KCOT Occurring in Bilateral Maxillary Sinus in Non-Syndromic Patient
Vilas Newaskar1, Manish Verma2, Sushmita Rajmohan3, Dolly Dashore4
1 Professor and Head, Department of Oral and Maxillofacial Surgery, Government College of Dentistry, Indore, Madhya Pradesh, India.
2 Lecturer, Department of Periodontics, Government College of Dentistry, Indore, Madhya Pradesh, India.
3 Professor, Department of Oral and Maxillofacial Surgery, Sri Aurobindo College of Dentistry, Indore, Madhya Pradesh, India.
4 Lecturer, Department of Oral and Maxillofacial Surgery, Sri Aurobindo College of Dentistry, Indore, Madhya Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Manish Verma, 210 Khajuri Bazaar, M G Road, Indore, Madhya Pradesh-452002, India.
E-mail: idamanish@yahoo.co.in
Odontogenic Keratocyst (OKC) also termed as Keratocystic Odontogenic Tumour (KCOT) (WHO 2005) is a pathology with unique behavior because of which it is under much scrutiny and continued study. The pathology usually presents itself commonly in mandible and less commonly in maxilla. The occurrence of KCOT in maxillary sinus is reported as rare and multiple occurrences are mostly associated along with the presence of Nevoid Basal Cell Carcinoma (NBCC) syndrome. Here, we present a rare case of bilateral Maxillary OKC involving maxillary sinuses, without the presence of NBCC syndrome.
An interesting feature of this case is the presence of left upper third molar in ectopic position in maxillary sinus and a vertically impacted right third molar suggesting an origin from the dental lamina.
Dental lamina, Nevoid basal cell carcinoma, Odontogenic keratocyst
Case Report
A 21-year-old male patient reported to our clinic with the history of pain and recurrent swelling in the upper left back tooth region since seven days. Pain was dull, continuous, non-radiating and was relieved on taking medication. Since four days the pain was accompanied with extra oral swelling on the left middle third region of the face. The patient noticed the swelling intra orally distal to the last tooth in the left upper back tooth region. The swelling was accompanied by pus discharge. The area was tender and patient had reduced mouth opening. On presentation to the clinic the swelling and other symptoms had subsided due to medication.
Extraoral examination showed no evident of facial asymmetry. On intraoral examination, a sinus was evident distal to the left maxillary second molar and the area was erythematous in appearance with no ulceration. All other teeth were present except maxillary third molars. On palpation the area was tender and pus discharge was present.
The patient was subjected to radiographic investigations where Intra-Oral Peri-Apical (IOPA) radiograph and Orthopantomograph (OPG) were taken. IOPA did not show any periapical pathology in relation to second molar. OPG revealed haziness in both the right and left maxillary sinus and impacted teeth 18.
On the basis of history, clinical examination and radiographic presentation, a provisional diagnosis of dentigerous cyst with respect to tooth 28 was made.
On further investigation, Cone Beam Computed Tomography (CBCT) [Table/Fig-1] revealed hyper dense area obliterating complete left maxillary sinus causing thinning and expansion of walls of maxillary sinus. Hyper dense area was oval in shape and corticated borders were observed. Extension of lesion was from roof of the maxillary sinus to floor of maxillary sinus and the alveolar bone. Medio-laterally it extended from medial wall of maxillary sinus and ethmoidal sinus to lateral wall of maxillary sinus. The lateral nasal wall at the level of the middle concha was destructed and showed displaced and impacted tooth 28.
CBCT of maxilla showing bilateral pathology.
Extension of lesion was from roof of maxillary sinus to floor of maxillary sinus and alveolar bone with displaced and impacted tooth 28.
Right maxillary sinus revealed dome shaped expanded hyper dense area causing expansion and thinning of lateral wall of maxillary sinus and impacted tooth 18.
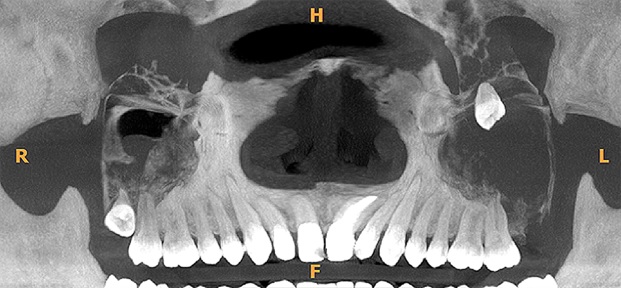
Right maxillary sinus revealed dome shaped expanded hyper dense area causing expansion and thinning of lateral wall of maxillary sinus. The cystic lesion showed complete destruction of the floor of maxillary sinus.
