Introduction
Hypertension (HTN) being one of the important risk factors for Cardiovascular Disease (CVD) is a significant health concern, especially in South-Asian region [1]. A linear correlation exists between high Blood Pressure (BP) and Cardiovascular Events (CVE). Compared to the younger (40-49 years) ones, significant differences exist in the incidence of vascular disease and mortality in middle-age (40-69 years) and old-age (70-89 years) populations [2]. With age, prevalence of HTN, especially systolic HTN increases [3]. Special attention needs to be directed to HTN in young ages (20-40 years) due to lower awareness, need for early treatment and better control of HTN [4]. Further, in absence of evidence from randomized clinical trials on benefits of antihypertensive treatment with drugs among younger individuals [5], HTN in the age group of 20-40 years needs critical reappraisal. Given the high prevalence of HTN in the general population in India, in this review we attempt to provide current evidence and expert opinion on epidemiology, aetio-pathogenesis and treatment of HTN in young (20-40 years) Indians.
Epidemiology
The prevalence of HTN in the general Indian population is reported to be 29.8% [1]. Epidemiological data suggests varying prevalence of HTN in young populations. The large prospective SITE (Screening India’s Twin Epidemic) study reported prevalence of 12.72% (n=918/7212) in individuals below 40 years [6]. Similar results were reported by Prasad et al., with prevalence of 11.91% (n=183/1537) in South Asian young population [7]. Another study from state of Karnataka reported prevalence of 17.7% (n=65/367) in age group of 30-39 years [8]. In apparently healthy young (18-40 years) individuals, Shukla et al., reported HTN prevalence of 11% (n=186/1735) [9]. Similarly, Aggarwal et al., studied young individuals with acute Coronary Artery Disease (CAD) and observed HTN prevalence of 10.66% (n=13/122) in patients without CAD and 19.66% (n=46/234) among those who had CAD [10]. Literature evidence on gender differences in HTN of young Indian is lacking. SITE study finds no significant gender difference in HTN for overall study population [6]. Prasad et al., reported significantly higher prevalence in men (14.30%, n=146/1022) than women (7.18%, n=37/515) in South Asian young adults [7]. Similarly, from Vietnam, Minh et al., reported higher prevalence of HTN in men (10.8%) than women (4.2%) in age group of 25-34 years [11]. A recent analysis in individuals aged18-49 years (mean age 34 years, n=27 081), reported isolated systolic HTN (ISH: systolic BP > 140 and diastolic BP < 90), isolated diastolic HTN (IDH: systolic BP < 140 and diastolic BP > 90) and systolic-diastolic HTN (SDH: systolic BP > 140 and diastolic BP > 90) in 25.3%, 3.7% and 19.8% in men respectively and 12.9%, 2.9% and 9.7% women respectively [12]. Everett et al., found that women are less likely to be hypertensive than men in young age (12% vs 27% respectively) and there is low awareness of HTN amongst both men and women [13].
Need to treat and at what level?
Most guidelines define HTN as elevation of systolic BP ≥ 140 mmHg or diastolic BP ≥ 90 mmHg in adults aged 18 years and above [5,14–17]. In general adult population, BP beyond 140/90 mmHg remains one of the most important multipliers of cardiovascular (CV) risk. The question often asked is “whether elevated BP is equally hazardous in young individuals?” In a large study by Yano et al., a 31-year follow-up of 27,081 young individuals (mean age 34 years, range 18-49 years) reported higher CV disease and Coronary Heart Disease (CHD) mortality in men and women with systolic-diastolic HTN followed by IDH in men and finally, ISH in women for overall study population. In individuals below 40 years, ISH was associated with significantly higher CV mortality in men (p=0.09) whereas significance was not reached in women (p=0.65) [12]. In another study with 25-year follow-up of 10,874 young men (18-39 years), Miura et al., reported progressively increasing risk of CHD mortality with increasing levels of BP (HR: 1.62, 2.51 and 3.60 for hypertension stages 1, 2 and 3 by JNC-VII definition respectively) [18,19]. One may conclude that HTN in young individual needs treatment and it should be prioritized based on BP levels in an individual.
Treating elevated BP is essential since reducing SBP even by 2 mmHg can reduce risk of stroke mortality by 10% and Ischemic Heart Disease (IHD) and other vascular causes by 7% in middle-age individuals [2]. Similar evidence on benefits of antihypertensive therapy in younger individuals is lacking. Even recommendations from recently released Joint National Committee (JNC) – 8 provide grade-A recommendation for 30 years and above but for 18-29 year individuals it is grade-E since it relies on expert opinion [14]. This is probably because most HTN trials with major CV end points have been conducted in patients aged 55 years and above [20]. Thus BP targets that can provide benefit in terms of CV events reduction in young individuals remain uncertain. Recommended target for essential HTN in general population is < 140/90 mmHg [5,14–16]. Should this also be the target for age group 20-40 years or should it be lower? Clearly, the evidence is lacking in support of any target value. Higher BP levels at a young age with longer duration of its effects on vasculature raise certain questions that need to be answered. These include: (a) Is treating to lower targets (<130/90) beneficial?; (b) Will treating HTN in 20s and 30s delay the first occurrence CV events?; (c) Whether drug therapy should be initiated as soon as diagnosis is made? In a cohort study of 1207141 Swedish men with mean age 18.4 years followed for 24 years, a U-shaped relation of systolic BP was observed to total mortality with lowest risk for systolic BP < 130 mmHg whereas diastolic BP threshold for mortality was 90 mmHg [21]. Due to prevailing scarcity of published evidence, we believe initiating therapy (lifestyle ± drugs) at threshold of ≥ 140 SBP or ≥ 90 DBP should be the priority and treating to goal of < 140/90 mmHg should prevail in absence of clear evidence on specific BP goals.
