Accelerated orthodontic treatment is the need of the hour in current scenario as the conventional orthodontics is time taking. Corticotomy assisted orthodontics have been used for years to reduce the treatment duration by reducing the resistance provided by alveolar bone housing.
This case report describes the orthodontic treatment combined with the modification in conventional wilkodontic technique in a patient to accelerate tooth movement and shorten the treatment time with an anterior open bite and flared and spaced upper and lower incisors. Firstly plaque control was achieved with supra and subgingival scaling. A modified approach using periodontal access flap followed by vertical bone cuts in the cortical bone from the crest of the alveolar bone margin to 2mm-3mm below the apices of all the anterior teeth extending from upper left canine to upper right canine were performed. These vertical cuts were joined by horizontal cuts apically and flap repositioned. An MBT 0.018 inch appliance was bonded. Orthodontic therapy proceeded with frequent activation of the appliances to retract the incisors every two weeks. The total treatment time was four and half months with active period of two months and no adverse effects were observed at the end of active treatment. The modified decortication technique reduced the treatment time to a considerable extent. The interdental spacing closed and optimum overjet and overbite was achieved.
Case Report
A 24-year-old male patient reported to the dental clinic with the chief complaint of spacing between teeth in upper front region of jaw [Table/Fig-1]. The patient was systemically healthy with no deleterious habits found. Periodontal examination revealed adequate zone (>3mm) of attached gingiva, having no gingival recession, no signs of acute infection and periapical pathology, root fracture or severe root irregularities and a healthy Cementoenamel Junction (CEJ).
Pre treatment clinical view.

Prior to initiating the case, the purpose was explained to the patient and informed consent was signed by the patient. After proper examination and diagnosis, initial periodontal therapy comprising of supra and subgingival scaling was performed. Plaque control was monitored till a plaque score of ≤1 was achieved. The periodontal status was revaluated after six weeks to check for patient’s response to the therapy. In addition, blood investigations including Complete Blood Count (CBC), Haemoglobin (Hb%), Bleeding Time (BT), Clotting Time (CT) and Prothrombin Time (PT) were carried out in laboratory.
After the clinical examination it was found that patient was also having altered passive eruption Type I A along with chronic generalized periodontitis (horizontal bone loss with upper and lower anteriors along with periodontal pocket depth in relation to upper and lower anteriors was found to be increased) [Table/Fig-1,2].
Internal bevel incision given.

Surgical Procedure: Before the surgery, the patient was asked to rinse his mouth with 0.2% chlorhexidine gluconate solution for one minute. Asepsis was maintained throughout the procedure. The maxillary anterior area subjected for surgery was anaesthetized by nerve block and infiltration anaesthesia using local anaesthetic solution of 2% xylocaine containing 1:80,000 concentration of epinephrine (Ligno-Ad Local Anaesthetic, Proxim Remedies, India). Modified approach consisting of a periodontal access flap was initiated by internal bevel i.e., 2 mm apical to the crest of the margin along with intracrevicular (sulcular) incisions using Bard-Parker surgical blade #15 and #12 on the buccal and palatal aspects respectively, and then 2mm of gingival margin was discarded [Table/Fig-2]. The purpose of using a modified Widmann flap approach was to remove the excess gingiva to correct altered passive eruption
A mucoperiosteal flap excluding the gingival margin was elevated well beyond the apices of the anterior teeth both buccally and palatally [Table/Fig-3]. After the flap reflection based on the OPG, greatest mesiodistal width of the incisors guided the vertical bone cuts in the cortical bone from the crest of the alveolar bone margin to 2-3 mm below the apices of all the anterior teeth [Table/Fig-4,5]. The mesio-distal width of the tooth was the guide for the inter-incisal distance so that the cuts were placed in the inter-dental area. The vertical cuts were performed from the distal of the right upper canine to the distal of left canine with a 0.5mm thickness and 5mm wide carborundum disk bur. The depth of the cuts was 1.5mm-2mm (the thickness of cortical bone). The vertical cuts were joined using the horizontal cuts 2mm-3mm apical to the root apex. After the bleeding was controlled, the flap was repositioned, closed with interrupted sutures and periodontal pack was placed [Table/Fig-6,7].
After reflection of full thickness flap labially.