The radiographic diagnosis was dentigerous cyst in relation to tooth 28 involving left maxillary sinus and left nasal fossa and dentigerous cyst in relation to tooth 18 involving right maxillary sinus.
The presence of syndrome in this particular patient was ruled out after detailed clinical examination, blood investigations, chest and skull radiographs.
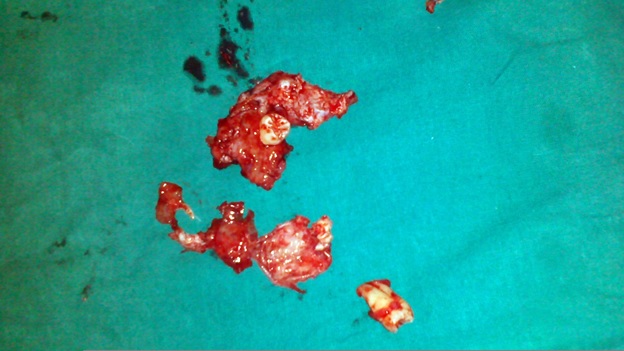
The surgery was planned for enucleation of the lesion with extensive curettage bilaterally through intraoral approach. Full thickness mucoperiosteal flaps were raised on either sides to expose the anterior wall of the maxilla bilaterally [Table/Fig-2,3]. Through Caldwell Luc approach the sinus was opened and the cystic lining was identified. Enucleation of the cystic lining was carried out extensively with the extraction of embedded teeth on either side [Table/Fig-4]. The lining texture was thick and adherent to the bony margins. Peripheral ostectomy was carried out wherever necessary and the lining was completely eliminated. Dressing was placed inside the sinus which was retrieved on the third post-operative day. Primary closure was done and post-operative healing was uneventful.
Intra-operative (Right side).

Intra-operative (Left side).

Excised lining with teeth.
All the excised cystic lining was subjected to histopathological examination. The report revealed that right sided section showed cyst wall lined by stratified squamous epithelium and content showed abundant keratin material and the left sided section also showed cyst with similar epithelium and keratin content thus confirming the diagnosis of odontogenic keratocyst involving bilateral maxilla.
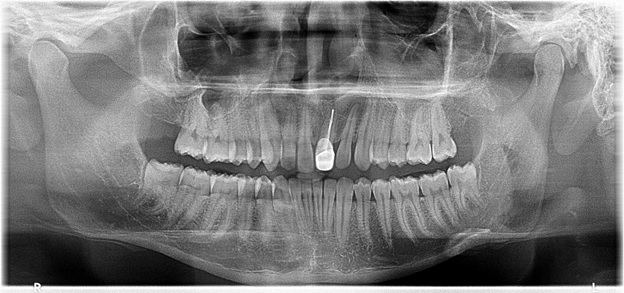
No recurrence has been determined after two year follow up [Table/Fig-5].
Follow-up OPG after 2 years.
Discussion
OKC was first reported by Phillipsen as a separate clinical entity in1956 [1]. OKC now also referred to as KCOT is a peculiar type of cyst which grows to a large size before it is evident clinically [2]. These cysts generally expand and grow within the medullary bone and therefore the pathology can be extremely large and still show no signs or symptoms [3]. In the case presented here, the patient reported due to an infection distal to the left second molar. Subsequent investigations during the treatment of same led to the discovery of multiple lesions in the maxillary sinus. Radiographically it presented as a unilocular or a multilocular radiolucency with scalloped and well defined margins and can be identical to a dentigerous cyst. Approximately 20%-40%of OKC’s are associated with unerupted tooth [4].
Occurrence of OKC in maxillary sinus is rare and the image can be misinterpreted due to normal radiopacity of the sinus. There was presence of unerupted teeth on both right and left sides giving the impression of huge dentigerous cysts. It is reported that KCOT are usually associated with crown of involved tooth and so should be distinguished from dentigerous cyst [5]. A definitive diagnosis is always made from histological examination of the biopsy specimen.
Histopathologically KCOT’s are always classified into parakeratotic and orthokeratotic subtypes [6]. This classification is based on the characteristics of the lining and type of keratin found. The parakeratotic type is reported to be more aggressive than orthokeratotic types [7].
Multiple OKC’s generally occur in NBCC syndrome, orofacial digital syndrome, Ehler Danlos syndrome, Noonan syndrome etc., [8,9]. Gorlin et al., in 1960 was the first to establish the association of multiple jaw cysts as a feature of Gorlin–Goltz syndrome. Shear and Soskolne (1967) showed in their studies [10], that patients with NBCC syndrome shows a predisposition to form OKC’s from dental lamina. Other manifestations of NBCC syndrome include palmar and plantar pits, bifid ribs, calcified falxcerebri and multiple basal cell carcinomas of skin. The chest radiographs and imaging of the skull did not reveal any features of NBCC syndrome in the present case. No dermatological signs were noticed which could have led to the diagnosis that the patient was syndromic.
