Introduction
Needlestick and sharps injuries (NSIs), are among the main job-related injuries that health care workers experience. In fact, contraction of hepatitis B or hepatitis C from work-related NSIs is one of the most common occupational hazards among health care workers.
Aim
The aim of this study was to determine the factors associated with NSIs in health care occupation.
Materials and Methods
In this study, a systematic and purposive review with emphasis on the research question was run to retrieve, evaluate and consolidate the required information. The following four key words were used to search for the relevant articles published from January 1998 to May 2015: NSI health care workers, risk factor and factors associated, in Science direct, EBSCO Host, PubMed, ProQuest, SID and Cochrane Library. Several steps of evaluation were taken to select and analyse the full texts of relevant articles. According to the inclusion criteria, we finally selected 11 articles from the 18642 retrieved articles.
Results
The data of the analysed articles indicated that the highest incidence of NSIs was seen in nurses and that the associated factors were age, level of education, number of shifts per month and history of related training. The highest rate of NSIs was related to instrument preparation followed by injection and recapping of used needles. Findings show that health care workers suffer a high rate of needlestick injuries.
Conclusion
It was seen that device, location, or action cannot be separately considered as responsible for all types of the NSIs. Rather, each of them has a contribution to the NSIs. Nevertheless, factors with higher frequency should be given a higher priority.
Introduction
Health Care Workers (HCWs) are at high risk for job-related infection due to biological factors because these workers are frequently exposed to human body fluids. Each year, hundreds of thousands of HCWs face the risk for blood-borne diseases which are acquired in job situations due to needlestick and sharps injuries (NSIs) [1].
NSIs, which can be prevented, are among the main job-related injuries that registered nurses experience in hospitals [2,3]. Among the main potential problems caused by NSIs, there are infectious diseases such as hepatitis B, hepatitis C and HIV. These diseases are transmitted by blood pathogens derived from contaminated needles or sharp device [4–7].
The number of percutaneous injuries per 100000 inpatient-days is estimated to be 2.43 in nurses, each year, approximately 10-fold higher than 0.23 which has been reported for medical doctors, and 0.20 for technologists. Furthermore, in Taiwan, hepatitis B and hepatitis C are endemic, with prevalence rates of 17.3% and 4.4% in the general population, respectively [8,9].
Due to their duties or some other reasons, HCWs are frequently at risk for exposure to NSIs [10]. These injuries constitute a major threat to HCWs’ psychophysical well-being [11]. The average risk of being infected with HIV from various types of job-related exposure is estimated to be low in comparison to the risk of being infected with hepatitis B virus (HBV) or hepatitis C virus (HCV) [10,12,13]. The reported risks of contracting infections after sustaining pathogen-positive NSIs were 0.3% for HIV, 6.0-30.0% for HBV, and 0%-10.0% for HCV [14]. Previous studies have shown that in the population of Taiwan, the seropositivity rate for HBsAg and HCV antibody is 15%-21% and 2.5%, respectively. In fact, contraction of HBV or HCV from work-related NSIs is one of the most common occupational hazards among HCWs in Taiwan [14].
In addition to causing potential threats due to infectious diseases, NSIs impose direct costs which are spent for laborotory tests such as tests for HIV antibodies, hepatitis B serology, and a baseline test for anti-hepatitis C, along with treatment costs spent for these conditions [6]. Other costs are related to post exposure prophylaxis for registered nurses as well as the economic loss imposed on hospitals because of absence from work [15]. The costs of the tests and treatments for NSIs are estimated to range from $6.1 million in France to $118–591 million in the USA per year [16]. At a tertiary care hospital in Mumbai, India, nearly Rs 9000/HCW/episode of needlestick injury are paid as short-term expenses [17]. A comprehensive review of relevant studies has demonstrated that the NSIs were associated with three major factors: engineering factors including the form of sharp devices and barrier devices, organizational factors including the existence of supplies and policies for reporting and behavioural factors like recapping and disposal-related issues [18]. Consistent with the cited review, The World Health Organization has reported the unavailability of engineering controls to make sure that safer needle devices are accessible, inadequacy of hospital staffing, and failure to replace needle caps after use to be some risk factors [19]. Based on the International Health Care Worker Safety Center, in the USA, injections accounted for 23.6% of NSIs and drawing venous blood accounted for 11.5% of NSIs. The review of the studies carried out in the USA, United Kingdom, Germany, France, Italy, and Spain shows that a significant proportion of NSIs are caused by injections, intravenous-related tasks, and use of safety engineered needle devices to do these tasks [20]. The aim of the present study was to assess the factors associated with NSIs in health care occupations.
