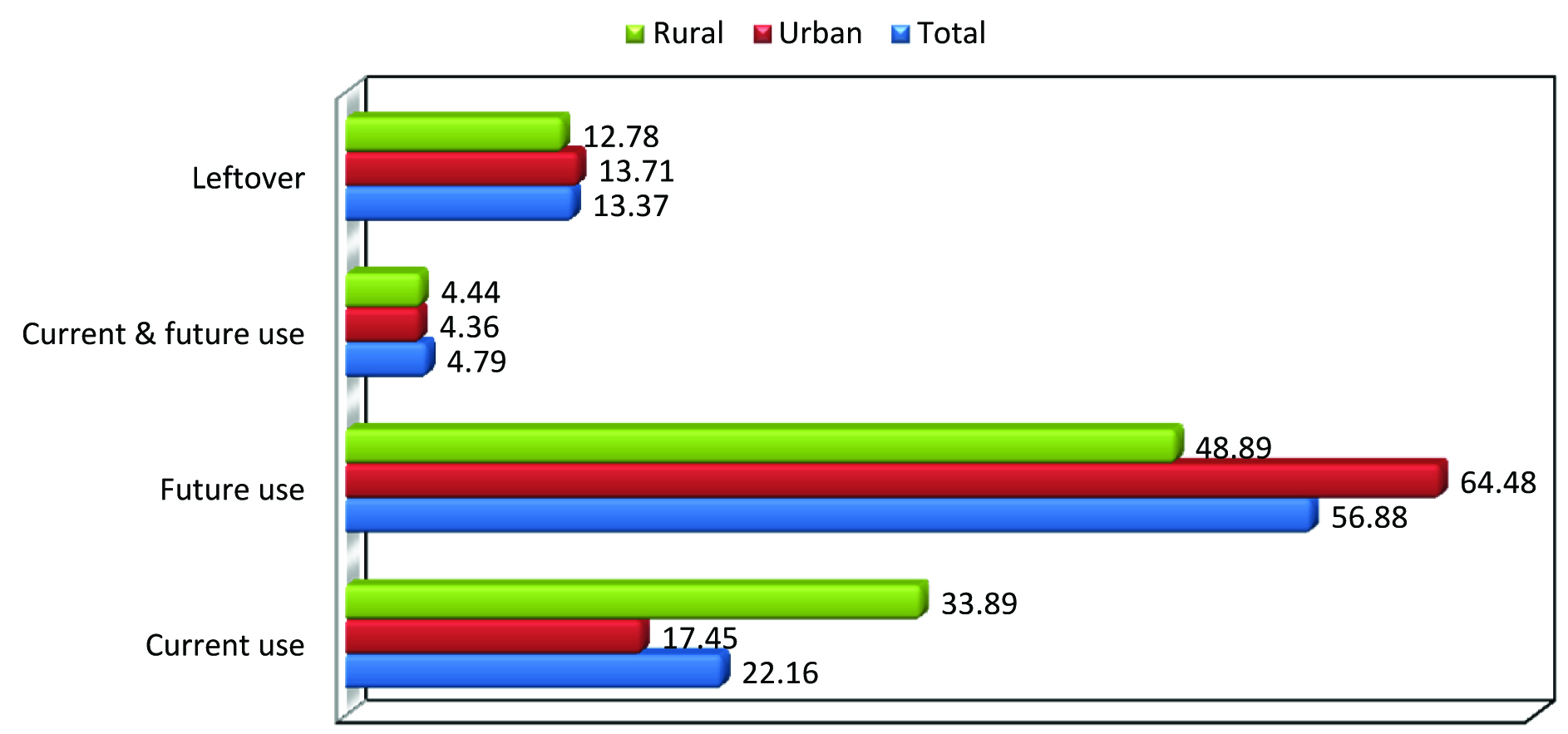
Quite similar results were found in urban and rural areas as far as the current and future use of both prescription as well as non prescription medicines is concerned. The leftover medicines with prescription were 20.39% [Table/Fig-4] and without prescription medicines were 13.37% [Table/ Fig-5].
Percentage of medicines with prescription for current use, future use or leftover.
Percentage of medicines without prescription for current use, future use or leftover.
Adherence with the dose was followed with 69.02% of prescribed medicines while adherence with the duration of the treatment was followed with 73.51% of medicines [Table/Fig-6]. It was noted that 70.86% medicines without prescription were taken in appropriate doses and 72.65% medicines in appropriate duration [Table/Fig-7]. Appropriate dose and duration of medicines were followed more significantly by urban people than the rural. (χ2 = 5.5967, p <0.05 & χ2 = 9.5317, p < 0.05 respectively).