Aetio-pathogenesis and Investigations
Essential HTN is the most common form of HTN in general population accounting for up to 95% cases of HTN [16]. In young individuals also, essential HTN remains the primary diagnosis of HTN. Panja et al., followed individuals in 18-30 year age group from Northern India and observed that essential HTN remained common aetiological group (34.8%) [22]. However, an essential step in management of HTN in the young populations is to rule out secondary causes of HTN. Clinically, a high level of suspicion for secondary HTN is essential in young individuals. Camelli et al., reported common occurrence of secondary HTN before 40 years and observed the prevalence of about 30% [23]. Exclusion of secondary causes of HTN is must in: (a) adults < 40 years; (b) sudden worsening of patients’ condition; (c) uncontrolled HTN with 3 medications; (d) accelerated HTN with or without papilloedema or retinal haemorrhage; or (e) cerebrovascular accident below 50 years of age. HTN is associated with an underlying cause in about five percent of young individuals. Common aetiologies include renal parenchymal disease, renovascular disease, endocrine disorders, vascular conditions and drugs [Table/Fig-1] [24–27]. HTN in pregnancy is a distinct entity that should be one of the causes to be evaluated in young females.
Aetiologies and investigations for secondary HTN in young individuals and drugs responsible for rise in BP [24–27].
| Etiology | Investigations |
|---|
| Renovascular | Renal Parenchymal Disease | Urine Examination, Renal Ultrasound, Biopsy |
| Renal vascular Disease | Renal Ultrasound, Renal Angiography – CT or MRI |
| Endocrine | Hyper- or Hypothyroidism | Thyroid hormone concentration |
| Cushing’s Disease | Dexamethasone suppression test |
| Pheochromocytoma | Concentrations of urinary free catecholamines, metanephrines and vanillylmandelic acid (VMA), MIBG-I 131 (meta-iodobenzylguanidine) |
| Primary aldosteronism | Plasma aldosterone/renin ratio, plasma aldosterone after intravenous saline |
| Hyperparathyroidism | Serum calcium, serum parathyroid hormone |
| Acromegaly | CT brain / MRI, Growth hormone levels |
| Vascular | Coarctation of aorta | Echocardiography, Doppler, CT imaging |
| Other | Obstructive sleep apnea | Polysomnography |
| Drugs | Non-steroidal anti-inflammatory agents (NSAIDs), estrogen, testosterone, steroids, immunosuppressant, carbamazepine, fluoxetine, lithium, tricyclic antidepressants (TCAs), amphetamines, cocaine, sympathomimetic agents, and herbal drugs like ephedra, ginseng, etc. |
Evaluation of Secondary causes of HTN
There is a general agreement that thorough history and accurate clinical examination can give important clues to the underlying cause of HTN. Thus, it is of paramount importance particularly in the young hypertensive patient.
Following examinations are recommended.
Accurate BP measurement in both upper limbs
Leg BP readings
Retinal examination
Abdominal or peripheral bruits
Haemoglobin levels
Complete urine examination
Thyroid function tests
Renal function tests and serum electrolytes
Electrocardiogram
2D Echocardiogram (if possible, a colour Doppler study will help to identify LV diastolic dysfunction)
Among secondary causes, renal disease (parenchymal and vascular) remains most common cause of HTN in young individuals. Observations by Panja et al., suggest that renal disease is the most common aetiology of secondary HTN in young Indians (26.4%) [22]. Ruling out bilateral renal artery stenosis is important in young individuals. It should be suspected in cases of rapidly progressive oligouric renal failure [25]. Non-invasive and invasive tests can help in assessment of renal artery stenosis. Captopril augmented renography, duplex renal ultrasound, Gadolinium-enhanced Magnetic Resonance Angiography (MRI), Computed Tomography (CT) angiography are common modalities for evaluation of renal arteries and renal disease [24,25]. Routine use of renal ultrasound in evaluating every young individual with HTN is debatable. It should be individualized taking in to consideration a strong clinical suspicion and patient’s perspectives.
