Acute bronchiolitis is a self limiting lower airway disease affecting infants and children caused by viral infections. RSV is responsible for > 80% of LRTI in infants with male preponderance and has a distinct seasonality feature causing outbreaks during winter and spring, other agents being parainfluenza, adenovirus, mycoplasma, rhinovirus, emerging viruses like human metapneumovirus and human boca virus [1–3]. One prospective, population-based study by the Centers for Disease Control and Prevention showed that the average RSV hospitalization rate was 5.2 per 1000 children younger than 24 months of age during the 5-year period between 2000 and 2005 [4]. Most clinicians recognize bronchiolitis as a constellation of clinical signs and symptoms, affecting children younger than 2 years, presenting with rhinorrhoea, cough and mild fever followed by increased respiratory effort manifested as grunting, nasal flaring, and intercostal and/or sub costal retractions: tachypnea, wheezing, rales. The infant may also have features of irritability, poor feeding, and vomiting. Though, in majority of cases, the disease remains benign, and recovery starts in 3-5 days, some of these children may continue to worsen. Especially those with various co-morbidities like underlying chronic lung disease, congenital heart disease or immuno- compromised state [5]. The course of bronchiolitis is found to be variable and dynamic, it can start from transient events, such as apnea, to progress to respiratory distress from lower airway obstruction. Pulse oximetry is useful in deciding about the need for supplemental oxygen. The chest may be hyperresonant to percussion. On auscultation wheezes and fine crackles may be heard throughout the lungs. Severely affected patients may have grunting, marked retractions, cyanosis and may have impaired perfusion. Apnea may occur in those born prematurely and in younger than two months of age [6].
Various studies done involving the detection of virus conducted on infants hospitalized for bronchiolitis have consistently found that 60% to 75% have positive test results for RSV, and have coinfections in up to one-third of infants. Infants with Non-RSV bronchiolitis, have been found to have a shorter course and also are found to represent a different phenotype associated with repeated wheezing [7–9]. Routine virologic testing is not recommended except for deciding the discontinuation of palivizumab prophylaxis for an infant hospitalized with bronchiolitis, where it is performed to determine if RSV is the aetiologic agent. If a break through RSV infection is determined to be present based on antigen detection or other assay, prophylaxis should be discontinued because of the very low likelihood of a second RSV infection in the same year [10].
This study was undertaken to analyse the demographic characteristics, clinical features and, haematological profile of bronchiolitis. To compare the findings of demographic characteristics, clinical features and haematological profile between RSV and Non-RSV bronchiolitis, in order to find out, is there any difference in presentation among both the groups so that the parents can be counselled, regarding the severity, hospital stay, morbidity and mortality and if possible to see on follow up how many develop wheezing and other complications and which group they belong to.
Materials and Methods
This prospective study was conducted from January 2015 to December 2015, in the Department of Paediatrics of Chettinad Hospital and Research Institute. Children of age of 1 month to 3 years admitted in paediatric intensive care unit with features of bronchiolitis were included in the study [10]. Children with congenital heart disease, chronic lung disease, family history of asthma and other chronic diseases were excluded and also age < 1 month who were admitted in neonatal intensive care unit, were not included in the study.
After taking informed consent, 2 ml venous blood was drawn and sent for analysis for haemoglobin, total leucocyte count, and platelet count by CBC counter method. Demographic, clinical information and haematological profile was recorded in standardized proforma. Then, nasopharyngeal specimens were obtained with nasopharyngeal swab with a flexible shaft within 24 hour of admission. Specimens were kept in viral transport medium and transported to Serum Institute Guindy, where Real Time PCR (Polymerase Chain Reaction) was performed to identify RSV.
Initially all cases were kept in paediatric intensive care and they received oxygen and hypertonic saline nebulisation with continuous vitals monitoring, if they did not respond, then a trial of bronchodilator and steroids were given and if features of leucocytosis, or if X-ray showed opacities, antibiotics was started. Duration of hospital stay and outcome was noted. Demographic, clinical and haematological data of the two groups of RSV and Non RSV was compared. Institutional ethical committee clearance was taken.
Operational definition: Bronchiolitis [11] The American Academy of Paediatrics (AAP) defines bronchiolitis as ‘acute inflammation, oedema and necrosis of epithelial cells lining small airways, increased mucus production, and bronchospasm’. Clinical signs and symptoms of bronchiolitis consist of rhinorrhea, cough, wheezing tachypnea and increased respiratory effort manifested as grunting, nasal flaring, and intercostal and/or subcostal retractions.
Sample size and sampling method: The present study sample was based on the number of cases that were admitted in the PICU, with features of bronchiolitis and who gave consent for the study, during study period of 1 year.
