Rare Offshoot of a Common Malady Anaemia and Tuberculosis
Gautham Kolla1, Vishak Acharya2, Prashantha Balanthimogru3, Arun Mani4, Shehzad Ruman5
1 Junior Resident, Department of Internal Medicine, Kasturba Medical College (KMC), Mangalore, Karnataka, India.
2 Professor and Head, Department of Pulmonary Medicine, Kasturba Medical College, Mangalore, Karnataka, India.
3 Senior Resident, Department of Medicine, Consultant; Department of Hematology, Kasturba Medical College, Mangalore, Karnataka, India.
4 Senior Resident, Department of Pulmonary Medicine, Kasturba Medical College, Mangalore, Karnataka, India.
5 Junior Resident, Department of Internal Medicine, Kasturba Medical College, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Gautham Kolla, S/O K. Ashok Kumar, Plot no-84/A, G-1, Road no-11, Nagavilla Apartments, Filmnagar, Jubilee Hills, Hyderabad, Telangana -500096, India.
E-mail: kollagautham@gmail.com
Haematological manifestations are one of the rarer presentations of tuberculosis and are usually of normocytic normochromic type. An association of Autoimmune Haemolytic Anaemia (AIHA) with active pulmonary tuberculosis is an exceeding rare entity, though anaemia and tuberculosis commonly co-exist. We report a patient with sputum negative pulmonary tuberculosis with associated Coomb’s positive AIHA. The patient responded well to Anti- Tubercular Therapy (ATT) and low dose steroids tapered over a month.
Acid fast bacilli, Anti tubercular therapy, Autoimmune haemolytic anaemia
Case Report
A 32-year-old Indian female presented with complaints of cough with mucoid expectoration with occasional streaks of blood since 1 month accompanied by on and off fever since 15 days. She complained of easy fatigability, decreased appetite and weight loss of 2 kilograms. There was no past history of tuberculosis or contact with tuberculosis patients. She had no associated co-morbidities.
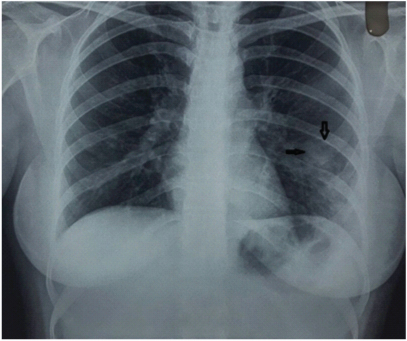
On examination, she was afebrile, had a pulse rate of 82/min, blood pressure of 130/80 mm Hg and respiratory rate 18cycles/ min. She was pale with no icterus, cyanosis, clubbing, lymphadenopathy and pedal oedema. Breath sounds were decreased over left mammary area with crepitations. Spleen was enlarged 2cm below left costal margin. Chest radiograph showed left lower zone in-homogenous opacity with air bronchogram suggestive of consolidation [Table/Fig-1].
Chest radiograph at the time of admission, consolidation is seen in left lower zone as depicted by an arrow.
Initial laboratory parameters revealed Haemoglobin of 9.3g/dl, with a total WBC count of 10,200 /mm3 (neutrophils of 64%, lymphocytes of 32 %), raised Erythrocyte Sedimentation Rate (ESR) of 83 mm/hour, peripheral blood smear revealed spherocytes, RBC agglutinates, and overall picture was suggestive of Auto immune Haemolytic Anaemia (AIHA).
Sputum sample was negative for Acid Fast Bacilli (AFB) and no organism were isolated on culture. Ultrasonography of the abdomen revealed mild splenomegaly (13cm). Direct Coomb’s test was positive. Indirect Coomb’s test was negative. Lactate dehydrogenase (752) and reticulocyte count (10) was elevated. Serum iron and unbound iron capacity were within normal limits. Total iron binding capacity was slightly decreased.
C-reactive protein was positive (23.69 mg/litre). C3 levels, serum uric acid, liver and renal functions were normal. Urine and stool routine were normal. No G-6PD deficiency was detected. Serologic tests for Anti-nuclear Antibody (ANA), Mycoplasma, Human immunodeficiency virus, Hepatitis B and C virus, Cytomegalovirus, Ebstein Barr virus were negative. Blood culture was also negative.
Bronchoscopy was done and lavage was sent for analysis. Bronchial lavage for AFB stain was negative. However, Mycobacterium tuberculosis was detected on Gene Xpert with no resistance to Rifampicin. Subsequent AFB culture was positive, and pyogenic culture revealed no growth. Patient was started on anti-tubercular therapy.