Stress and HTN in young
Increasing level of stress especially psychological stress could contribute to high BP and HTN. A prospective study of 13-year follow-up of more than 4100 normotensive young individuals (18-30 years) reported that larger BP responses to acute psychological stress predict risk of incident HTN in their mid-life [28]. Thus stress can add to development of HTN. Large number young Indian population is working and they are constantly exposed to certain stress. Study of 1071 young Indians (19-30 years) working at Information Technology/Information Technology Enabled Service industry reports alarming figures. Overall HTN prevalence was 31% and that of pre-HTN was 45.7%. In the age-group of 19-25 and 26-30 years, stage-I HTN was reported in 18% and 23% individuals respectively and stage-II HTN was reported in 5% and 3% individuals respectively [29]. Thus stress especially job-stress can have substantial impact on development HTN in the young.
Pregnancy and HTN
Chronic HTN complicates around five percent of pregnancies, and is likely to be seen more frequently as the age group. Pregnancy induced HTN (pre-eclampsia and eclampsia) is an issue related directly with pregnancy. Elevated BP however may continue in post-partum period and continue as persistent or chronic HTN. Sometimes HTN first noted in pregnancy may be due to secondary causes like renal disease, endocrine diseases and neurological disorders. It is advised to evaluate for secondary causes of HTN in all pregnant females to exclude treatable causes of HTN. HTN before, during and after pregnancy is major contributing factor for maternal and fetal morbidity and mortality [30–33]. Worse still, these patients exhibit increased CV morbidity in the future. Thus young females in reproductive age group should be thoroughly evaluated and treated.
Treatment of HTN without Co-morbidities
Management of HTN is essential. Various guidelines released in recent years provide substantial evidence based recommendations for treating HTN [5,14,15,17]. But advice on management of HTN in the younger age group remains scant and unrecognized. We identify major concerns that need addressal in young Indians. These include use of tobacco including smoking from young age, higher consumption of salt in households, lack of adequate physical activity, unhealthy food habits, increasing levels of obesity, higher levels of stress and lack of adequate sleep. Beside these, some other factors like illicit drug use, use of anabolic steroids and psychiatric conditions also need careful attention. Thus initial treatment of HTN in young should largely be directed towards lifestyle modification.
Lifestyle modification
Tobacco abstention: In a large study on smoking from India, Jindal et al., reported 15.6% prevalence (study sample = 73605) of smoking with higher rates amongst males (28.5%) than females (2.1%). Adjusted odds ratios of any tobacco smoking were 6.068 and 12.154 in the age-group of 25-34 and 34-44 years suggesting substantial rates of smoking in young individuals [34]. Further use of tobacco from early childhood and adolescence poses higher threat of CV risk. Atherosclerotic effects of smoking are well known and need no description here. Availability of tobacco in different forms in India makes tobacco abstention more difficult [35]. Avoidance of tobacco in any form should be promoted and counseled at regular intervals in young hypertensives.
Salt reduction: Mean salt intake on daily basis is higher in Indians. In hypertensives, Radhika et al., reported significantly higher mean daily salt intake (9.9 vs 8.0 g, p<0.0001) and dietary sodium intake (4357 ± 1570mg vs 3607 ± 1209mg, p<0.0001) than normotensives. HTN correlated linearly with increasing quintiles of salt intake [36]. Studies on salt intake in young individuals and especially in Indians are lacking. In a meta-analysis, Strazzullo et al., studied 19 cohort samples from 13 studies involving 177025 participants and reported association of excess salt intake with greater relative risk of stroke (pooled Relative Risk {RR} 1.23, 95% Confidence Interval (CI) 1.06 to 1.43; p=0.007) and CV disease (RR, 1.14, CI 0.99 to 1.32; p=0.07). Most studies involved middle-age population and only few studies involved individuals below 40 years [37]. Given the strong causal association with HTN and CV events and higher mean salt intake in Indian households, lowering salt intake to recommended levels of ≤ 5 gm/day (Campbell 2015) is advised and stressed-on in young individuals.
Change in food, food habits and physical exercise: Restriction of high calorie diet and reducing intake of saturated fatty products should be rigorously advised in young individuals. Alcohol restriction is mandated in young individuals. Minimal consumption of processed foods that are rich in salt, sugar and fats should be promoted [38]. Further, it is advised that parents should follow healthy food habits in their routine to inculcate healthy food habits from childhood [39].
Physical inactivity is very common in Indian population. In Indians aged 20 years and above, Anjana et al., reported physically inactivity in 54.4% individuals (n=7737/14227) [40]. Similarly, Ravikiran et al., reported 61.3% physically inactive individuals aged over 20 years from urban Indian region [41]. Health benefits of physical activity are huge and it is strongly recommended. In a retrospective analysis, Johnson et al., reported that only 55% of young (18-39 years) hypertensives were having documented lifestyle education at 1 year. However, individuals with dyslipidemia or family history of HTN or CAD had higher odds of having lifestyle education and therapy [42]. A moderate intensity exercise for 30-45 minutes five days a week is minimal recommended exercise for all ages with HTN. On average, physical activity reduces systolic BP by 2-5 mmHg and diastolic BP by 1-4 mmHg [43]. One important critical issue is the adherence to physical activity. This is often more challenging in obese individuals. To improve patient adherence to physical exercise, it is advisable to counsel patients on benefits of exercise in increasing energy expenditure, preservation of fat free mass, and its role in maintaining weight loss. Alternatively, cognitive behavioral strategies can be adopted [44].
