Hypospadias is a congenital anomaly of the urogenital tract which results from an arrest in normal development of urethra, foreskin and ventral aspect of the penis. The phenotype ranges from a mild degree with distal glanular meatus to severe cases with ambiguous genitalia. The incidence is 3.2 per 1000 live male births [1]. The ideal time to correct primary hypospadias is when aged 6-12 months. However, in some developing countries, such as ours, this anomaly may be left untreated until adulthood. A multifactorial aetiology including genetic, endocrine and environmental factors are considered to be involved in the genesis of this anomaly [2]. There is a definite role of paternal abnormalities like scrotal or testicular defect, low sperm motility and abnormal sperm morphology in genesis of hypospadias [3], but the fertility potential of hypospadiac patient has not been clearly defined. The sexual function of patients who have either paediatric or adult hypospadias correction remains one of the enigmatic problems frequently raised by patients. As the child grows into adulthood, sexual function becomes an important issue. There are only few studies in the literature that focus on the sexual function, semen quality and reproductive hormonal profile, the results of these studies are somewhat discordant [4–8]. All these studies were done in group of adult hypospadiac patients who were operated in childhood. To the best of our knowledge, a study assessing the fertility potential in hypospadiac patients, who were operated in adulthood is not available. We hereby attempt to evaluate the fertility potential in hypospadiac patients as compared to age matched healthy controls along with effect of age of surgical correction over fertility potential in hypospadiac patients.
Materials and Methods
The present study was carried out in the Department of Urology, SMS Medical College Jaipur, Rajasthan, India from September 2013 to December 2015. After ethical clearance from the institutional ethics committee, 86 cases of adult hypospadiac patients with Tanner stage 5 [9] at the time of evaluation were included in this study. Out of 86 patients, 56 were operated during the above study period and rest 30 patients were taken from urology outpatient department clinic, who were operated during childhood and attended the clinic for a variety of reasons, including renal calculus disease, minor degree of lower urinay tract symptoms, symptoms of non-specific flank pain or infertility. All these 30 patients were selected on the basis of discharge card provided by them. Patients with urethral stricture and multiple urethrocutaneous fistula were excluded. Seventy age matched sexually active patients suffering from renal stone disease, hydronephrosis or unilateral non-functioning kidney with normal serum creatinine admitted in urology ward were enrolled as control group.
All the participants enrolled in this study were explained about the study and then informed written consent was taken. Then they underwent thorough physical examination to rule out any associated genitourinary abnormality.
All patients of hypospadias were broadly divided into two groups according to the location of meatus:
- Proximal hypospadias if the meatus was at perineal, scrotal, penoscrotal or proximal penile location and
- Distal hypospadias if the meatus was at midshaft, distal penile, subcoronal or glanular location.
Penile size and circumference measurements were done by participants themselves both in flaccid and erect position in a warm and quiet room as per instruction given to them. Penile length was defined as the linear distance from the penopubic skin junction to the mid of glans, which was measure by flexible measuring tape over dorsal aspect of penis. The penile circumference was measured at the middle of the shaft by a flexible measuring tape. The erected penile length and circumference were measured at full erection without using any pharmacological agents after self stimulation in private room. In order to reduce errors in measurements, two measurements were taken by same method at different times and mean value was recorded.
Testicular size measurement and detection of other associated genitourinary tract abnormalities were done by ultra-sonographic examination.
All participants underwent semen analysis after 3 days of sexual abstinence. The semen sample was collected through masturbation into a special container provided in laboratory room itself to avoid any delay in semen analysis.
Blood samples was drawn between 9 AM to 11 AM from cubital vein of each participant and then send to reproductive laboratory where it was centrifuged and the serum was separated and frozen at -200C. The serum level of Follicular Stimulating Hormone (FSH) (normal 0.7 to 11.1 mIU/ml), Luteinizing Hormone (LH) (normal 0.8 to 7.6 mIU/ml and testosterone (normal 262 to 960 ng/dl) were analysed using a immunoflourometric assay.
A set of questionnaire was given to all the participants which included information regarding causes of late surgical attention, the penile erectile function according to a 5-item version of the International Index of Erectile Function (IIEF-5), ejaculatory function- as a projectile or non-projectile and the strength of libido (scored as follow: very low, low, moderate, high and very high; patients were given score of 1-5). The overall satisfaction after penetrating intercourse (very dissatisfied, dissatisfied, inconclusive, satisfied and very satisfied; patients were given score of 1-5) were recorded for both participants and their partners.