Materials and Methods
Search Strategy and Inclusion Criteria
Investigation strategy: This systematic review has considered the incidence of NSIs and sought to determine the factors associated with such injuries within health care occupations. The major questions of the present study were: “What is the incidence rate of NSIs in HCWs in the previous studies?” And “what are the major findings of the studies reviewed regarding the factors associated with such injuries among health care occupations?” Data collection was performed by four inclusion criteria: 1) Published within the past 16 years (January 1998-May 2015); 2) Published in English and Persian languages; 3) Published in trustworthy peer-reviewed scientific journals; and 4) Occurrence of the keywords in titles or abstracts. The following words were used independently and then in combination to search for in databases and electronic journals: Occupational exposure; needlestick injuries; health care worker; risk factor; factors associated. The articles on the needlestick with accessible full text were searched for in Science Direct, EBSCO Host, PubMed, ProQuest, SID and Cochrane Library.
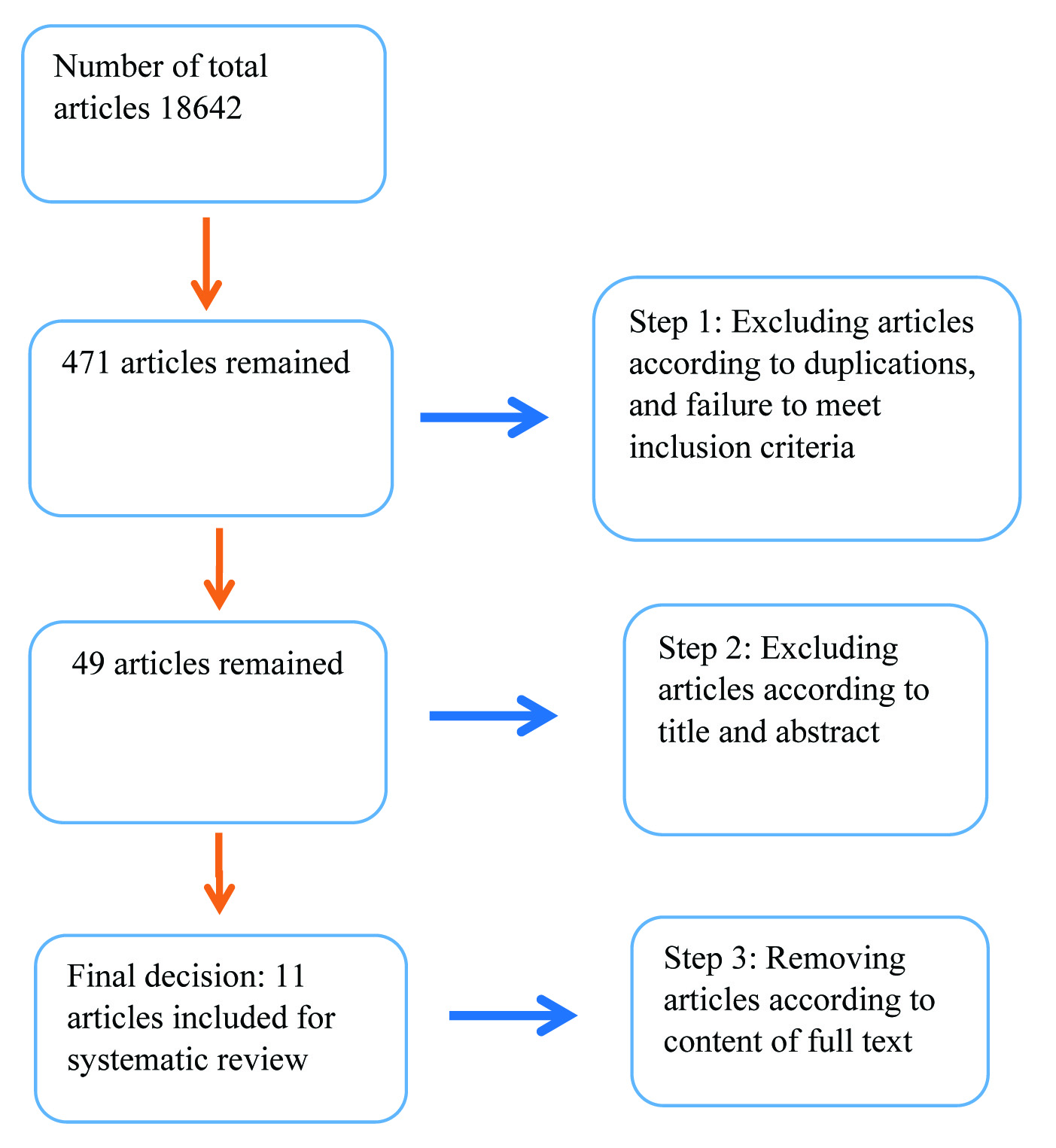
According to the inclusion criteria, 18642 articles were retrieved. Each step of this process was carried out by two researchers. First, the articles which did not comply with the inclusion criteria or were duplicated were ruled out (n=18171). Secondly, some articles were ruled out on the basis of title and abstract (n=422). In the third step, the full texts of the remaining 49 articles were read and 38 articles were ruled out based on the content of the articles. In the final step, eight articles in English and three articles in Persian language were picked out and their full texts were reviewed and analysed. The process of selecting articles was systematically performed in three steps [Table/Fig-1]. The data obtained from each article included the author(s), the time and location of the study, the method of sampling, the methodology, and the major findings [Table/Fig-2].