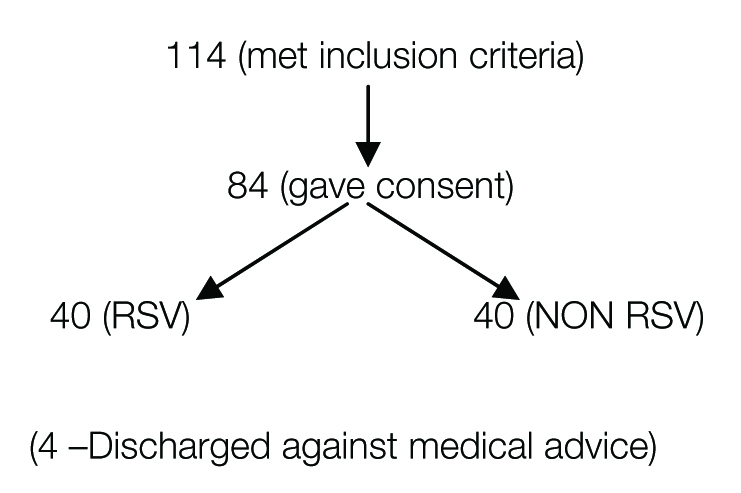
Total children who met the inclusion criteria during study period of 1 year were 114, among them 84 of them met inclusion criteria and also gave consent for the study, at the end it was found 44 cases were RSV bronchiolitis and 40 were Non RSV group among which 4 of them got discharged against medical advice, hence remaining 40 cases were compared with Non RSV group [Table/Fig-1].
Flowchart explaining distribution of patients.
Statistical Analysis
RSV positivity was the primary explanatory variable. Various clinical, laboratory and clinical outcome related parameters and duration of hospital stay were compared between the two study groups. For categorical variables, frequencies and percentage were used. Quantitative variable were presented as mean and standard deviations. The differences in the proportions and mean values were compared using chi square test and independent sample t-test respectively and corresponding p-values were presented. p-value < 0.05 was taken as statistically significant. IBM SPSS version 21.0 and micro soft excel 2010 were used fro analysis.
Results
A total of 80 children were included in the final analysis out of which 40 (50.0%) were RSV group and the remaining 40 (50.0%) were Non RSV group. Demographic profile analysis showed that the proportion of children below 1 year was slightly higher in RSV group. There was no statistically significant difference between the two groups in terms of gender, gestational age, smoking exposure and socio economic status as shown in [Table/Fig-2].
| Demographic Features | RSV (N=40) | | Non RSV (N=40) | | p-value |
|---|
| Number | % | Number | % | |
|---|
| Age |
| 1month-6months | 7 | 17.5 | 7 | 17.5 | 0.661 |
| 7months-1yr | 6 | 15.0 | 4 | 10.0 |
| 1yr-1yr6m | 9 | 22.5 | 5 | 12.5 |
| 1yr7m-2yrs | 8 | 20.0 | 11 | 27.5 |
| 2yr-3yrs | 10 | 25.0 | 13 | 32.5 |
| Sex |
| Male | 24 | 60.0 | 20 | 50.0 | 0.369 |
| Female | 16 | 40.0 | 20 | 50.0 |
| Gestational Age |
| <37wk | 9 | 22.5 | 8 | 20.0 | 0.785 |
| >37wk | 31 | 77.5 | 32 | 80.0 |
| Smoking Exposure |
| Yes | 23 | 57.5 | 18 | 45.0 | 0.263 |
| No | 17 | 42.5 | 23 | 55.0 |
| SES |
| Class II | 3 | 7.5 | 1 | 2.5 | 1.000 |
| Class III | 18 | 45 | 19 | 47.5 |
| Class IV | 19 | 47.5 | 20 | 50.0 |
Clinical profile analysis showed 50% of Non RSV cases had fever (>100.40F) and 30% of RSV cases had fever when temperature was measured during the first 24 hours of admission.
Statistically significant difference was also observed in proportion of subjects with wheeze (89.7% vs 41.5%, p-value < 0.001). No statistically significant difference was observed in other clinical parameters and also in any of the vital signs, including, heart rate, respiratory rate, blood pressure and Sp02 between the study groups [Table/Fig-3].