Each of the interventions described above are linked to benefits beyond HTN control [45]. The United States Preventive Services Task Force (USPSTF) provides grade A recommendation to counseling on tobacco and grade B for counseling on healthy diet and physical activity for individuals with CV risk [45,46]. Thus we advise every physician to effectively recommend lifestyle therapy to young individuals with HTN.
Yoga and meditation: Yoga, together with meditation has been found to effective in controlling blood pressure. This effect may be due to a normalization of autonomic cardiovascular rhythms [47].
The available evidence on yoga has been criticized stating that most studies were not randomized, had smaller sample size, had inadequately described yoga programs and did not use standardized outcomes measures. The benefits also have been found to be modest. But these studies have used only yoga asana, pranayama, and/ or short periods of meditation for therapeutic purposes. But in fact yoga is a holistic way of life leading to a state of complete physical, social, mental, and spiritual well-being [47]. It is not merely doing one asana for a short period of time. There is a need for larger, long term well designed randomized clinical trials for assessing the effects of lowering BP in patients with prehypertension and stage 1 hypertension considering yoga as a way of life and not a short term therapeutic intervention.
Lifestyle therapy for Mild HTN: How long?: In a recent analysis, subjects (n=1114, mean age: 33±9 years) with stage-1 HTN untreated for at least 3 months having follow-up data available for at-least 2 years were included. Ambulatory BP (ABP) was performed at baseline, 3 months and at the end of study. Mean follow-up was for 11±6 (range: 2-20) years. Strong predictors of future normotension were a normal ABP at baseline and at 3 months and office BP decline of over 10 mmHg after a year [48]. Thus in young individuals with mild HTN (stage 1) long period of observation should be allowed before taking decision on drug therapy. At least duration of 3-12 months should be allowed before starting drug treatment with close follow-up of ABP, home BP or office BP.
Pharmacological treatment
In young patients, diastolic BP (≥ 90 mmHg) may have stronger relationship with total and CV mortality and up to 20% mortality could be explained by elevated DBP. ISH may occur with normal central aortic BP. Such individuals need close follow-up and lifestyle therapy is recommended [5]. Structural changes in large arteries of hypertensive patient evolve over time and may manifest after substantial time duration as ischemic heart disease, stroke or renal disease. Thus it may be prudent to arrest these structural changes early in the course of HTN [49]. A limited data exists on this hypothesis. Treating with valsartan to BP <140/90 was shown to slow and/or reverse early CV disease in asymptomatic high-risk patients with HTN [50]. With generous follow-up on lifestyle advice, BP tends to decline. If BP remains above the expected goal even after persistent lifestyle changes, antihypertensive therapy can be started.
Choosing a drug is important in a young individual. Most guidelines for HTN recommend use of all major classes of drugs for treating young hypertensives [5,14–17]. Among these, Angiotensin Receptor Blockers (ARBs), Angiotensin Converting Enzyme Inhibitors (ACEIs) are preferred as initial choice of agents although thiazide diuretics, Calcium Channel Blockers (CCBs), Beta Blockers (BBs) can be used alternatively for initiation and maintenance of treatment [5,16,17]. Two antihypertensive drugs either as singly or as combination therapy (from any class of drugs mentioned above) should be used when systolic BP is 20 mmHg or higher and/or diastolic BP is 10 mmHg or higher from the desired goal [17]. Strong evidence from randomized controlled trials on CV outcomes with antihypertensive therapy in young individuals is lacking. However, a meta-analysis involving 1,90,606 participants from 31 trials compared total major CVEs after antihypertensive treatment for young (<65 years) and old (≥65 years) observed no difference between age groups or differences in drug classes on major CV events. Also, no significant interaction was seen between age and treatment [51].
Role of beta-blockers (BB)
It is long believed that BBs should be preferred as first choice in young population. But this has been debated. In older (≥ 60 years) patients, significantly higher risk of stroke was observed with atenolol (RR: 1.17, 95% CI: 1.05-1.30) but not with other antihypertensives. With non-atenolol BB, RR was 1.22 (95% CI, 0.99-1.50) but did not reach statistical significance. Contrast to this, atenolol was associated with reduced risk (RR: 0.78, 95% CI: 0.64-0.95) of stroke in young adults (<60 years) and non-atenolol BBs were associated with lower risk of composite cardiac endpoint (RR: 0.86, 95% CI: 0.75-0.99). This suggests differential effects of BBs by age with potential benefits in young than old [52]. Thus for BB, young age is more important factor than choice of specific BB. They can be preferred in young individuals especially those with increased sympathetic drive, along with other antihypertensive agents [5].