The group of adult hypospadias patients operated during adulthood underwent same physical examination, lab investigation and a set of questionnaire twice, first at the time of admission and second minimum 3 months after surgery. During follow-up 2 patients did not reported and 11 patients were excluded from the study due to post surgical complication. Final statistical analysis was done between total of 73 hypospadiac patients and 70 controls.
All the parameters of hypospadiac patients (after corrective surgery either in childhood or in adulthood) were compared with control. Preoperative and postoperative parameters of that group of hypospadiac patients who were operated during adulthood were compared separately to rule out effect of surgical correction. To rule out the effect of age of surgical correction, all the parameters of the patients operated during childhood were compared with patients who were operated during adulthood after minimum of 3 months of follow-up (mean-13.93 months). Data were analysed using Students t-test, Paired t-test, Chi-square test and one-way ANOVA, as appropriate, with p<0.05 considered statistically significant.
Results
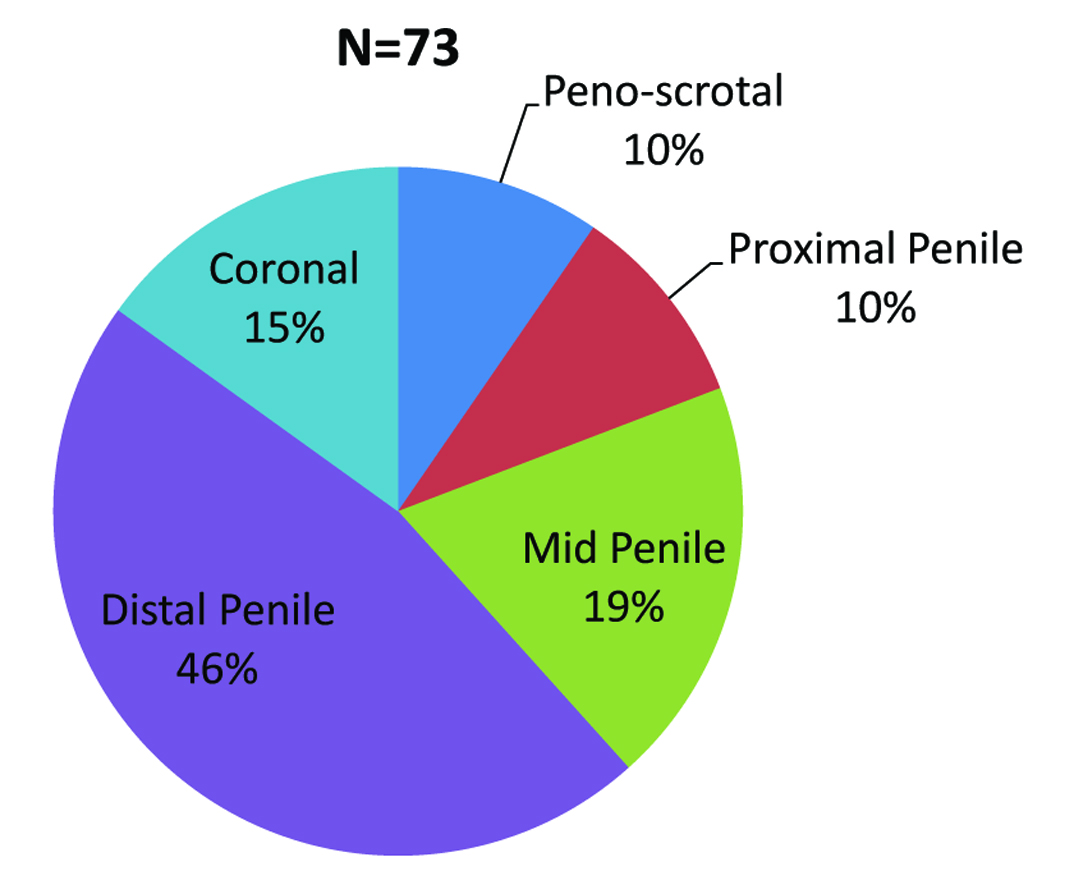
There were 73 patients of adult hypospadias with a mean age of 23.73 years (range 18 to 50) and with mean BMI of 21.09 (range 17.6 to 32.4) out of which 7(9.59%) had peno-scrotal, 7(9.59%) proximal, 14(19.18%) mid penile, 34(46.58%) distal penile, and 11(15.07%) coronal hypospadias [Table/Fig-1]. General characteristic of patients and controls were comparable as shown in [Table/Fig-2].