The limitation of the present case is that the clinical sign, symptoms and radiographs were used as a reference to rule out the syndrome. No genetic studies were carried out to determine the absence of syndrome in this case.
Studies in literature have shown a higher male predilection in patients who were nonsyndromic [11]. A different study by Vedtofte 1979 showed equal gender distribution in patients with multiple OKC’s of whom half patients were syndromic (NBCCS) [10].
As suggested in literature the occurrence of KCOT is less than 1% in maxilla with sinus involvement [12,13]. According to University of Witwatersrand, Johannesburg, the study on age of occurrence confirmed a bimodal trend [10].
The first peak was around 15-45years and the second smaller peak at around 55-65 years. But in patients with syndrome there was found to be a single peak around 10-30 years. Rate of recurrence in this pathology varies between 0-62 percent, depending on the kind of treatment [14], but studies by Browns (1970) [10] showed no significant co-relation between the frequency of recurrence, age of the patient, location of cyst, method of treatment and nature of cyst lining. Recurrence principally occurs within five years of first surgery. The mitotic value of OKC lining is established at a value of 8.0 which is very high as compared to other cysts.
Treatment of OKC has been described by various authors and with different alternatives and adjunctive therapies. In this case we have done excision of the cystic lesion with the extraction of involved teeth and peripheral ostectomy was carried out where ever necessary.
Conclusion
To conclude it is noted that radiological appearance is not a definitive diagnosis of KCOT. Histopathological examination is necessary for a confirmatory diagnosis. Due to high recurrence of KCOT, care should be taken for complete excision and thorough enucleation. Recurrence of KCOT is even reported after 10 years of treatment. So regular post operative follow-up should be done at least for five years.
[1]. Chuong R, Donoff RB, Guralnick W, The odontogenic keratocystJ Oral Maxillofac 1982 40:797-802. [Google Scholar]
[2]. Philipsen HP, Keratocystic odontogenic tumour In: World Health Organization Classification of Tumours: Barnes L, Eveson JW, Reichart P, Sidransky D edsPathology and Genetics of Head and Neck Tumors 2005 LyonIARC Press:306-07. [Google Scholar]
[3]. Neville BW, Oral and Maxillofacial Pathology 2009 3rd edSt. Louis, MOElsevier/Saunders [Google Scholar]
[4]. Mendes RA, Carvalho JF, Vander Waal I, Characterization and management of the keratocysticod ontogenic tumor in relation to its histopathological and biological featuresOral Oncol 2010 46(4):219-25. [Google Scholar]
[5]. Gustafson G, Lindahl B, Dahl E, Svensson A, The nevoid basal cell carcinoma syndrome-Gorlin’s syndromeSwed Dent J 1989 13:131-39. [Google Scholar]
[6]. Haring JI, Van Dis ML, Odontogenic keratocyst: a clinical, radiographic, and histopathologic studyOral Surg Oral Med Oral Pathol 1988 66:145-53. [Google Scholar]
[7]. Verbin RS, Barnes L, Cysts and cyst like lesions of the oral cavity, jaws and neck. In: Barnes L edSurgical Pathology of the Head and Neck 1985 Vol.2New YorkMarcel Dekker:1257-63. [Google Scholar]
[8]. Blanchard SB, Odontogenic keratocysts: review of literature and report of a caseJ Periodontal 1997 68:306-11. [Google Scholar]
[9]. Yucetas S, Centiner S, Oygur T, Suspected familial odontogenic keratocysts related to Gorlin- Goltz syndromeSaudi Med J 2006 27:250-53. [Google Scholar]
[10]. Mervyn Shear and Paul Speight – Cysts of the Oral and Maxillofacial Regions. Fourth edition, Blackwell Munksgaard, 2007 [Google Scholar]
[11]. Chirapathomsakul D, Sastravaha P, Jansisyanont P, A review of odontogenic keratocyst and the behavior of recurrencesOral Surg Oral Med Oral Pathol Oral Radiol Endod 2006 101(1):5-9. [Google Scholar]
[12]. Brannon RB, The odontogenic keratocyst. A clinicopathologic study of 312 cases. Part I. clinical featuresOral Surg Oral Med Oral Pathol 1976 42:54-72. [Google Scholar]
[13]. Voorsmit RA, Stoelinga PJ, Van Haelst UJ, The management of keratocystsJ Maxillofac Surg 1981 9:228-36. [Google Scholar]
[14]. Brannon RB, Odontogenickeratocyst clinical pathologic study of 312 cases part II. Histologic featuresOral Surg Oral Med Oral Pathol 1977 43:233-55. [Google Scholar]