After corticotomy cuts given 2 mm apical to the root apex.

Modified crestal corticotomy cuts.

Simple interrupted sutures were placed.

Periodontal dressing given after the surgery.

Post-Operative Care: After surgery, a non-steroidal anti-inflammatory drug, consisting of combination of Ibuprofen 325 mg and Paracetamol 400 mg, three times a day for five days along with antibiotic consisting of Amoxicillin 500 mg three times a day was prescribed for five days post surgical period. Patient was instructed not to brush the teeth in the treated area and only to rinse with 0.2 % chlorhexidine gluconate twice daily, for 4-6 weeks and was instructed not to disturb the periodontal pack. As additional crestal incisions were given there was an additional bone cut so in order to reduce any chance of post operative swelling cold fomentation was advised along with an analgesic in combination with seratiopeptidase if at all swelling started to develop.
One week post surgery, sutures were removed, polishing of the teeth was done and patient was instructed to clean the treated area with chlorhexidine gluconate 0.2% using cotton pellet followed by soft tooth brush. Follow-up was done after 3, 6 and 12 weeks and clinical measurements i.e., width of keratinized gingiva and periodontal pocket depth were recorded post operatively.
Orthodontic Procedure: After the surgical procedure was performed, a 15 days of healing period was observed and then MBT 0.018” prescription was selected so as to reach the working wire 0.016” X 0.022” stainless steel wire within two months. After initial leveling and alignment, the space closure was started with conventional “e” chains and 15days activation was followed as per the conventional protocol after corticotomy so as to utilize the maximum of regional acceleratory phenomena [Table/Fig-8]. The 6mm of spacing was closed in a span of two months and the total treatment time for the patient was four and a half months [Table/Fig-9]. Post debonding a permanent lingual retainer was given for retention.
Orthodontic mechanotherapy.

Post treatment clinical view after four and a half months.