Number of medicines with prescription in relation to adherence of dose and duration of treatment.
| Adherence | Dosen (%) | Duration of Treatmentn (%) |
|---|
| Urban | Rural | Total | Urban | Rural | Total |
|---|
| Yes | 1132(71.02) | 895(66.64) | 2027(69.02) | 1195(74.97) | 964(71.78) | 2159(73.51) |
| No | 462(28.98) | 448(33.36) | 910(30.98) | 399(25.03) | 379(28.22) | 778(26.49) |
| Total | 1594(100) | 1343(100) | 2937(100) | 1594(100) | 1343(100) | 2937(100) |
Number of medicines without prescription in relation to appropriateness of dose & duration of treatment.
| Appropriateness | Dosen (%) | Duration Of Treatmentn (%) |
|---|
| Urbann (%) | Ruraln (%) | Totaln (%) | Urbann (%) | Ruraln (%) | Totaln (%) |
|---|
| Yes | 239(74.45) | 116(64.44) | 355(70.86) | 248(77.26) | 116(64.44) | 364(72.65) |
| No | 39(12.15) | 27(15.00) | 66(13.17) | 30(9.35) | 27(15.00) | 57(11.38) |
| Not known | 43(13.40) | 37(20.56) | 80(15.97) | 43(13.40) | 37(20.56) | 80(15.97) |
| Total | 321(100) | 180(100) | 501(100) | 321(100) | 180(100) | 501(100) |
A total of 43 (1.46%) out of 2937 prescription medicines were identified for self medication, of which 26 from urban and 17 were from rural area. Five medicines (1 from rural & 4 from urban area) among these crossed the expiry dates. Of the total 43 medicine preparations intended as self medication, 5 preparations from urban area were for current use while rest preparations from urban and all preparations from rural area were either leftover/unused and or for future use. Twelve preparations intended for pediatric use were also used for other kids at homes without doctor’s advice.
Discussion
Many drug utilization surveys have been carried out on use of drugs in the population either by telephonic interview or by sending questionnaires to people but there are less studies done through home visits with personal interview.
In this study, we found that there were more number of medicines either prescribed or without prescription available in urban than rural houses. The average of 4.72 medicines formulations found in our study was quite similar to that of studies done at North Jakarta, Indonesia-4.9, Qatar–6.0, Pakistan-5.13 while it was found to be less in Ethiopia-1.7 and high in Basrah, Iraq-14.26, Brazil-10.9 and Palestine-13.3 [1,2,7–11]. The differences between results may be because of varied study groups and different study settings. There is no similar study available in India for comparing the data of prescribed drugs. A study from Rohtak, India [12] while interview with houses wives, showed that 97% houses to have medicines but only 73% practiced self medication. The difference in the rates of home drug storage could have been due to the unique socio-economic factors and cultural attitudes in Gujarat compared to Rohtak in India and other countries. It may reflect different health seeking habits among different nations. It might also be due to differences in compliance with medications or differences in prevalence of chronic diseases like diabetes mellitus, cardiovascular and respiratory diseases. Sometime patients do not comply with the exact duration of prescriptions, perhaps because of inadequate communication to patients by health professionals which frequently leads to incomplete consumption of medicines with piling up at home. Presence of large family size, insurance coverage, higher economic status, high literacy, without medically related jobs may be responsible for higher storage of medicines in homes. Among the other causes of home storage of drugs may be excessive prescribing, imperfect therapeutic adherence and treatment modifications after hospitalization and oversized drug packages resulting in home storage of leftover drugs.
Solid dosage forms (tablets and capsules) were the major forms of medicines kept at homes which matched with the studies done in Ethiopia, Palestine and Northern Uganda [8,11,13]. This could be due to their ease of administration. The most significant similarity was seen with the use of NSAIDs with that of the study of Northern UAE [14]. They were the major class without prescription medicines. Jogdand SS reported in his study from rural Maharastra [15] that 49.5% were having any type of medicines stored at home at the time of survey and using it as self-medication as and when require, and NSAIDs (42%) were the major group from allopathic drugs followed by antimicrobials (10%). A study from Jamnagar, Gujarat [16] reported with 64% NSAIDS as most commonly used drugs for self-medication. Antimicrobials were very less in number than the studies done in Basrah, Iraq, Nekemte town, Ethiopia and in Sudan [9,17,18]. In spite of ease of availability, they were rarely used as self medication that shows that either people are wiser of taking such medicines or pharmacists are more careful about dispensing them.
It was also found that patients did not comply with the exact dose & duration with 30% prescribed medicines. In Rohtak, India, 59% housewives did not adhere to instructions given by the prescriber regarding dose, frequency of administration and duration of treatment [12]. This might be due to inadequate communication to the patients by health professionals often leading to piling up of these unused medications at home.
