Case Report
A 22-year-old male patient with a history of slow growing non-tender hard swelling on left side of jaw since four months was referred to the outpatient clinic of Department of Oral and Maxillofacial Surgery. The patient didn’t have any complaint of pain, but there was a history of occasional salty discharge in the mouth. There were no other medical complaints or family history of similar swelling.
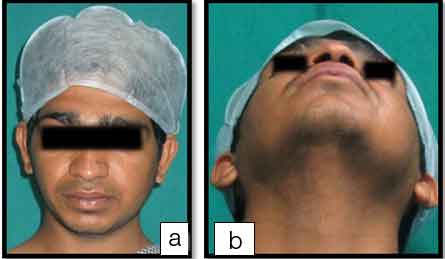
The patient was otherwise average built, with non-significant medical findings. Initial clinical examination revealed extra oral asymmetry due to oval-shaped swelling of size approximately 3cm X 2cm, on left side angle of mandible, with diffuse border. Antero-posteriorly swelling extends from left mandibular angle to left mandibular body region, super-inferiorly from the inferior border of the mandible to tragus [Table/Fig-1]. Overlying skin was normal and non-adherent to deeper structures. No draining sinus was seen extra orally. No neurologic changes were present. Intra-orally, on palpation bony hard non-tender swelling, was noted, in the third molar on lingual side and bony swelling with eggshell crackling on buccal aspect in the second molar region extending from the second molar to the retromolar region. Overlying mucosa was normal with a draining sinus in the region of the second molar. The second molar with slight mesial angulation and third molar with distal migration was noticed.
Preoperative photographs (a) Frontal view, (b) Worm’s view. Antero-posteriorly swelling extends from left mandibular angle to left mandibular body region, super-inferiorly from the inferior border of the mandible to tragus.
On aspiration, straw colored creamy fluid was obtained with traces of pus in it and was further sent for cytologic examination.
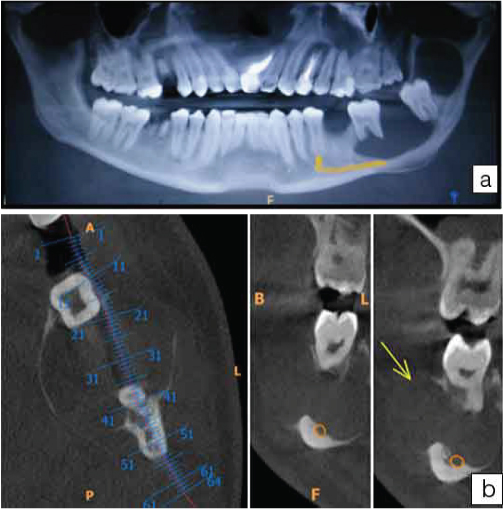
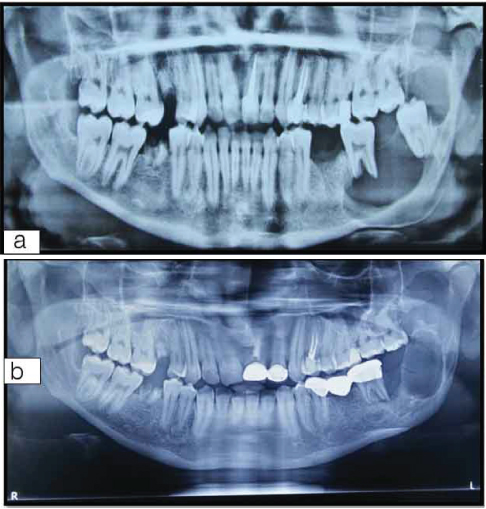
A panoramic image revealed the presence of round, well-defined cystic lesion extending from the root apex of the lower left second molar causing root resorption and extending up to third molar causing its distal migration. An additional radiolucent lesion which appeared to be an extension of the anterior lesion was separated by the third molar, extending into the ascending ramus up to the sigmoid notch. A Cone-Beam Computed Tomography (CBCT) suggested the presence of two separate lesions. The lesion anterior to the third molar showed thinning of buccal and lingual plates, an intact lower border of mandible and shifting of mandibular canal inferiorly. Another lesion distal to the third molar was seen extending into ascending ramus up to sigmoid notch with thinning of buccal and lingual cortices [Table/Fig-2a,b].