Erectile Dysfunction (ED) is feared with use of BB in young individuals. But evidence suggests not just BB, but other antihypertensives may also have association with ED. The apparent ED in an individual is more likely because of underlying disease or to the anxiety related to side-effects of drugs [53]. Fear of ED might be the reason for nonprescription of BB and assurance may improve acceptance of BB in younger individuals.
Diuretics: Should they be used as sole agents for HTN?
Guidelines did not differ for four major classes of drugs as initial choice for young HTN. A very scant data exist for recommending diuretic as sole agents in initial management of HTN in young. In a small study (n=17) of young (18-35 years) pre-hypertensives, amiloride 10mg a day reduced systolic BP, diastolic BP, central systolic BP after 4 weeks. Thus diuretic treatment with amiloride can help prevent progression to HTN and thereby CV disease [54].
Assuring compliance
In CV disease, under utilization of preventive medications is high among younger age groups. Mehta et al., observed that young individuals (35-44 years) were 30-40% less likely being prescribed with BP lowering medication compared to older (65-75 years) adults [55]. Compliance to the prescribed therapeutic regime is an unsolved issue in patients with HTN. Hashmi et al., identified factors like younger age, poor awareness, and symptomatic treatment to be associated with poor adherence to antihypertensive therapy [56]. Every effort on part of treating physicians and young hypertensive is needed to ensure effective compliance to prescribed therapy. Drug combination with long acting medications will help improve compliance.
Treatment of Hypertension with Co-morbidities
There is very little data about the most effective treatment strategies for younger patients with high blood pressure [57]. Further association of HTN with co-morbidities makes it more difficult to advise best therapeutic strategy. In absence of clear evidence, we feel co-morbidities should be managed in line with their management in older adults. Choices of therapy in specific co-morbid conditions are tabulated in [Table/Fig-2].
Choice of therapy in HTN with co-morbidity {ASH-ISH/ACC AHA CAD/ADA}.
| Comorbidity | Initial choice | Second Preference | Third preference |
|---|
| Diabetes | ARB/ACEI | CCB | Thiazide diuretic |
| Chronic kidney disease | ARB/ACEI | CCB/Thiazide diuretic | Alternate drug for second preference |
| Coronary artery disease | BB + ARB/ACEI | CCB/Thiazide diuretic | Alternate drug for second preference |
| Stroke | ACEI/ARB | CCB/Thiazide diuretic | Alternate drug for second preference |
| Heart Failure | BB + ACEI/ARB + Diuretic + K sparing diuretic | Dihydropyridine CCB | |
Other co-morbidities like obesity, Obstructive Sleep Apnea (OSA), chronic obstructive pulmonary disease, and chronic infections need special attention. There is knowledge gap in understanding these conditions in young HTN. A study in college students (mean age 20 years) by Pensukasan et al., found 6.3% students at high risk for OSA and 4.5% had HTN. High risk of OSA was associated with HTN independent of demographic and lifestyle factors. Thus treating OSA is important modalities to prevent HTN in healthy young individuals [58].
BP Goal in HTN associated with Co-morbidities
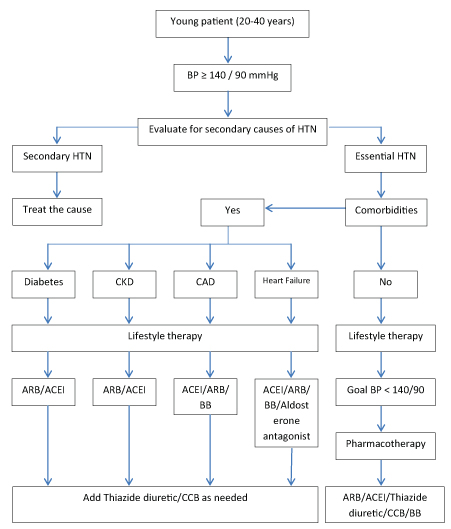
A BP goal of <140/90 mmHg is recommended in patients with diabetes, coronary artery disease and chronic kidney disease (CKD) without proteinuria [5,15,59]. In patients of CKD with proteinuria, a lower goal of <130/80 may preferable [14]. Further, American Diabetes Association (ADA) recommends lower target (<130/80) for young (age not specified) patients with HTN and diabetes [59]. An approach to the treatment of young HTN patient is detailed in [Table/Fig-3].
Approach to treatment of young HTN patient
Summary of expert opinion
Hypertension in the young is increasing in prevalence. Current prevalence average around 12%.
Essential HTN is the primary cause of HTN even in this young population.
Evaluate secondary causes of HTN in each young individual. A thorough history and clinical examination is vital to get clues for secondary HTN. Assessment of renal parenchymal and vascular disease by renal ultrasonography or angiography should be individualized.
Management of HTN in pregnancy is a specialized group. Careful follow-up is needed post-partum in view of future risk of CV morbidity.