| Clinical Features | RSV (N=40) | Non RSV (N=40) | p-value |
|---|
| Number | % | Number | % |
|---|
| Symptoms |
| Fever | 12 | 30.0 | 20 | 50.0 | 0.068 |
| Rhinorrhoea | 40 | 100.0 | 40 | 100.0 | - |
| Cough | 40 | 100.0 | 40 | 100.0 | - |
| Distress | 40 | 100.0 | 39 | 97.5 | 0.314 |
| Vomiting | 40 | 100.0 | 40 | 100.0 | - |
| Signs |
| Tachypnea | 40 | 100.0 | 40 | 100.0 | - |
| Chest Indrawing | 40 | 100.0 | 40 | 100.0 | - |
| Cyanosis | 1 | 2.5 | 0 | 0 | 0.314 |
| Wheezing | 35 | 89.7 | 17 | 41.5 | <0.001 |
| Vital Signs | Mean | SD | Mean | SD | |
| Heart Rate | 110.45±17.42 | 113.47±17.26 | 0.438 |
| Respiratory Rate | 57.27±7.41 | 57.37±7.24 | 0.951 |
| Systolic BP | 87.77±6.73 | 87.77±6.73 | 1.000 |
| Diastolic BP | 59.55±3.66 | 59.55±3.66 | 1.000 |
| Spo2 | 96.000±1.64 | 96.000±1.55 | 1.000 |
There were no statistically significant differences between the two study groups in total leucocyte count, platelet count and serum electrolytes. The proportion of neutrophils was significantly higher in RSV negative group, compared to RSV positive group (45.64% vs 37.46%, p-value 0.074) [Table/Fig-4]. There was no statistically significant difference observed between the two groups, in culture results and radiological finding in chest X-ray [Table/Fig-5]. Statistically significant differences were observed in the treatment of study groups. Higher proportion of RSV negative subjects received bronchodilator nebulization, steroid and antibiotic therapy [Table/Fig-6]. The hospital stay was significantly higher in RSV positive cases, compared to RSV negative cases (5. 57 days vs 4.67 days, p-value <0.001). None of the study participants met with mortality [Table/Fig-6].
| Tests | RSV (N=40) | Non RSV (N=40) | p-value |
|---|
| Mean± SD | Mean± SD |
|---|
| HB % | 10.60±0.93 | 10.87±0.91 | 0.185 |
| Total Leucocyte Count | 11597.50±4404.45 | 11990.00±3876.15 | 0.438 |
| DC-N | 37.46±19.43 | 45.64±20.72 | 0.074 |
| DC-L | 59.30±12.26 | 55.67±11.95 | 0.184 |
| Platelet | 5.75±1.000 | 5.77±0.99 | 0.951 |
| Tests | RSV (N=40) | Non RSV (N=40) | p-value |
|---|
| Number | % | Number | % |
|---|
| Blood Culture |
| Ng | 34 | 85.0 | 34 | 85.0 | 1.000 |
| Cons | 6 | 15.0 | 6 | 15.0 |
| Chest X-Ray |
| Hyper Inflation | 33 | 82.5 | 31 | 77.5 | 0.838 |
| B/L Para Card Opac | 5 | 12.5 | 6 | 15.0 |
| Right Para Card | 2 | 5.0 | 3 | 7.5 |
| Treatment | RSV (N=40) | Non RSV (N=40) | p-value |
|---|
| Number | % | Number | % |
|---|
| Non Invasive |
| Nrbm | 20 | 50 | 17 | 42.5 | 0.509 |
| Face Mask | 18 | 45 | 17 | 42.5 |
| Nasal Prongs | 2 | 5.0 | 6 | 15.0 |
| Mechanical Ventilation | 0 | 0% | 0 | 0% | - |
| Hypertonic Saline Neb | 40 | 100.0 | 40 | 100.0 | - |
| Bronchodilator Neb | 16 | 40.0 | 25 | 62.5 | 0.044 |
| Steroid | 9 | 22.5 | 25 | 62.5 | <0.001 |
| Antibiotics | 7 | 17.5 | 22 | 55.0 | <0.001 |
| Outcome | Mean ± SD | Mean ± SD | p-Value |
| Hospital Stay | 5.57±0.75 | 4.67±1.02 | <0.001 |
| Mortality | 0% | 0% | – |
Discussion
Acute bronchiolitis is an important cause of morbidity in infants and children and also the most common cause of hospitalization in children presenting an acute lower respiratory tract infection, So this prospective study was done to analyse the demographic characteristics, clinical features and haematological profile of children with bronchiolitis and the findings were compared between RSV and Non –RSV Bronchiolitis.