CBCT showing (a) two separate radiolucent lesions in panoramic view, one anterior to lower left third molar, another lesion distal to third molar. (b) Axial and sagittal section showing thinning of buccal and lingual cortical bone. Resorption of roots of the second molar was seen with the downward shifting of the inferior alveolar canal with intact inferior border.
On the basis of clinical presentation and aspiration of fluid from the anterior lesion (as both lesions considered as a single entity), provisional diagnosis of both the lesions was considered as OKC. The differential diagnosis was a dentigerous cyst, lateral periodontal cyst, ameloblastoma.
Treatment protocol for large and extensive OKC is advocated as follows:
Marsupialisation alone,
Marsupialization followed by enucleation/curettage, if necessary,
Excision of the lesion (resection) [1,2].
Considering the age of patient and extent of lesions, marsupialization followed by enucleation of cystic lining was planned, and if necessary along with enucleation (which may be done in secondary surgery if after one to one and half year sufficient bone formation has occurred at all the boundaries of the cystic lesion and if the cystic cavity is not fully obliterated) application of Carnoy’s solution as an adjuvant to reduce the chance of recurrences by eliminating residual pathology from peripheral bone like epithelial remnants or daughter cysts invaded into surrounding medullary cavity was planned to avoid extensive facial deformity at the younger age by advocating a more conservative method. The second molar involved in the lesion was decided to be retained as pulp vitality of the involved teeth was positive. In marsupialization, deeper parts of lining are not disturbed and closely adjacent important structures namely blood vessels to the apices of vital teeth and Inferior Alveolar Nerve (IAN) integrity remains intact as well as if OKC that interdigitates between and around the root surfaces of the teeth may be removed without a commitment to root canal therapy. Teeth that are curetted apically in this fashion become de-innervated, but not devitalized (a blood supply is maintained through pulpal connection through the periodontal ligament). Most will regain responsiveness to pulp testing in six months to one year [3,4]. Parents were informed about a need for regular follow-up and the second surgery of possible enucleation or jaw resection if required in due course of time.
Informed consent was obtained from the patient. The procedure was performed under general anesthesia with nasal intubation. An extended third molar incision was made and marsupialization was carried out for the lesion anterior to the second molar with the extraction of the third molar. After exposure of cystic lining, a window was created by excising lining, approximately 2cm in diameter and cystic cavity evacuated. The cavity was irrigated with normal saline and 5% povidine-iodine solution. The cystic lining was folded in cavity and edges were sutured with mucosal flap. 5% providine-iodine soaked gauze was packed in the cystic cavity [Table/Fig-3].
(a) Marsupialized cystic cavity; (b) Povidine-iodine soaked gauze pack kept in situ in marsupialized cavity; (c) Specimen from marsupialized cavity, (d) Enucleated cystic lining; (e) Acrylic denture plate gave for maintaining patency of cystic cavity.
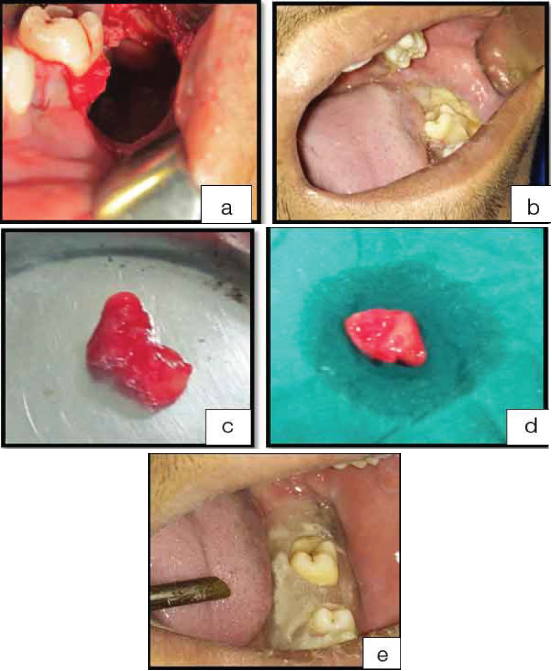
After extraction of the third molar, the thinned bone was removed exposing the cystic lining of the distal lesion which could be separated out from surrounding bone and completely enucleated, though enucleation of the lesion was not planned initially. The bony cavity was thoroughly irrigated and checked for any remnants. The distal flap was closed primarily with 3-0 VICRYL (Ethicon). Both specimens were labeled separately and sent for histopathological examination.