Haematologist opinion was sought in view of AIHA and high reticulocyte count - Use of low dose steroids was advised along with anti-tubercular therapy. However, pulsed steroid therapy was avoided in view of underlying active tuberculosis.
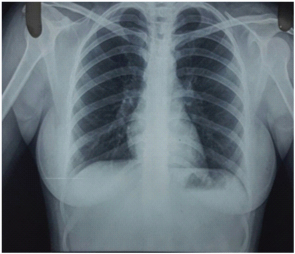
She was discharged with tapering dose of steroids over a month. Haematological parameters improved after one and a half month of anti-tubercular therapy. Haemoglobin improved from 8.4 mg/dl to 13.4 mg/dl, ESR reduced to 6mm/hour, Coomb’s test became negative and left lower zone opacity on Chest radiograph cleared [Table/Fig-2].
Chest radiograph during follow up, resolution of consolidation.
Discussion
AIHA represents a spectrum of disorders in which antibodies against self antigens on erthyrocyte membrane causes a shortened RBC life span. AIHA can occur as idiopathic (primary) disorder or can coexist with another disease (secondary) [1]. The incidence of AIHA is estimated to be approximately 0.8 in one lac population per year, the prevalence being 17 in one lac population per year [2].
Tuberculosis presents with a wide variety of haematological manifestations. The prevalence of anaemia among tuberculosis patients ranges between 30%-94% [3]. Anaemia in tuberculosis often gets corrected with treatment of tuberculosis and mostly does not require specific interventions, the most common being normocytic normochromic anaemia of chronic disease. In a study done by Bashir et al., 34% of tuberculosis patients had anaemia of chronic disease, 24% had iron deficiency anaemia, 16% had severe iron deficiency anaemia, 5% had macrocytic anaemia, 18% had normocytic normochromic anaemia [3].
Presence of haemolytic anaemia is extremely rare in tuberculosis though cases have been reported with anti tubercular drugs like rifampicin, isoniazid, Para Amino Salicylic Acid (PAS). Many mechanisms of anaemia in tuberculosis were proposed and exact aetiology is not known. There might be suppression of erythropoiesis by inflammatory response mediators like cytokines, inhibitory effects of tumour necrosis factor alpha (TNF-α) which is released during inflammation. Other causes are nutritional deficiency, malabsorption syndrome, failure of iron utilization, bone marrow suppression [1].
There is no known exact aetiopathogenesis of tuberculosis patients manifesting with haemolytic anaemia, however, previous studies suggested that haemolytic anaemia and other manifestations like pancytopenia, myelofibrosis could develop with the injection of tubercle bacilli or their products [4]. In our study and other previous studies, response of AIHA to ATT suggests the possible aetiological role of tuberculosis in pathogenesis of AIHA. AIHA is exceedingly rare in tuberculosis. As per our knowledge, till date only few cases of AIHA associated with tuberculosis have been reported. Amongst these, majorities were extra pulmonary or disseminated tuberculosis [4].
Previous studies concluded that tuberculosis with AIHA improved with ATT alone [5], some improved with combination of ATT and steroids, some even required blood transfusions as well in addition to anti-tubercular therapy [2], some patients had miliary tuberculosis with AIHA who responded to anti-tubercular therapy alone [6] and childhood tuberculosis with AIHA responded to both ATT and steroids combination [7].
Such an association of AIHA with tuberculosis may have therapeutic implication. In the presence of active tuberculosis, use of high dose steroids (like in pulse therapy) can be detrimental to the patient. The cases mentioned in [Table/Fig-3] where pulmonary tuberculosis was the site, had either sputum/bronchial lavage smear tested positive for acid fast bacilli or tuberculosis was confirmed by imaging. Our study had both sputum and bronchial lavage smear negative for acid fast bacilli; gene Xpert was positive for tuberculosis. ATT was started before culture for AFB report came and Coomb’s test was negative within a month of starting ATT. The rarity of our case is the unusual presentation of AIHA in patient with smear negative but culture positive and Gene Xpert positive pulmonary tuberculosis, which has not been reported so far to the best of our knowledge.
