Chronic Otitis Media (COM) is a long standing infection of a part or the whole of the middle ear cleft, which is divided into two types – Tubotympanic or safe and Atticoantral or unsafe [1]. Bone destruction, seen in unsafe COM mainly involves the ossicles. The frequency of involvement of different ossicles varies in different studies but incus seems to be the most frequently involved ossicle [2].
A number of histopathological changes develop in the middle ear in COM. An insight into these histological changes in COM can improve clinicians’ diagnostic and therapeutic capabilities by enabling more rational decisions regarding selection of cases and surgical techniques to optimize control of disease and restoration of hearing [3].
As discussed above that incus is most frequently involved ossicle so, an investigation of the histopathological changes in incus was carried out in the anticipation that such a study would aid in the determination of mechanism of the destructive process and might help in the decision of type of surgical procedure as well as in developing new therapeutic interventions to prevent the changes occurring in the bone.
The aim of this study was to conduct the histology of normal incus and report the structural changes occurring in it in chronic otitis media.
Materials and Methods
Ten normal incuses were collected from cadavers in the Department of Anatomy, Guru Gobind Singh Medical College, Faridkot and studied histologically. The findings were compared with ten incuses which were removed during the surgery for COM (seven cases with cholesteotoma and three without cholesteotoma) in the Department of ENT, Guru Gobind Singh Medical College, Faridkot. The specimens were decalcified in formic acid (10-15 %) for one week in electric bone decalcifier by putting in a cassette for 3-4 hours daily. Then the specimens were processed in the series of alcohol and xylene. Then were embedded in paraffin wax overnight, cut into the sections of 5 micron thickness. Later the slides were prepared and were again processed in series of alcohol and xylene in reverse manner. Finally, they were stained with haematoxylin and eosin stains. All the specimens were examined under the microscope under 10X and 40X magnification.
Results
Normal structure of Incus
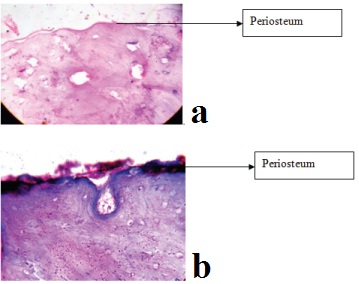
The normal specimens of incus collected from the cadavers were examined. In these specimens, the periosteum consisted of a narrow fibrous layer covered by mucosal lining of simple squamous epithelium with numerous capillaries [Table/Fig-1a,b].
Periosteum of normal ossicle covered by simple squamous epithelium seen under 10X, haematoxylin and eosin stained.
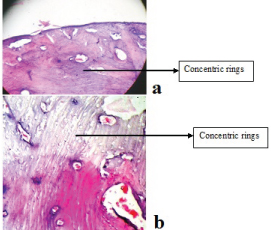
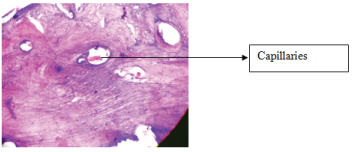
The body and the processes of the ossicle showed compact bone with concentric rings seen in irregular fashion [Table/Fig-2a,b]. The body of incus contains many marrow spaces. The spaces contain a network of fine connective tissue with network of capillaries [Table/Fig-3].
Normal incus showing compact bone pattern of concentric rings seen under 40X, haematoxylin and eosin stained.
Spaces showing network of capillaries seen under 10X, haematoxylin and eosin stained.
Histopathological changes
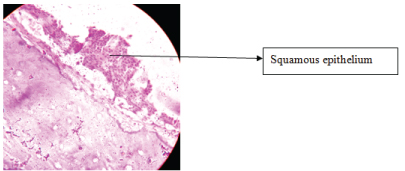
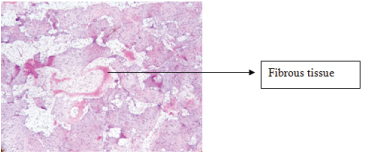
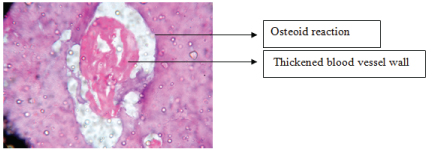
Pathological incuses of COM (both with and without cholestoetoma) were collected from ENT department and were examined. These incuses demonstrated certain changes. The epithelium over the periosteum was not seen in some of the specimens. This is thought to have been due to alterations during processing and due to preparation of the specimen. But in most of the specimens, the epithelium was observed to be stratified squamous type [Table/Fig-4]. The significant changes found in the osseous spaces seemed to be increased and distorted [Table/Fig-5]. The fibrous tissue often occupied the spaces in the bone [Table/Fig-6]. The blood vessels in the spaces were observed with thickened endothelial lining [Table/Fig-7]. The normal architecture of the bone i.e., the concentric rings were seen distorted. Osteocytes were found absent in the lacunar spaces. The free margin of the destroyed bone showed an osteoid reaction [Table/Fig-7].
Pathological specimen showing stratified squamous epithelium seen under 10X, haematoxylin and eosin stained.
Concentric rings distorted with increased osseous spaces seen under 10X, haematoxylin and eosin stained.