The patient was discharged after 48 hours. Oral antibiotics and anti-inflammatory were prescribed on discharge for one week. Two separate specimens were sent for histopathological examination, one from the marsupialized cystic lesion and another enucleated cystic lining distal do the third molar. Postoperatively uneventful healing observed. After 1-week gauze pack was changed. Acrylic denture plate was given to the patient to prevent food lodgment and maintaining the patency of cystic opening after two weeks [5].
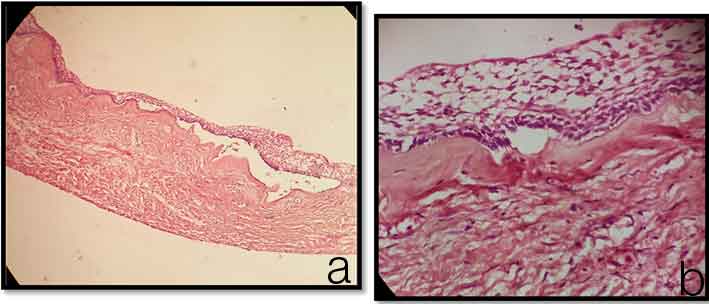
Histopathological examinations of anterior lesion specimen revealed a thin layer of parakeratinized stratified squamous epithelium (5-8 cell layers thick) and fibrous connective tissue. The distal specimen revealed an odontogenic epithelium, structured stellate reticulum, and peripheral palisading within a fibrous stroma [Table/Fig-4a,b]. These histopathological results indicated the diagnoses of OKC and cystic ameloblastoma, respectively. Both the lesions being highly recurrent, the patient is being followed up on a regular basis [Table/Fig-5a,b].
Histopathological analysis of the specimens obtained from the lesions following incisional biopsy; (a) Specimen from the lesion anterior to the third molar revealed a thin layer of regularly parakeratinized stratified squamous epithelium and fibrous connective tissue. The histopathological diagnosis was of the keratocystic odontogenic tumor; (b) Specimen from the lesion distal to the third molar revealed trabeculation of enamel organ-like tissue with proliferation of epithelium into stellate reticulum like cells. Histopathological analysis indicated ameloblastoma. Specimens were stained with hematoxylin-eosin and images were captured at anoriginal magnification of 10X.
Panoramic image (a) before treatment and (b) after 12months of marsupialization. Note significant bone formation around roots of lower left second molar with a reduction in the size of marsupialized lesion and also, a slight reduction in posterior enucleated lesion with mild thickening of the posterior border of irthe ramus. FPD has been given to the patient on the support of lower left second molar and premolar by some private dentist without consulting with the authors, although the bridge is stable and patient is comfortable, without any complaint in chewing.
Discussion
Cysts of the jaws are common and two important entities are the OKC and cystic ameloblastoma because of their propensity to recur. These two lesions, however, may present as ordinary cysts [6].
OKC has been reclassified as a benign neoplasm by WHO due to its aggressive nature and intrinsic growth potential but there is still a lot of controversy over it and on the use of new name keratocystic odontogenic tumor. There is as yet no international consensus among the clinicians, either on the question of the cyst’s neoplastic nature or on a name change. As the term ‘odontogenic keratocyst’, is so widely used by clinicians and pathologists, a good case can be made for retaining this term even if it is agreed that the cyst indeed has a neoplastic potential. Even if OKC is considered to be benign, locally invasive lesion with a high rate of recurrence; its treatment has remained to be controversial. There are still a number of articles proposing conservative management like marsupialization alone [2] and/or enucleation with use local adjunctives like cryotherapy, Carnoy’s solution or peripheral ostectomy. Resection is considered to be last option [1].