Lifestyle therapy remains cornerstone in management of HTN in the young. Strict adherence to lifestyle management should be ensured.
Lifestyle therapy should be followed up for adequate time in young individuals before starting medications.
In lack of evidence on CV outcomes with antihypertensive therapy in young individuals, our management strategies are based on recommendations for older adults.
A goal of <140/90 mmHg is recommended for HTN without co-morbidities. A lower goal may be targeted in these patients but evidence on benefit in terms of CV outcomes is lacking.
Lower goal <130/80 may be useful in HTN associated with co-morbidities. Again evidence on CV outcome benefit is unclear.
ACEIs/ARBs should always be preferred as first line agents in patients not responding to lifestyle therapy.
CCBs/thiazide diuretic/beta blockers can be added or used as initial choice in patients with co-morbidities.
Use of fixed dose combinations preferably of drugs with once daily dosing is favoured to ensure adherence to therapy.
Conclusion
Management of HTN in young is essential to reduce long-term morbidity and mortality. The benefit of treating HTN in young is not only limited to reduction in BP but extends to prevention of structural and functional cardiovascular damage. Lifestyle therapy should be aggressively followed over a considerable period of time. Adherence to the therapeutic regime should be assured for higher benefits from BP reduction. In absence of clear evidence on young population on benefits of therapy, we identify a great need of prospective, randomized studies over a long duration of time in the young individuals with HTN.
[1]. Achala R, Kannuri NK, Pant H, Khan H, Franco OH, Di Angelantanio E, Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertensionJournal of Hypertension 2014 32:1170-77. [Google Scholar]
[2]. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Prospective studies collaboration. Age specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studiesLancet 2002 360(9349):190313 [Google Scholar]
[3]. Anderson GH, Effect of age on hypertension: analysis of over 4,800 referred hypertensive patientsSaudi J Kidney Dis Transpl 1999 10(3):286-97. [Google Scholar]
[4]. Johnson HM, Thorpe CT, Bartels CM, Schumacher JR, Palta M, Pandhi N, Undiagnosed hypertension among young adults with regular primary care useJournal of Hypertension 2014 32:65-74. [Google Scholar]
[5]. Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, 2013 ESH/ESC Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC)J Hypertens 2013 31(7):1281-357. [Google Scholar]
[6]. Joshi SR, Saboo B, Vadivale M, Dani SI, Mithal A, Kaul U, Prevalence of Diagnosed and Undiagnosed Diabetes and Hypertension in India-Results from the Screening India’s Twin Epidemic (SITE) StudyDiabetes Technology & Therapeutics 2012 14(1):8-15. [Google Scholar]
[7]. Prasad M, Flowers E, Mathur A, Sridhar V, Molina C, Turakhia M, Effectiveness of a community screening program for metabolic syndrome and cardiovascular risk factor identification in young South Asians adultsDiabetes & Metabolic Syndrome: Clinical Research & Reviews 2015 9:38-41. [Google Scholar]
[8]. Rao CR, Kamath VG, Shetty A, Kamath A, High blood pressure prevalence and significant correlates: A Quantitative Analysis from Coastal Karnataka, IndiaISRN Preventive Medicine 2013 2013:574973 [Google Scholar]
[9]. Shukla AN, Madan T, Thakkar BM, Parmar MM, Shah KH, Prevalence and predictors of undiagnosed hypertension in an apparently healthy western indian populationAdvances in Epidemiology 2015 2015:649184 [Google Scholar]
[10]. Aggarwal A, Aggarwal S, Sarkar PG, Sharma V, Predisposing factors to premature coronary artery disease in young (age ≤ 45 years) smokers: a single center retrospective case control study from indiaJ Cardiovasc Thorac Res 2014 6(1):15-19. [Google Scholar]
[11]. Van Minh H, Byass P, Chuc NTK, Wall S, Gender differences in prevalence and socioeconomic determinants of hypertension: findings from the WHO STEPs survey in a rural community of VietnamJournal of Human Hypertension 2006 20:109-15. [Google Scholar]
[12]. Yano Y, Stamler J, Garside DB, Daviglus ML, Franklin SS, Carnethon MR, Isolated systolic hypertension in young and middle-aged adults and 31-year risk for cardiovascular mortality the chicago heart association detection project in industry studyJ Am Coll Cardiol 2015 65(4):327-35. [Google Scholar]