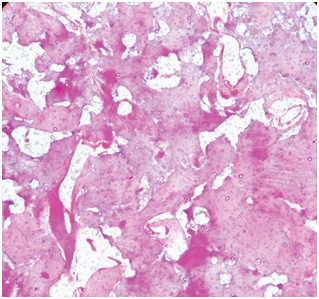
Spaces filled with fibrous tissue seen under 10X, haematoxylin and eosin stained.
Thickened blood vessels seen under 40X, haematoxylin and eosin stained.
Discussion
The ossicles of middle ear are commonly involved in COM. The frequency of involvement of ossicles vary in different studies but incus seems to be most frequently involved [2], particularly long process of incus [4,5]. Incus showed higher destruction in adults than children [6]. Histopathological studies of the ossicles of the middle ear in COM have not been carried out so frequently. So, the study was conducted to understand the changes occurring in the miniature bone, i.e., incus involved in COM. To understand the pathogenesis of the ossicular changes in the otitis media, we must be familiar with the structural aspects of a normal incus bone.
The specimens seen in our study had the periosteum with the fibrous layer consisting of simple squamous epithelium. Maximow and Bloom [7] also claimed it as simple squamous epithelium. According to Eggston and Wolff [8], this epithelium made up of simple nonciliated cells having no basement membrane. Ash and Raum [9] explain it as flattened cuboidal cells.
Gruber emphasized the structural identity of ossicles and long bones [10]. Grippaudo considered ossicles as long bones in miniature [11]. Attanasio et al., studies also showed the structure of incus similar to that of long bone with lamellar pattern [12]. In our study, the body and the processes of the ossicle seen are made up of compact bone with the concentric rings seen. The body contained many marrow spaces, which is in accordance with Frederic J. Pollock., who claimed the head of malleus and body of incus too contains marrow spaces [13]. According to Eggston and Wolff, the stapes contains no marrow spaces [8].
Long back, it was reported that the ossicles in middle ear may become diseased in COM. With long standing disease, the body of incus gets involved, according to Schwatze [14]. Frederic J. Pollock also claimed incus to be most frequently involved bone in COM [13]. Grippaudo said that involvement of incus indicates the greater extent of disease [11], could be because of its poorer vascularity and cancellous nature. Nager and Nager explained it by following individual sections in the serial sections of temporal bone and observed that a single branch of anterior tympanic artery, called as ossicular artery, supplies the outer ossicles [15]. This ossicular artery divides into two branches, one supplying the malleus and other incus. The vessels to long process of incus have convolutions as it traverses the marrow spaces. The mucosal network over long process of incus seldom sends vessels into the bone. Because of this meager vascular supply, chronic inflammation of marrow spaces through which blood vessel courses, may lessen the vascularity of long process and may be a factor in its subsequent destruction and dissolution.
Cristina explained incus to be most commonly affected ossicle due its incudal mass, its prominent bone marrow and mainly due to exposure and fragility of its long apophysis and its lenticular process [6].
According to Gruber and Jackson, malleus and incus were involved equally in the disease [10,16] where as Schwatze, claimed malleus to be more often affected than incus [14]. Many authors like, Grippaudo, believe the stapes to be least commonly affected [11].
The specimens taken in the present study were the incuses from COM, both, with and without cholesteotoma. The changes found in both the groups were similar. Grippaudo and Pollock also described the changes in ossicles in COM as same with and without cholesteotoma [11,13] whereas Sade and Berco’s claimed the epithelial lining of ossicles in simple COM to be cuboidal or respiratory epithelium [17].
The changes described by Pollock in the diseased incus go parallel to those reported in this study [13]. The epithelium over the periosteum changed to stratified squamous. He claims this metaplastic alteration to be a protective mechanism resulting from chronic irritation of inflammation.
Grippaudo and Pollock state the changes in the osseous spaces to be enlarged, often filled with fibrous tissue along thickened blood vessels and destruction of bone adjacent to marrow spaces, which is also visible in this study. It seems to be an attempt to repair the eroded bone [11,13].
Sade and Berco’s findings suggests that the ossicular bone destruction in the middle ear were either surrounded by granulation tissue or by the connective tissue along osteoid reaction seen at the margins of the destroyed bone [17]. Though osteiod reaction was seen in our specimens, but the granulation tissue was not appreciated.
In certain diseased cases, incuses after removal from epitympanum, is used as bone graft after careful sculpturing the bone. The newly prepared graft is tightly fitted between the stapes and malleus [18]. The commonly used autograft material is the body of incus [12]. These chronically infected incuses include the histological changes in middle as well as peripheral regions. So, use of incus autografts, as prosthesis in type III tympanoplasties, to reconstruct ossicular chain, is debatable and needs further elaborative study due to less number of specimens in the present study.
Limitation
The only limitation of the study is small sample size as we could not get many incuses of pathological conditions. The probable result is, therefore, needed to be studied at larger scale.
Conclusion
The architecture of the normal incus is found to be similar as that of any long bone of the body. The histological study of pathological ossicles, removed from the cases of chronic otitis media, demonstrated increased marrow cavities, distorted concentric ring pattern and osteoid formation which were seen in peripheral as well as in the body of incus. So, the use of incus as autografts may jeopardize the whole surgery and may predispose to the reoccurrence of the disease. Therefore, as per our study, the reuse of incus is questionable and synthetic prosthesis should be preferred.