Distribution of hypospadiac patients according to location of external urethral meatus.
Comparison of general characteristics, sexual function parameters, semen parameters and serum reproductive hormonal profile status of adult hypospadiac patients and age-matched control.
| Characteristics | Hypospadias (n=73) | Controls (n=70) | p-value | PH(n=14) | p-value | DH (n=59) | p-value |
|---|
| Mean age (years) | 23.73 ± 6.06 | 23.74 ± 3.55 | 0.984 | 27.29±8.73 | 0.014 | 22.88±4.97 | 0.317 |
| Body weight (kg) | 60.51 ± 6.56 | 60.04 ± 6.57 | 0.674 | 63.00±8.87 | 0.125 | 59.92±5.83 | 0.912 |
| Height (cm) | 169.32 ± 4.78 | 169.04 ± 4.98 | 0.740 | 167.93±5.1 | 0.437 | 169.6±4.6 | 0.487 |
| BMI (kg/m2) | 21.08 ± 1.93 | 21.00 ± 1.89 | 0.791 | 22.27±2.43 | 0.022 | 20.80±1.70 | 0.554 |
| Flaccid penile length (cm) | 7.92 ± 1.33 | 10.78 ± 0.94 | <0.001 | 6.93±0.87 | <0.001 | 8.16±1.32 | <0.001 |
| Erected penile length (cm) | 9.62 ± 1.31 | 13.15 ± 1.15 | <0.001 | 8.86±0.56 | <0.001 | 9.80±1.37 | <0.001 |
| Flaccid penile circumference (cm) | 9.03 ± 0.74 | 8.96 ± 0.59 | 0.58 | 9.10±1.04 | 0.475 | 9.01±0.67 | 0.714 |
| Erected penile circumference (cm) | 10.69 ± 0.68 | 10.60 ± 0.51 | 0.366 | 10.54±0.72 | 0.717 | 10.73±0.67 | 0.230 |
| Testicular volume (ml) | 23.81 ± 1.23 | 23.91 ± 1.39 | 0.630 | 23.86±1.02 | 0.882 | 23.80±1.28 | 0.614 |
| Strength of libido* | 4.56 ± 0.50 | 4.56 ± 0.50 | 0.957 | 4.64±0.49 | 0.560 | 4.54±0.50 | 0.868 |
| Erectile function | 22.40 ± 2.20 | 23.14 ± 0.83 | 0.009 | 19.43±3.15 | <0.001 | 23.17±0.88 | 0.918 |
| Sexual satisfaction (patient)¥ | 4.66 ± 0.58 | 4.77 ± 0.48 | 0.235 | 4.50±0.65 | 0.087 | 4.70±0.57 | 0.488 |
| Sexual satisfaction (partner)¥ | 4.68 ± 0.58 | 4.70 ± 0.52 | 0.803 | 4.57±0.64 | 0.429 | 4.70±0.57 | 0.971 |
| Semen volume (ml) | 1.58 ± 0.50 | 1.70 ± 0.62 | 0.192 | 1.25±0.58 | 0.006 | 1.66±0.45 | 0.642 |
| Sperm concentration (mill/ml) | 58.88 ± 20.18 | 68.67 ± 17.38 | 0.002 | 27.57±10.39 | <0.001 | 66.31±13.73 | 0.386 |
| Active motile sperm (%) | 57.40 ± 17.42 | 65.36 ± 8.90 | 0.001 | 33.21±11.86 | <0.001 | 63.14±13.06 | 0.259 |
| Normal morphology (%) | 73.22 ± 6.08 | 76.71 ± 5.50 | <0.001 | 65.71±6.46 | <0.001 | 75.00±4.45 | 0.064 |
| FSH (m IU/ml) | 4.20 ± 2.67 | 2.27 ± 0.94 | <0.001 | 5.26±2.30 | <0.001 | 3.95±2.71 | <0.001 |
| LH (m IU/ml) | 5.12 ± 3.44 | 3.21 ± 1.13 | <0.001 | 6.45±7.42 | <0.001 | 4.80±1.37 | 0.001 |
| Testosterone (ng/dl) | 465.74 ± 153.21 | 570.67 ± 125.40 | <0.001 | 459.3±152.5 | 0.008 | 467.2±154.6 | <0.001 |
Data are expressed as mean ± SD, *Range 1-very low to 5 very high, ¥ Range 1-very unsatisfied to 5-very satisfied, PH- Proximal hypospadias, DH- Distal hypospadias.