Bronchiolitis typically affects children younger than two years with a peak incidence between two and six months of age [5]. In our study, it was found that major age group affected was <1year mean age being 7.3 ± 2, with males being affected more among both the groups without any difference and this was comparable to various studies like Syed et al., study that showed 80% of infants were in the age group 30-90 days, with male preponderance, this was because the cases included were < 90 days infants [12], Saleh ahmed conducted retrospective study on 70 children with RSV bronchiolitis, whose records showed major age group affected was < 6months, with males being more common [13]. Hemalatha et al., conducted a cohort study with 126 children with lower respiratory infection among them 56 were RSV positive and 70 were negative, most common age group was < 1 year, males were predominantly affected [14]. Iqbal et al., conducted a study with 107 children where mean age was 11.3 ± 5 months and male to female ratio was 1.3 [15]. Durani et al., in his prospective cohort study showed that the mean age of patients was 5 months and 57% were male [16].
In our study, clinically most of them presented with cough and respiratory distress, with wheezing being more common among RSV group. In Syed et al., study again, cough was the predominant symptom and wheezing predominant sign, similar to our study [12]. Respiratory distress as chest retractions was more common presentation in the records as studied by Saleh ahmed [13]. Iqbal et al., in his study also showed that, among total of 107 children, 91% had respiratory distress at the time of presentation [15]. Durani et al., in his prospective cohort study with children < or = 36 months of age, showed that combination of cough, wheezing and retractions predicted RSV infection in infants and young children [16]. None of the studies showed any difference in clinical presentation based on the aetiological agent.
Fever (>100.40F) as shown by temperature measured during the first 24 hours of admission was more common among Non RSV group as compared to RSV group in our study This difference may be explained based on the day of admission to hospital as counted from the first day of viral prodrome, may be children of Non RSV group presented earlier to the hospital or have not received any antipyretics which we have not noted in our study but other studies have shown that infants with bronchiolitis may have fever or a history of fever. High fever is uncommon in bronchiolitis [17–19].
In our study, investigations like chest X-ray showed hyperinflation predominantly, which is common feature in bronchiolitis and haematological profile showed reactive thrombocytosis which was seen in both groups, with no significant difference between both the groups but, Efraim et al. in his prospective study, found that thrombocytosis was significantly higher in RSV positive group [20].
Most of the RSV group responded well to oxygen and hypertonic saline nebulisation, whereas Non RSV needed bronchodilator, steroids and antibiotics. Duration of stay was prolonged in RSV group and no mortality was noted among both the groups in our study.
In the study conducted by Syed et al., in infants younger than 90 days, High flow oxygen with nebulization was used in 39 patients. Hypertonic Saline nebulization was used in 38 patients. Of the 141 patients, 111 were initially treated with inhaled bronchodilators and 25 received antibiotics empirically. Mean duration of hospital stay for admitted patients was 7± 4.03 days. All three patients admitted to the PICU needed ventilatory support. No mortality occurred in the study population but this study shows no details regarding the difference among the two groups [12].
In saleh et al., study, all patients received supplemental oxygen, some via nasal cannula and others with oxygen hood, 38.6% of those admitted needed mechanical ventilation. Majority (97.1%) of these children were found to receive inhaled bronchodilators and antibiotics (98.5%) despite the viral aetiology. Half of them also received corticosteroids (61.4%) and antipyretics (50%) and only one mortality was documented [13].
Hemalatha et al., in her study showed that among 104 hospitalised, 99 recovered and five children among them 3 were RSV and 2 were Non RSV had fatal outcomes and died in the hospital [14].
Most of the findings regarding the demographic and clinical profile of our study were similar to other studies but the sample size was relatively more in other studies which may lead to decreased false negatives, but the methodology in majority of studies was retrospective which has its own drawbacks. Inclusion criteria was not mentioned clearly, viral testing also has some differences as some studies used immuoflurescence, others used PCR which have their own sensitivity and specificity.
Limitation
The limitation of our study is the small sample size which may one of the reason for false negatives and also not much of significant difference among the two groups and also we did not follow-up the cases to note which group were prone for recurrent wheezing that may be undertaken in future studies.
Conclusion
Bronchiolitis due to RSV was found to affect more commonly children < 1 year, with male preponderance. An 89.7% of RSV cases had wheeze that was statistically significant. Haematological parameters showed reactive thrombocytosis that was present in both groups with not much of difference in other findings. Percentage of Non RSV subjects who received bronchodilator nebulisation, steroid and antibiotic therapy were higher than RSV subjects. The hospital stay was significantly higher in RSV cases and None of the study participants met with mortality.
As there were no significant differences in clinical parameters among both the groups from our study findings, any child with features of bronchiolitis needs continuous monitoring of vitals along with SPO2 and appropriate supportive therapy as and when required without waiting for any investigations.
Virological testing may help us to counsel the parents regarding the duration of stay which was found to be prolonged in RSV bronchiolitis as per our study which was the only difference among both the groups and if possible the cases needs to be followed up for any occurrence of repeated wheezing episodes, which group they belong to so that counselling can be done on this aspect also.