Ameloblastomas are slow growing benign odontogenic tumors that primarily occur in the molar region of the mandible. It is usually classified into solid or multicystic, unicystic and peripheral types. Unicystic Ameloblastoma though less aggressive than solid variant it still has a high rate of recurrence. Treatment cascade for it is described as small lesions can be treated with a radical surgical approach characterized by low morbidity (“box” resection). Large mandibular lesions without cortical perforation can be managed with conservative operations: enucleation followed by accurate curettage, including 0.5cm–1cm of surrounding clinically uninvolved bone [7]. When the cortex is perforated and soft tissue infiltrated marginal or segmental resection, including removal of overlying soft tissues, should be the treatment of choice [8].
Clinically and radiographically both ameloblastoma, especially the Unicystic ameloblastoma and OKC are indistinguishable due to the similar location of occurrence, the age of patients.
The synchronous occurrence of ameloblastoma and OKC as distinct lesions is very rarely documented in English language literature [9,10]. Combined occurrence of odontogenic tumors called as combined or hybrid lesions have also been reported in other situations [11], but the occurrence of two distinct and simultaneous odontogenic lesions in the same patient is extremely rare.
Ameloblastomas have been previously reported to co-occur with an ortho-keratinized odontogenic cyst and a glandular odontogenic cyst [12]. Fregnani et al., reported a case of synchronous ameloblastoma and ortho-keratinized odontogenic cyst located on bilateral posterior regions of the mandible [10]. In addition, Hisatomi et al., described a case of a glandular odontogenic cyst that was associated with an ameloblastoma [13]. Shimamoto et al., presented a case of ossifying fibroma and KCOT [14]. Case reports with simultaneous occurrence of odontogenic lesions have been tabulated in [Table/Fig-6].
Case reports of simultaneous odontogenic lesions of the jaw.
| Case [reference] Modality, Locality | Year | Age | Gender | Histopathological Diagnosis | Imaging |
|---|
| Hisatomi et al., [13] Mandible | 2000 | 45 | F | Glandular odontogenic cyst and ameloblastoma | IO, CT, MR |
| Fergnani et al., [10] Mandible | 2006 | 21 | M | Ameloblastoma & orthokeratinised | PI, CT |
| Shimamo et al., [14] Mandible | 2011 | 48 | F | OF and KCOT | PI, CT |
| Gamoh et al., [9] Mandible | 2015 | 45 | M | KCOT and ameloblastoma | PI, CT, SI |
| Present Case Mandible | 296 | 22 | M | OKC and Unicystic ameloblastoma | PI, CBCT |
M=male; F=female; OF=Ossifying Fibroma; KCOT=Keratocystic Odontogenic Tumor; OKC=Odontogenic Keratocyst; IO=Intaroral Image; PI=Panoramic Image; CT=Computed Tomography; SI=Soft X-Ray Image; CBCT=Cone Beam Computed Tomography
They may both present as ordinary cysts in the dentate area. They can be multilobular or multilocular and unilocular and both have a predilection for the angle of the mandible and ascending ramus [10,12].
The present case proved the possibility of the simultaneous occurrence of OKC and ameloblastoma in a jaw. This knowledge should be a valuable warning as both the lesions have high recurrence rate and require long-term follow-up.
Follow-up of patients with ameloblastoma or odontogenic keratocyst should be carried out regularly. As most recurrences present within the first five years, yearly follow-up during this period is advisable [6,15,16]. Thereafter, follow-up every two years seems appropriate but should extend for at least 25 years, as recurrences may appear after a long time [17].
Conclusion
The presence of ameloblastoma as one of the cystic lesions shows the importance of proper histopathological assessment after surgery for further management of the patient as there is a higher chance of recurrence and need of extensive surgery like resection in cases of ameloblastoma.