Mean penile length of surgically corrected hypospadiac patients under both flaccid and erect conditions (7.92±1.33 and 9.62±1.31 cm) were significantly shorter than those of control (10.78±0.94 and 13.15±1.15 cm) (p<0.001), however there was no statistically significant difference with respect to mid penile circumference [Table/Fig-2]. Shortening of penile length was more affected in proximal type than in distal. There was no significant difference regarding strength of libido in between hypospadiac patients and control (p>0.05), however erectile function (IIEF-5 score) was poor in proximal type [Table/Fig-2]. Level of satisfaction of hypospadiac patients and their opposite partner after penetrating intercourse were comparable to control (p>0.05) [Table/Fig-2].
Proximal type of hypospadiac patients had poor semen parameters like semen volume(ml), sperm concentration (mill/ml), active sperm motility (%), and normal sperm morphology as compared to control (p<0.05). Over all hypospadiac patients had poor semen parameters like sperm concentration (mill/ml), active sperm motility (%), and normal sperm morphology as compared to control (p<0.05) except the semen volume and these parameters were poorer in the proximal group, whereas all the above semen parameters were comparable between distal hypospadias group and control (p>0.05) [Table/Fig-2]. However, all these semen parameters were comparable between distal hypospadias group and control (p>0.05) [Table/Fig-2].
Regarding reproductive hormonal profile, the serum FSH and LH level were significantly high and serum testosterone level was significantly low in hypospadiac patients than control (p<0.001) [Table/Fig-2]. However, all the above hormonal profiles were within normal limits in hypospadiac patients. In spite of hormonal discrepancy, there was no significant difference in testicular size between hypospadiac patients and control [Table/Fig-2].
We also compared the above parameters between patients operated during childhood or during adulthood separately. In childhood operated group, there were total 30 patients out of which 23.33% had proximal hypospadias in the group of patients operated during childhood where as out of 43 patients in adulthood operated group out of which 16.27% had proximal hypospadias in the group of patients operated during adulthood. All the parameters were comparable between these two groups except penile length which were shorter in childhood operated group [Table/Fig-3].
Comparison of parameters of sexual function, semen analysis and serum reproductive hormonal profile between the group of hypospadiac patients operated during childhood and adulthood.
| Parameters | Operated in childhood (n=30) | Operated in adulthood (n=43) | p-value |
|---|
| Flaccid penile length (cm) | 7.45 ± 0.77 | 8.26 ± 1.54 | 0.010 |
| Erected penile length (cm) | 9.13 ± 0.86 | 9.97± 1.47 | 0.007 |
| Flaccid penile circumference (cm) | 9.07 ± 0.55 | 9.00 ± 0.86 | 0.711 |
| Erected penile circumference (cm) | 10.60 ± 0.57 | 10.76± 0.74 | 0.339 |
| Testicular volume (ml) | 23.93± 0.86 | 23.72 ± 1.43 | 0.473 |
| Strength of libido* | 4.60 ± 0.49 | 4.53 ± 0.50 | 0.587 |
| Erectile function | 22.04 ± 2.47 | 22.63 ± 2.00 | 0.278 |
| Sexual satisfaction (patient)¥ | 4.63 ± 0.68 | 4.68 ± 0.521 | 0.718 |
| Sexual satisfaction (partner)¥ | 4.63 ± 0.68 | 4.71 ± 0.512 | 0.595 |
| Semen volume (ml) | 1.50 ± 0.39 | 1.64 ± 0.57 | 0.250 |
| Sperm concentration (mill/ml) | 59.10 ± 21.74 | 58.72 ± 19.28 | 0.938 |
| Active motile sperm (%) | 57.83 ± 19.05 | 57.09 ± 16.41 | 0.860 |
| Normal morphology (%) | 72.17 ± 8.06 | 73.95 ± 4.16 | 0.220 |
| FSH (m IU/ml) | 4.64 ± 2.59 | 3.89 ± 2.72 | 0.236 |
| LH (m IU/ml) | 4.71 ± 1.43 | 5.40 ± 4.33 | 0.400 |
| Testosterone (ng/dl) | 459.87 ± 163.28 | 469.84 ± 147.61 | 0.787 |
Data are expressed as mean ± SD, *Range 1-very low to 5 very high, ¥ Range 1-very unsatisfied to 5-very satisfied
After comparing the pre-operative and post-operative data of all after minimum 3 months of post-operative follow-up (mean-13.93 months) in the group of 43 patients operated during adulthood, there were significant improvement in the size of penis both in flaccid and erect conditions, erectile function scores (IIEF-5), level of sexual satisfaction both in patients and partners and semen volume after surgical correction [Table/Fig-4].