[13]. Everett B, Zajacova A, Gender differences in hypertension and hypertension awareness among young adultsBiodemography Soc Biol 2015 61(1):1-17. [Google Scholar]
[14]. James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the eighth joint national committee (jnc 8)JAMA 2014 311(5):507-20. [Google Scholar]
[15]. Weber MA, Schiffrin EL, White WB, Mann S, Lindholm LH, Kenerson JG, Clinical practice guidelines for the management of hypertension in the community: a statement by the american society of hypertension and the international society of hypertensionJ Clin Hypertens (Greenwich) 2014 16(1):14-26. [Google Scholar]
[16]. Association of Physicians of IndiaIndian guidelines on hypertension (I.G.H.) - III. 2013J Assoc Physicians India 2013 61:6-36. [Google Scholar]
[17]. Daskalopoulou SS, Rabi DM, Zarnke KB, Dasgupta K, Nerenberg K, Cloutier L, The 2015 Canadian Hypertension Education Program recommendations for blood pressure measurement, diagnosis, assessment of risk, prevention, and treatment of hypertensionCan J Cardiol 2015 31(5):549-68. [Google Scholar]
[18]. Miura K, Daviglus ML, Dyer AR, Liu K, Garside DB, Stamler J, Relantionship of blood pressure to 25-year mortality due to coronary heart disease, cardiovascular disease, and all causes in young adult menArch Intern Med 2001 161:1501-08. [Google Scholar]
[19]. National High Blood Pressure Education Program. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Bethesda (MD): National Heart, Lung, and Blood Institute (US); 2004 [Google Scholar]
[20]. Mancia G, Grassi G, Manual of Hypertension of the European Society of Hypertension 2008 Informa UK Ltd [Google Scholar]
[21]. Sundström J, Neovius M, Tynelius P, Rasmussen F, Association of blood pressure in late adolescence with subsequent mortality: cohort study of Swedish male conscriptsBMJ 2011 342:d643 [Google Scholar]
[22]. Panja M, Kumar S, Sarkar CN, Sinha DP, Ray S, Chatterjee A, Hypertension in the young in Estern IndiaIndian Heart Journal 1996 48(6):663-66. [Google Scholar]
[23]. Camelli S, Bobrie G, Postel-Vinay N, Azizi M, Plouin PF, Amar , LB01.11: Prevalence of secondary hypertension in young hypertensive adultsJ Hypertens 2015 33(Suppl 1):e47 [Google Scholar]
[24]. Viera AJ, Neutze DM, Diagnosis of secondary hypertension: an age-based approachAm Fam Physician 2010 82(12):1471-78. [Google Scholar]
[25]. Bhalla A, D’Cruz S, Lehl SS, Singh R, Renovascular hypertension – its evaluation and managementJournal, Indian Academy of Clinical Medicine 2003 4(2):139-46. [Google Scholar]
[26]. Kamath SA, Young hypertensive: how and how much to investigate?Medicine Update 2008 18:570-77. [Google Scholar]
[27]. Kallistratos MS, Giannakopoulos A, German V, Manolis AJ, Diagnostic modalities of the most common forms of secondary hypertensionHellenic J Cardiol 2010 51:518-29. [Google Scholar]
[28]. Matthews KA, Katholi CR, McCreath H, Whooley MA, Williams DR, Zhu S, Blood pressure reactivity to psychological stress predicts hypertension in the CARDIA studyCirculation 2004 110(1):74-78. [Google Scholar]
[29]. Babu GR, Mahapatra T, Detels R, Job stress and hypertension in younger software professionals in IndiaIndian J Occup Environ Med 2013 17(3):101-07. [Google Scholar]
[30]. Seely EW, Maxwell C, Chronic hypertension in pregnancyCirculation 2007 115:e188-90. [Google Scholar]
[31]. Bramham K, Nelson-Piercy C, Brown MJ, Chappel LC, Postpartum management of hypertensionBMJ 2013 346:f894 [Google Scholar]
[32]. James PR, Nelson-Piercy C, Management of hypertension before, during, and after pregnancyHeart 2004 90:1499-504. [Google Scholar]
[33]. Bili E, Tsolakidis D, Stangou S, Tarlatzis B, Pregnancy management and outcome in women with chronic kidney diseaseHippokratia 2013 17(2):163-68. [Google Scholar]
[34]. Jindal Sk, Aggarwal AN, Chaudhry K, Chhabra SK, D’Souza GA, Gupta D, Asthma Epidemiology Study Group. Tobacco Smoking in India: Prevalence, Quit-rates and Respiratory MorbidityIndian J Chest Dis Allied Sci 2006 48:37-42. [Google Scholar]
[35]. Chadda RK, Sengupta SN, Tobacco use by Indian adolescentsTobacco Induced Diseases 2002 1(2):111-19. [Google Scholar]
[36]. Radhika G, Sathya RM, Sudha V, Ganesan A, Mohan V, Dietary salt intake and hypertension in an urban south Indian population--[CURES - 53]J Assoc Physicians India 2007 55:405-11. [Google Scholar]
[37]. Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ, Effect of lower sodium intake on health: systematic review and meta-analysesBMJ 2013 346:f1326 [Google Scholar]