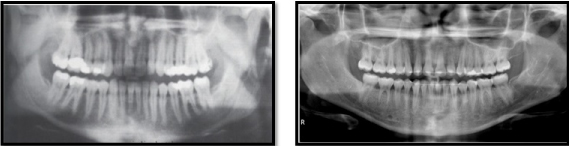
In this case report, patient with Class I malocclusion, maxillary anterior spacing was treated by modified alveolar corticotomy and facilitated orthodontic treatment. Ideal aesthetic and functional results were achieved in four and half months (active treatment period-2months) or one-third the average treatment time without detrimental periodontal effects such as gingival recession and periodontal pockets. Radiographic examination at three months post-surgery showed no significant reduction in the crest bone height, no marked apical root resorption and no post operative complications like mobility and devitalization of teeth [Table/Fig-10].
Pre and post treatment OPG.
Discussion
In this present world, where every individual wants to make a strong impact on the society, esthetics plays a vital role in connecting with the people around them. Thus recently, many adult patients who once ignored the esthetics at an early age are now starting to take interest in their cosmetic well being and for that, these patients are now seeking orthodontic treatment as well. However, adult orthodontic treatment gets difficult because dento-alveolar complex gets less plastic and more calcified. Due to this the average orthodontic treatment time in adults is more than in adolescent patients [1–3]. It is more likely for adult patients to experience root resorption, gingival recession because of an aplastic marrow, and less vascular periodontal membrane, as well as denser, avascular, and aplastic bone [4].
The corticotomy procedures have been employed for more than 100 years. The major historical events for corticotomy procedure are enlisted in [Table/Fig-11].
Historical events of corticotomy procedure.
| 1 | Kole H (1959) [5] | First successful clinical trial to check rapid tooth movement followed corticotomy. |
| 2. | Duker J (1975) [6] | Used Kole’s basic technique on beagle dogs to investigate how rapid tooth movement with corticotomy affects the vitality of the teeth and the marginal periodontium. |
| 3. | Frost HM (1983) [7] | Coined the term “Regional Acceleratory Phenomenon (RAP)”. |
| 4. | Wilko WM (2001) [4] | Coined the term “Accelerated Osteogenic Orthodontics (AOO)”. |
| 5. | Murphy and Wilko (2009) [8] | Coined the term “ Periodontically Accelerated Osteogenic Orthodontics”. |
The current corticotomy procedures are based on Kole’s combination of radicular corticotomy/supra-apical osteotomy technique comprising of buccal and lingual interproximal subcrestal vertical corticotomy cuts extending only up to cortical layers connected by horizontal osteotomy cuts approximately 1mm beyond the apices of the roots [9,10]. He suggested that the resistance of tooth movement could be overcome by creating what he called as “blocks of bone” in which the two blocks were connected to each other by just medullary bone only and that these “blocks of bone” could be orthodontically moved rapidly, taking anchorage from the crowns of the teeth [11].
In our modification, we have given crestal incisions over the bone around each tooth and creating complete blocks of bone i.e., “a true alveolar housing” and evaluated the effectiveness of the additional incisions on orthodontic movement of the specific teeth, these incisions were given as the crestal bone remains intact and it offers maximum resistance for tooth movement.
The rate of orthodontic tooth movement is related to bone mineral density [11]. Tooth movement in young patients is faster than in adults [11].
Hajji stated that the total treatment duration was only one-third to one-fourth to that of routine orthodontic therapies [11]. The basis of corticotomy as introduced by Kole (1959) relied on reducing the resistance provided by bone blocks [12,13]. The same concept was followed by many researchers who reported corticotomy-facilitated orthodontic treatment in many patients [14]. However conventional orthodontic forces were advocated by Wilcko et al., who explained the rapidity of tooth movement due to regional acceleratory phenomenon [4]. Initially, the term “Accelerated Osteogenic Orthodontics” was used to describe the combined corticotomy-facilitated orthodontics and periodontal alveolar augmentation [4]. Later, Wilcko et al., changed it to “Periodontally Accelerated Osteogenic Orthodontics” (PAOO) technique. Conventional corticotomy-facilitated orthodontic treatment involved buccal and lingual osteotomy cuts and the use of alveolar augmentation by bone graft to cover any fenestrations and dehiscences [4]. The use of autogenous bone graft taken from mandibular ramus was reported by Nowzari et al., and bone structure remained same a year after the completion of treatment [15].
In the current case, no gingival recession and root resorption were seen after the orthodontic treatment.