Process of selecting articles for review.
Methodological characteristics of the reviewed studies.
| No | Author | Methodology | Samples | Country | Results |
|---|
| 1 | Smith et al., [22] | Descriptive-exploratory | 509 nurses | China | Nurses who reported their departments were understaffed were more likely to suffer needlestick injuries than nurses who told their departments were sufficiently staffed. Nurses who worked mixed shifts were more likely to sustain NSIs than those who did not. |
| 2 | Nsubuga and Jaakkola [9] | Descriptive | 526 nurses and midwives | Africa | Lack of training was the most important risk factor for needlestick injuries; working for more than 40 h/week, replacing needle caps most of the time, and not wearing gloves when working with needles. |
| 3 | Lotfi and Gashtasbi [21] | Cross-sectional study | 90 health center personnel | Iran | Important risk factor for needlestick injuries was working night shifts; other important risk factors included lack of training on such injuries, number of patients attended daily or nightly and recapping needles. |
| 4 | Rampal et al., [25] | Cross-sectional study | 345 health care workers | Malaysia | Staff nurses suffered the highest prevalence. The causes of needlestick injuries were mainly replacing needle caps. Majority said that they dispose of needles or sharp devices instantly after use in sharp bins, most of them did not separate needles from syringes before throwing away and did not dissemble needles or sharps with hand and restore needle caps after use. |
| 5 | Bijani [26] | Cross-sectional study | 246 nurses | Iran | Independent risk factors for needlestick injuries were recapping used needles habitually and consecutive shift works. |
| 6 | Habib et al., [27] | Cross-sectional study | 216 nurses selected by convenience random sampling | Pakistan | Most injury causing instruments and needlestick injuries were reported at bedside and wards, the professionals did not participate in any educational sessions, seminars or workshops related to needlestick injuries during their job. |
| 7 | Martins et al., [28] | Cross-sectional study | 363 health care workers | North Portugal | The major risk factor was working in health services for more than 10 years. Another important associated factor was being over 39 years old. |
| 8 | Parsa-Pili et al., [33] | Cross-sectional study | 97 health care workers | Iran | A significant association was observed between the risk of needlestick injury and age, gender, work experience of less than two years and education. The majority of needlestick injuries happened at the ICU and CCU. |
| 9 | Afridi et al., [34] | Cross-sectional study | 497 health care workers | Pakistan | Factors which are found to be highly associated with needlestick injuries were experience of more than five years and working as nurse than doctor, working in surgical wards and being a female. Most repeatedly quoted cause of needlestick injuries was injecting medicine and drawing blood, followed by doing needle recapping by two hands. |
| 10 | Yenesew and Fekadu [24] | Cross-sectional study | 317 health care professionals | Northwest Ethiopia | The reasons for job-related exposure to blood and body fluids were: the sudden movement of a patient during blood sampling or the intramuscular or venous injection of drugs during childbirth; during the handling of specimens; during recapping of specimens; during handling and collection of waste; and due to lack of personal protective equipment. |
| 11 | Ashat et al., [23] | Descriptive | 107 health care workers | India | The major factor for the exposure was heavy patient load. Most injury instances happened during emergency care. The most conventional action after exposure was cleaning with spirit. |
Results
The data of the analysed articles indicated that the highest incidence of NSIs was seen in nurses [Table/Fig-2]. Various factors resulted in these injuries including overcrowding of hospital wards, failure to observe universal precautions, and patients’ fault [21,22]. The highest injury incidence happened during emergency care [23]. Injured sites included finger tips, hands, and face/eyes. The frequency of NSIs was compared based on different demographic variables [24].
The highest NSIs incidence was related to instrument preparation, followed by injection and recapping of used needles [24–26]. The incidence of NSIs has been reported to be associated with age, level of education, immunization status, number of shifts per month, and history of related training [27].