[38]. Dietary Guidelines for Indians – A Manual. Second Edition. National Institute of Nutrition, Indian Council of Medical Research, Hyderabad India [Google Scholar]
[39]. Brown R, Ogden J, Children’s eating attitudes and behaviour: a study of the modelling and control theories of parental influenceHealth Educ Res 2004 19(3):261-71. [Google Scholar]
[40]. Anjana RM, Pradeepa R, Das AK, Deepa M, Bhansali A, Joshi SR, ICMR– INDIAB Collaborative Study Group. Physical activity and inactivity patterns in India - results from the ICMR-INDIAB study (Phase-1) [ICMR-INDIAB-5]Int J Behav Nutr Phys Act 2014 11(1):26 [Google Scholar]
[41]. Ravikiran M, Bhansali A, Ravikumar P, Bhansali S, Dutta P, Thakur JS, Prevalence and risk factors of metabolic syndrome among Asian Indians: a community surveyDiabetes Res ClinPract 2010 89(2):181-88. [Google Scholar]
[42]. Johnson HM, Olson AG, LaMantia JN, Kind AJ, Pandhi N, Mendonça EA, Documented lifestyle education among young adults with incident hypertensionJ Gen Intern Med 2015 30(5):556-64. [Google Scholar]
[43]. Eckel RH, Jakicic JM, Ard JD, de Jesus JM, Houston Miller N, Hubbard VS, American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice GuidelinesJ Am CollCardiol 2014 63(25 Pt B):2960-84. [Google Scholar]
[44]. Dalle Grave R, Calugi S, Centis E, El Ghoch M, Marchesini G, Cognitive-behavioral strategies to increase the adherence to exercise in the management of obesityJ Obes 2011 2011:348293 [Google Scholar]
[45]. Fontil V, Gupta R, Bibbins-Domingo K, Missed opportunities: young adults with hypertension and lifestyle counseling in clinical practiceJ Gen Intern Med 2015 30(5):536-38. [Google Scholar]
[46]. Lin JS, O’Connor E, Evans CV, Senger CA, Rowland MG, Groom HC, Behavioral counseling to promote a healthy lifestyle in persons with cardiovascular risk factors: a systematic review for the U.S. Preventive Services Task ForceAnn Intern Med 2014 161(8):568-78. [Google Scholar]
[47]. Taneja DK, Yoga and healthIndian J Community Med 2014 39(2):68-72. [Google Scholar]
[48]. Palatini P, Benetti E, Fania C, Mos L, Mazzer A, Cozzio S, 6A.02: White-coat hypertension as predictor of long-term normotension in subjects screened for stage 1 hypertensionJ Hypertens 2015 33(Suppl 1):e73 [Google Scholar]
[49]. Williams B, Hypertension in the young: preventing the evolution of disease versus prevention of clinical eventsJ Am Coll Cardiol 2007 50(9):840-42. [Google Scholar]
[50]. Duprez DA, Florea ND, Jones K, Cohn JN, Beneficial effects of valsartan in asymptomatic individuals with vascular or cardiac abnormalities: the DETECTIV Pilot StudyJ Am Coll Cardiol 2007 50(9):835-39. [Google Scholar]
[51]. Turnbull F, Neal B, Ninomiya T, Algert C, Arima H, Barzi F, Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different regimens to lower blood pressure on major cardiovascular events in older and younger adults: meta-analysis of randomised trialsBMJ 2008 336(7653):1121-23. [Google Scholar]
[52]. Kuyper LM, Khan NA, Atenolol vs nonatenolol β-blockers for the treatment of hypertension: a meta-analysisCan J Cardiol 2014 30(5 Suppl):S47-53. [Google Scholar]
[53]. Erdmann E, Safety and tolerability of beta-blockers: prejudices & realityIndian Heart J 2010 62(2):132-35. [Google Scholar]
[54]. Bhagatwala J, Harris RA, Parikh SJ, Zhu H, Huang Y, Kotak I, Epithelial sodium channel inhibition by amiloride on blood pressure and cardiovascular disease risk in young prehypertensivesJ ClinHypertens (Greenwich) 2014 16(1):47-53. [Google Scholar]
[55]. Mehta S, Wells S, Riddell T, Kerr A, Pylypchuk R, Marshall R, Under-utilisation of preventive medication in patients with cardiovascular disease is greatest in younger age groups (PREDICT-CVD 15)J Prim Health Care 2011 3(2):93-101. [Google Scholar]
[56]. Hashmi SK, Afridi MB, Abbas K, Sajwani RA, Saleheen D, Frossard PM, Factors associated with adherence to anti-hypertensive treatment in PakistanPLoS One 2007 2(3):e280 [Google Scholar]
[57]. Williams B, Hypertension in the young: preventing the evolution of disease versus prevention of clinical eventsJ Am Coll Cardiol 2007 50(9):840-42. [Google Scholar]
[58]. Pensuksan WC, Chen X, Lohsoonthorn V, Lertmaharit S, Gelaye B, Williams MA, High risk for obstructive sleep apnea in relation to hypertension among South East Asian young adults: role of obesity as an effect modifierAm J Hypertens 2014 27(2):229-36. [Google Scholar]
[59]. American Diabetes Association Diabetes GuidelinesSection 8. Cardiovascular Disease and Risk ManagementDiabetes Care 2015 38(Suppl. 1):S49-S57. [Google Scholar]