The leftover medicines in our study were less in number than the studies of Ethiopia, Basrah, Iraq, Palestine and Northern Uganda [8,9,11,13]. It is also good to note that prescribed medicines intended for self medication was very less in our study i.e. 1.46% than studies done in Belgium, Palestine, North India and Iraq which is 21%, 25%, 73% and 78% respectively [5,11,12,9]. It was reported that the education level was the major factor of self medication in North India [12]. The limited knowledge on proper drug storage & its use and presence of medicines at homes is likely to fuel irrational drug use mainly due to unintentional use among household members [12].
The purpose of the package inserts or leaflets is to provide information essential for the safe and effective use of the drugs, and hence reducing the number of adverse reactions resulting from medication errors [19]. Only about 3% medicines were found with package inserts in our study. Belgium study found it with 82% of medicines [5]. This may be due to the European Medicines Agency (EMA) which amends the regulations of labeling for drug products from time to time. In India, regulations for package insert are provided under ‘Section 6.2’ and ‘Section 6.3’ of ‘Drugs and Cosmetics Act (1940) and Rules (1945)’ [19]. The final amendment to the act had been enforced in 1986. The Drugs and Cosmetics Rules do not specify the user of package insert but it appears to be directed to the healthcare professionals. Also, the text in ‘Schedule Y’ of the rules does refer to package inserts as prescribing information. User testing of labels and package inserts are mandatory in many countries, but not in India [19]. So it was perceived that there is a dire need of availability of package inserts along with medicines for the patients and in the most suitable languages for the proper use of medicines.
Another area of concern was the use of preparations crossing the expiry dates amongst the drugs intended for self medication, which might be ineffective or responsible for harmful effects.
Places with high availability of non prescription drugs have emerged as the contributing factors in promoting home drug storage. Socioeconomic factors and cultural attitudes influence the prevalence. The ease of access of medicines from the private sector in the community due mainly to inadequate regulation in addition to higher income among participants potentially influences use of without prescription medicines.
Drug wastage is a direct measure of efficiency and success of overall healthcare system. Drug wastage was accounted for 2-3% of all drug costs representing more than $ 1 billion in drug wastage in elderly population in the United States (US) [20]. Unused/leftover medications at home are the results of excessive buying of OTC drugs, self-discontinuation and expiration of drugs which is responsible for wastage of drug at home. Drug wastage can lead to delay in-treatment, disease progression, and treatment of ensuing complications that include exacerbation or prolongation of illness, uncontrolled chronic disease, hospitalization, disability and death adding to overall increase in cost of treatment. It is definitely advisable to clear the medication cabinet of expired medications at least annually if not more often.
Possible impact of inappropriate use or reuse of expired or leftover medicines especially prescription medicine by self or other person are adverse drug reactions, drug- drug interaction, development of antibiotic resistance, addiction/misuse of medicines, ineffective treatment with potentially prolonged illness, chances of poisoning and may harm fetus if taken during pregnancy and in addition to those, the financial loss.
In countries, such as Australia, New Zealand, Finland, France, Sweden and the UK, there is a graduation in the level of availability of nonprescription products. There can be some sub-divisions in the nonprescription category such as a “behind the counter” class – where there is a need for pharmacist assistance; pharmacy “self-selection”, or “general sale” through any retail outlet [21]. The phrase “OTC” has no legal recognition in India so the list of OTC drugs is obtained through exclusion method means, the drugs which are not in Schedule H or G is OTC [22]. Provision of awareness to the communities on the risks of drug usage especially on self-medication through health campaigns in addition to drug regulation may be a better approach. Both the problems of self-medication and non-compliance warrant more efforts to educate and to avoid the irrational use of drugs. The need for public educational efforts on the rational use of medicines with respect to appropriate drug use, safety, expiry date and appropriate storage at home is required to obtain both economic and health benefits. Further in depth studies may be required to have complete picture on utilization at homes.
Limitation
Since the interviewers were fully aware of the purpose of the project, a few information regarding medicines were not shared which might have lead to skewed result. However, this limitation does not underscore the importance of the findings. The observations made from the study, at least, provide the links for future similar studies while providing the base line information for future comparison.
Conclusion
The evaluation of utilization of medicines, in urban and rural population describes high drug storage, inappropriate use of medicines specially NSAIDs as a major class without prescription drugs. This study also indicates that leftover medications at home may also be a potential risk for health of people which are not properly addressed. This suggests the need to educate the patients and their relatives about proper and rational use of medicines.
There remains a major role of health care professionals at all levels right from doctors, pharmacists, nurses to health care workers in increasing awareness of general population on appropriate use of drugs. For this, we recommend to develop drug information centers in all hospitals and health centers and awareness programs which can enhance the proper way of using medicines.