The modified technique employed for tooth movement during corticotomy induced regional acceleratory phenomenon using conventional orthodontic force. Therefore, two months of active orthodontic treatment time period in the present case could be considered adequate with this modified corticotomy approach.
The advantage of using this technique over conventional PAOO is that a “true alveolar housing” is created. In this technique crestal incisions were given over the bone around each tooth. The purpose of giving these additional incisions on the crestal bone was to create complete blocks of bone (islands of bone) so that there is minimum resistance offered by the crestal bone. In conventional PAOO the incisions extend just below crestal bone leaving the cortical bone intact which gives maximum resistance to orthodontic tooth movement whereas in our technique the incisions were given involving crestal bone so the resistance offered as compared to PAOO technique is less thereby expecting a faster tooth movement.
The disadvantage and the contraindication of this technique is that in cases where the teeth are crowded and root approximation is more, it is not possible to give crestal incision and also in crowding cases thinning of cortical plate takes place making it insignificant to give an additional crestal incision. The pre treatment OPG revealed mild amount of bone loss in relation to anterior teeth but even then the treatment was accomplished successfully with no complications seen. This adds to the evidence that the corticotomy assisted orthodontics can be carried out in patients with compromised periodontal health.
The indications for this technique are teeth with spacing between them, in cases requiring extraction, at the extraction site, bimaxillary protrusion with spacing or well aligned arches. The contraindications for this technique are crowding cases, class II division 2 malocclusion, buccally or palatally placed canines where thinning of cortical plate normally exists.
Conclusion
From the analysis of the results, and within the limitations of the present case it can be concluded that modified corticotomy- facilitated orthodontic treatment is an effective treatment approach in adults to decrease treatment time and reduce the risk of root resorption. The corticotomy cuts only on buccal and labial aspects, produced the Regional Acceleratory Phenomenon (RAP) which is needed to significantly reduce treatment time. However, the results obtained are limited and hence more clinical studies should be performed with additional patients and long-term follow-up.
[1]. Kole H, Surgical operations of the alveolar ridge to correct occlusal abnormalitiesOral Surg Oral Med Oral Pathol 1989 12:515-29. [Google Scholar]
[2]. Gantes B, Rathbun E, Anholm M, Effects on the periodontium following corticotomy-facilitated orthodontics. Case reportsJ Periodontol 1990 61:234-38. [Google Scholar]
[3]. Suya H, Corticotomy in orthodontics. In; Hosl E, Baldauf A, edsMechanical and Biological Basis in Orthodontics therapy 1991 Heidelberg, GermanyHutlig Buch:107-226. [Google Scholar]
[4]. Wilcko WM, Wilcko MT, Bouquot JE, Rapid orthodontics with alveolar reshaping: two case reports of decrowdingInt J Perio Restor Dent 2001 21:9-19. [Google Scholar]
[5]. Kole H, Surgical operations on the alveolar ridge to correct occlusal abnormalitiesOral Surg Oral Med Oral Pathol Oral Radiol Endod 1959 12:515-529. [Google Scholar]
[6]. Duker J, Experiment animal research into segmental alveolar movement after corticotomyJ Maxillofac Surg 1975 3:81-84. [Google Scholar]
[7]. Frost HM, The regional acceleratory phenomenon: a reviewHenry Ford Hosp Med J 1983 31(1):3-9. [Google Scholar]
[8]. Wilcko WM, Wilcko T, Bissada NF, An evidence-based analysis of periodontally accelerated orthodontic and osteogenic techniques: a synthesis of scientific perspectivesSemin Orthod 2008 14:305-16. [Google Scholar]
[9]. Murphy KG, Wilcko MT, Wilcko WM, Ferguson DJ, Periodontal accelerated osteogenic orthodontics: a description of the surgical techniqueJ Oral Maxillofac Surg 2009 67(10):2160-66. [Google Scholar]
[10]. Germeç D, Giray B, Kocadereli I, Enacar A, Lower incisor retraction with a modified corticotomyAngle Orthod 2006 76(5):882-90. [Google Scholar]
[11]. Hajji SS, The Influence of Accelerated Osteogenic Response on Mandibular Decrowding (master’s thesis) 2000 St. Louis, MoSt Louis University [Google Scholar]
[12]. Iino S, Sakoda S, Miyawaki S, An adult bimaxillary protrusion treated with corticotomy-facilitated orthodontics and titanium miniplatesAngle Orthod 2006 76(6):1074-82. [Google Scholar]
[13]. Suya H, Corticotomy in orthodontics. In: Hösl E, Baldauf A, edsMechanical and Biological Basics in Orthodontic Therapy 1991 Heidelberg, GermanyHütlig Buch:207-26. [Google Scholar]
[14]. Anholm M, Crites D, Hoff R, Rathbun E, Corticotomy facilitated orthodonticsCalif. Dent Assoc J 1986 7:8-11. [Google Scholar]
[15]. Nowzari H, Yorita FK, Chang HC, Periodontally accelerated osteogenic orthodontics combined with autogenous bone graftingCompend Contin Educ Dent 2008 29(4):200-06. [Google Scholar]