Comparison of pre-operative and post-operative parameters of sexual function, semen analysis and serum reproductive hormonal profile in adult hypospadiac patients operated during adulthood.
| Pre-operative (n=43) | Post-operative (n=43) | p-value |
|---|
| Flaccid penile length (cm) | 8.15 ± 1.46 | 8.26 ± 1.54 | 0.011 |
| Erected penile length (cm) | 9.73± 1.47 | 9.97± 1.47 | <0.001 |
| Flaccid penile circumference (cm) | 8.96 ± 0.85 | 9.00 ± 0.86 | 0.083 |
| Erectrd penile circumference (cm) | 10.74± 0.72 | 10.76± 0.74 | 0.323 |
| Strength of libido* | 4.49 ± 0.50 | 4.53 ± 0.50 | 0.160 |
| Erectile function | 22.29 ± 2.40 | 22.63 ± 2.00 | 0.007 |
| Sexual satisfaction (patient)¥ | 4.39 ± 0.62 | 4.68 ± 0.521 | <0.001 |
| Sexual satisfaction (partner)¥ | 4.54 ± 0.55 | 4.71± 0.51 | 0.007 |
| Semen volume (ml) | 1.09 ± 0.39 | 1.64 ± 0.57 | <0.001 |
| Sperm concentration (mill/ml) | 58.74 ± 19.20 | 58.72 ± 19.28 | 0.931 |
| Active motile sperm (%) | 57.35 ± 15.87 | 57.09 ± 16.41 | 0.547 |
| Normal morphology (%) | 73.84 ± 4.05 | 73.95 ± 4.16 | 0.767 |
Data are expressed as mean ± SD, *Range 1-very low to 5 very high, ¥ Range 1-very unsatisfied to 5-very satisfied
Overall, mode of ejaculation was projectile in most of hypospadiac patients (65/73, 89.04%). The group of patients in which it was non-projectile (8/73, 10.95%), majority were from proximal group (5/8, 62.5%). Out of these 8 patients, 4(50%) patients were from the group operated during childhood (4/30, 13.33%).
Surgical correction of hypospadias in adulthood led to improvement in mode of ejaculation, before surgical correction non-projectile ejaculation was present in 11 (11/43, 25.58%) patients, majority were in proximal hypospadias (6/11, 54.54%) which was reduced to 4 (4/43, 9.30%) after surgical correction. Out of these 4 patients, 3 were from proximal group (75%). There were no other genitor-urinary abnormalities in our study population. Most of the patients in our study group who consulted for surgical correction during adulthood (57.14%) were referred from the armed forces recruitment board for medical fitness. They all had distal type of hypospadias.
Discussion
Proper development of penis is one of the most important sign of normal sexual development in male. In hypospadiac patient’s smaller penile size may be the single reason for dissatisfaction with penile appearance and it may be due to multiple factors like lower level of androgens, presence of undescended testis, surgical trauma and incomplete correction of penile curvature. The reports on degree of severity of hypospadias on penile development have varied among different studies [10–12]. These studies showed that proximal hypospadiac patients had a decreased average penile length compared with distal hypospadiac patients and there were significantly shorter penile length and circumference under both flaccid and erect conditions in hypospadiac patients. In current study the findings were little bit discordant, average penile length in hypospadiac patients under both erect and flaccid conditions were significantly shorter than those of control but penile circumference under both flaccid and erect conditions were comparable to control. Similar to previous studies [10–12] penis of patients with proximal type group were significantly smaller than distal type group.