M=male; F=female; OF=Ossifying Fibroma; KCOT=Keratocystic Odontogenic Tumor; OKC=Odontogenic Keratocyst; IO=Intaroral Image; PI=Panoramic Image; CT=Computed Tomography; SI=Soft X-Ray Image; CBCT=Cone Beam Computed Tomography
[1]. Tolstunov L, Treasure T, Surgical treatment algorithm for odontogenic keratocyst: combined treatment of odontogenic keratocyst and mandibular defect with marsupialization, enucleation, iliac crest bone graft, and dental implantsJ Oral Maxillofac Surg 2008 66:1025-36. [Google Scholar]
[2]. Pogrel MA, Marsupialization as a definitive treatment for the odontogenic keratocystJ Oral Maxillofac Surg 2004 62:651-55. [Google Scholar]
[3]. Shear M, Speight P, Cysts of oral and maxillofacial region 2007 4th edVictoria AustraliaBlackwell Publishing Asia Pty Ltd:228-29. [Google Scholar]
[4]. Robert E. 2nd ed. Quintessence Publishing Co, Inc; 2002. Nov 1, Marx, Diane Stern Textbook of Oral and Maxillofacial Pathology: A Rationale For Diagnosis and Treatment. 2003; pp. 596-97 [Google Scholar]
[5]. Langdon J, Patel M, Ord R, Brennan P, Operative Oral And Maxillofacial Surgery 2011 2nd edLondon, UKHodder Arnold:76 [Google Scholar]
[6]. Chapelle KA, Stoelinga PJ, de Wilde PC, Brouns JJ, Voorsmit RA, Rational approach to diagnosis and treatment of ameloblastomas and odontogenic keratocystsBr J Oral Surg 2004 42:381 [Google Scholar]
[7]. Sammartino G, Zarrelli C, Urciuolo V, di Lauro AE, di Lauro F, Santarelli A, Effectiveness of a new decisional algorithm in managing mandibular ameloblastomas: a 10-years experienceBr J Oral Maxillofac Surg 2007 45:306-10. [Google Scholar]
[8]. Gardner DG, Some current concepts on the pathology of ameloblastomasOralSurg Oral Med Oral Pathol Oral Radiol Endod 1996 82(6):660-69. [Google Scholar]
[9]. Gamoh S, Akiyama H, Tominaga K, Nakajima M, Kakudo K, Tanaka A, Simultaneous occurrence of keratocystic odontogenic tumor and ameloblastoma in the mandible: A case reportOncology Letters 2015 10:785-89. [Google Scholar]
[10]. Fregnani ER, Cruz Perez DE, Soares FA, Alves FA, Synchronous ameloblastoma and orthokeratinized odontogenic cyst of the mandibleJ Oral Pathol Med 2006 35(9):573-75. [Google Scholar]
[11]. Siar CH, Ng KH, Combined epithelial odontogenic tumor in MalaysiansBr J Oral Maxillofac Surg 1991 29(106) [Google Scholar]
[12]. Som PM, Curtin HD, Tumors and Tumor-like ConditionsIn: Head and Neck Imaging 2003 vol14th ednSt. LouisMosby:347-352.:354-56.Som PM and Brandwein MS (eds) [Google Scholar]
[13]. Hisatomi M, Asaumi J, Konouchi H, Yanagi Y, Kishi K, A case of glandular odontogenic cyst associated with ameloblastoma: Correlation of diagnostic imaging with histopathological featuresDentomaxillo fac Radiol 2000 29(4):249-53. [Google Scholar]
[14]. Shimamoto H, Kishino M, Okura M, Chindasombatjaroen J, Kakimoto N, Murakami S, Radiographic features of a patient with both cemento ossifying fibroma and keratocystic odontogenic tumor in the mandible: A case report and review of literatureOral Surg Oral Med Oral Pathol Oral Radiol Endod 2011 112(6):798-802. [Google Scholar]
[15]. Stoelinga PJW, Long-term follow-up on keratocysts treated according to a defined protocolInt J Oral Maxillofac Surg 2001 30:14-25. [Google Scholar]
[16]. Reichart PA, Philipsen HP, Sonner S, Ameloblastoma: biological profile of 3677 casesEur J Cancer B Oral Oncol 1995 31B(2):86-99. [Google Scholar]
[17]. Bisinelli JC, Ioshii S, Retamoso LB, Tetü Moysés S, Moysés SJ, Tanaka OM, Conservative treatment of unicystic ameloblastomaAmerican Journal of Orthodontics and Dentofacial Orthopedics 2010 137(3):p297-442. [Google Scholar]