Case reports of tuberculosis and AIHA in India and elsewhere in last decade.
| Main Author/Year/Place | Sex/Age | Site | Treatment |
|---|
| Gupta [8]/2005 (India) | Male/8 | Abdominal | ATT, Glucocorticoids |
| Khemiri [9]/2008(Tunisia) | Female /11 | Pulmonary | ATT |
| Nandennavar[1]/2011(India) | Female /19 | Lymph-nodal | ATT |
| Wu [10] /2012 | Female /24 | DisseminatedTuberculosis withMycoplasmapneumonia | ATT/Packed red bloodcell transfusion |
| Kumar [11]/2013(India) | Male/23 | Endobronchial(biopsy from lesionpositive for AFB) | ATT |
| Safe [12]/2013 (Brazil) | Female/18 | Disseminated | ATT/Packed red bloodcell transfusion |
| Somalwar [13]/2013 (India) | Male/22 | Disseminated | ATT/Packed red bloodcell transfusion/Glucocorticoids |
| Bahbahani [4]/2014 (Kuwait) | Female/24 | Disseminated | ATT/Glucocorticoids/Packedred blood cell transfusion |
| Anurag/Richa [2]2015 (India) | Female /25 | Pulmonary | ATT/ Packed red bloodtransfusion |
Conclusion
Although rare, AIHA should be considered in the differential diagnosis of anaemia in tuberculosis patients. Also, our study highlights the need of a detailed evaluation for detecting pulmonary tuberculosis when there is strong clinical suspicion even though sputum was negative. The patient responded to ATT along with low dose steroid tapered over a month implying the effectiveness of ATT for treatment of AIHA in tuberculosis patients. AIHA with active tuberculosis often gets corrected with treatment and resolution of tuberculosis as in our case possibly implicating a more complex association that needs more studies to unearth this cause affect association.
[1]. Nandennavar M, Cyriac S, Krishnakumar TG, Immune haemolytic anaemia in a patient with tuberculous lymphadenitisJournal of Global Infectious Diseases 2011 3(1):89 [Google Scholar]
[2]. Anurag L, Richa C, Cold agglutinin induced haemolytic anaemia in a patient with pulmonary tuberculosisInt J Med Res Health Sci 2015 4(4):911-12. [Google Scholar]
[3]. Bashir BA, Abdallah SA, Mohamedani AA, Anaemia among patients with pulmonary tuberculosis in port sudan, eastern sudanInternational Journal of Recent Scientific Research 2015 6:4128-31. [Google Scholar]
[4]. Bahbahani H, Al-Rashed M, Almahmeed M, Tuberculosis and autoimmune haemolytic anaemia: Case report and literature reviewJournal of Applied Haematology 2014 5(4):164 [Google Scholar]
[5]. Turgut M, Uzun O, Kelkitli E, Özer O, Pulmonary tuberculosis associated with autoimmune haemolytic anaemia: an unusual presentationTurk J Haematol 2002 19(4):477-80. [Google Scholar]
[6]. Kuo PH, Yang PC, Kuo SS, Luh KT, Severe immune haemolytic anaemia in disseminated tuberculosis with response to antituberculosis therapyCHEST Journal 2001 119(6):1961-63. [Google Scholar]
[7]. Bakhshi S, Rao IS, Jain V, Arya LS, Autoimmune haemolytic anaemia complicating disseminated childhood tuberculosisThe Indian Journal of Pediatrics 2004 71(6):549-51. [Google Scholar]
[8]. Gupta V, Bhatia BD, Abdominal tuberculosis with autoimmune haemolytic anaemiaThe Indian Journal of Pediatrics 2005 72(2):175-76. [Google Scholar]
[9]. Khemiri M, Zouari S, Barsaoui S, Autoimmune bicytopenia in pulmonary tuberculosis. Report of a pediatric caseRespiratory Medicine CME 2008 1(4):281-83. [Google Scholar]
[10]. Wu B, Rong R, Cold agglutinin syndrome with severe haemolytic anaemia in a patient diagnosed of disseminated tuberculosis and concomitant Mycoplasma pneumoniae infectionTransfusion Medicine 2012 22(2):151-52. [Google Scholar]
[11]. Kumar S, Kambar VM, Bheemaraya D, Chaitra CS, Autoimmune haemolytic anaemia in a patient with endobronchial tuberculosisJEMDS 2013 17(2):2944-45. [Google Scholar]
[12]. Safe IP, O’brien C, Ferreira FR, Souza ML, Ramasawmy R, Tuberculosis associated with transient haemolytic anaemia responsive to tuberculosis chaemotherapy: a case reportBrazilian Journal of Infectious Diseases 2013 17(1):110-11. [Google Scholar]
[13]. Somalwar A, Aher A, Zanwar V, Kolpakwar K, Tubercular lymphadenitis and abdominal tuberculosis with autoimmune haemolytic anaemia and severe intravascular haemolysisAnnals of Tropical Medicine and Public Health 2013 6(1):123 [Google Scholar]