Excellent libido and good quality of penile erection are most important parts of successful sexual life. In current study hypospadiac men reported an excellent strength of libido as control, meaning that original penile deformity does not have any influence on the strength of libido. The quality of erection was comparable between patients of distal type group and control, however it was significantly poor in proximal type of patients group. This was consistent with the findings in recent literature [10,13,14]. Overall level of satisfaction of patients and their partners in sexual activity did not differ significantly from control and this is consistent with previous studies [4,10,15]. This finding indicates that hypospadias and its related surgery did not alter the overall sexual function.
Adequate quantity of semen deposition in female genital tract is very important to make the ova fertilize and it depends up on the mode of ejaculation of male partner. Similar to previous studies [13,14,16] ejaculation difficulties in the form of weak or dribbling ejaculation or having to milk out ejaculate after intercourse occurred more frequentely in proximal hypospadiac patients (5/73,6.84%%) than in distal type group of hypospadiac patients (3/73,4.10%). These problems may be due to insufficient support of spongiosum tissue, skin folds, associated urethral diverticulae, abnormal development of prostate and seminal vesicles or higher occurrence of postoperative uretheral stricture.
There are only few studies related to reproductive hormonal profile status in adult hypospadias, the results of these studies are somewhat discordant [8,17]. In our study the mean value of both serum FSH and LH were significantly higher where as mean value of serum testosterone level was significantly lower in hypospadiac patients than controls (p<0.05) although these hormonal levels in all patients were within normal limits. Hormonal discrepancies were more in proximal type group, that may be the reason for poor semen quality.
Regarding semen analysis our findings were similar to study done by Asklund et al., semen parameters like semen volume, total number of sperm per ml, active sperm motility and normal morphology were similar in distal type group of hypospadiasc patients and control, but these parameters were significantly abnormal in proximal type group of hypospadiac patients (p<0.05) [7].
After comparing the data between proximal and distal type of hypospadiac patients group, it became more evident that proximal type of patients group were more affected in view of shorter penile length, IIEF-5 score, reproductive hormonal profile and poor quality of semen parameters. This may result in poor fertility potential in proximal type group of hypospadiac patients. However, there was no difference in testicular volume, strength of libido and level of sexual satisfaction between the groups.
When data were compared between patients operated in childhood and patients operated in adulthood, it was found that all the variables were comparable between these two groups except the penile length which was shorter in patients operated in childhood. These may be due to higher percentage of proximal hypospadiac patients in this group. To conceive, this parameter is not significant.
In the group of 43 patients operated during adulthood, preoperative and postoperative variables were compared. Significant improvement in length of penis both in flaccid and erect conditions and erectile function score (IIEF-5) may be due to surgical correction of associated penile curvature present during preoperative period. Improvement in semen volume may be due to improvement in mode of ejaculation from non-projectile to projectile after surgical correction (74.41% to 90.69%).
Conclusion
In our study, fertility potential parameters in distal group of hypospadiac patients were comparable with control. However, it was significantly poor in proximal group of patients. Patients operated in either childhood or in adulthood, there was no significant differences in the capability of being a father. Our results should be reassuring for patients with distal hypospadias and they can be informed that adult with hypospadias of this type has fertility potential similar to adult without hypospadias. However the proximal type had poor erectile function and semen quality. Patients operated in either childhood or in adulthood, there was no significant difference in fertility potential noted. More studies are needed to confirm the above findings.
Data are expressed as mean ± SD, *Range 1-very low to 5 very high, ¥ Range 1-very unsatisfied to 5-very satisfied, PH- Proximal hypospadias, DH- Distal hypospadias.
Data are expressed as mean ± SD, *Range 1-very low to 5 very high, ¥ Range 1-very unsatisfied to 5-very satisfied
Data are expressed as mean ± SD, *Range 1-very low to 5 very high, ¥ Range 1-very unsatisfied to 5-very satisfied