NSIs are more likely to happen in understaffed departments than adequately staffed departments, and to nurses who work mixed shifts than those who didn’t [22]. The results indicated an association between the NSIs and gender, so that the majority of NSIs happened to women [27]. The results demonstrated that the most significant risk factor for NSIs was closely associated with an increased odds ratio for sharps injuries, being senior or nursing officer, having work experience for less than 10 years, working long hours and not using gloves [9,24,28].
Discussion
This systematic review demonstrated the results of 11 articles which investigated the prevalence of NSIs and their association with risk factors among HCWs who cared for the patients in hospitals directly. A limitation of this systematic review is the potential bias due to the research strategy.
Various studies have indicated that there are wide variations in the prevalence of NSIs among HCWs [4,18,29,30]. The variations in the NSIs prevalence in different regions can be explained by different number of HCWs per hospital, various work cultures and environments, differences in availability of resources, measurement methods and research designs.
In this study, the majority of the exposed HCWs were nurses [22], which is similar to a study in Taiwan [12]. This can be explained by the fact that nurses perform the majority of the injections and intravenous fluid administration. Basically, nurses are the main health care professionals that deal with injections and sharp objects; moreover, the number of nurses is generally higher in comparison to other occupational groups in hospitals. It should not be forgotten that not having enough nurses in hospitals is also a problem per se.
The main reasons for occupational exposure to Blood and Body Fluids (BBFs) in this study were: a sudden movement of the patient during blood sampling or during the intramuscular or venous injection of drugs; during childbirth; during the handling of specimens; during the recapping of specimens; during the handling and collection of waste; or due to a lack of Personal Protective Equipment (PPE) [24], which is in agreement with Dessie study [31]. Most published works have recommended that training be given on wearing gloves in every procedure and other PPE whenever necessary to prevent occupational exposure to BBFs and NSIs [19,27,32]. In Yenesew and Fekadu study, 54% of the participants reported that they wore gloves during the last health care procedure [24], which is lower than Dessie study (85%) [31].
Previous studies have clearly confirmed the significance of engineered safety devices in decreasing NSIs [19,25,27]. Yenesew and Fekadu consider using safety devices as the best way to decrease NSIs and protect against the associated risks [24]. Previous studies have also demonstrated that interventions on safety devices use is more effective compared to educational workshops conventionally held for health care providers [23,32]. Notably, while education is an effective tool in reducing NSIs, it has been proved to be not as effective as safety devices.
In the present study, training was the most significant factor for the incidence of NSIs among the nurses [21,33]. The nurses who did not participate in any training sessions regarding prevention and dealing with NSIs in their workplace faced a significantly higher risk of suffering such injuries in comparison with those participating in some type of training [9]. This finding has great significance for planning for preventive measures in developing countries, where organizing appropriate training is a more practical goal than supplying expensive equipment.
The present study demonstrated that the risk for NSIs significantly increased among those who usually or always did needle recapping in comparison to those who did not [24,26,34]. This finding is compatible with other studies [29,30,35,36]. Using gloves during work with sharp devices is a suggested preventive measure suggested and observing this measure appears to be an indicator of risky behaviour [9,19]. HCWs that only sometimes or never wore gloves faced a significantly higher risk of suffering NSIs compared with those who wore them regularly. Some of the studies have associated use of gloves with observing precautions in general [6,27, 33]. Needle recapping, placing sharps containers and not wearing protective gloves are factors that can be improved through training, but unavailability of protective equipment and safe needles can regularly be observed in many developing countries and may somewhat explain risky behaviours among HCWs.
This systematic review has found no randomized control trials (RCTs) attempting to decrease NSIs. This means that the designs of the studies were either cross-sectional or retrospective. The rarity of RCT designs has led to the fact that reliable scientific evidence is unavailable based on the available studies. Therefore, more emphasis and investment need to be placed on randomized controlled trials.
In the present study, the high prevalence of NSIs was also because of other factors including heavy patient load [21]. Governmental hospitals are overloaded and because of the essence of urgency in certain wards like emergency, labour rooms’ HCWs are likely to neglect and not to observe universal preventive measures [2,27,34]. Other risk factors were long work hours and inadequate experience [37]. Future research should explore the type of training which is most effective. This emphasizes the importance of considering perceived benefits and threats while developing plans to decrease NSIs among HCWs. When the interns understood the threats of acquiring a disease and benefits of wearing gloves, they observed the standard precautions more than ever.
Limitation
This review article suffers from some limitations. It is a review of the previous studies that were conducted in different time periods. Therefore, the distribution may be incorrect, though the studies were screened using STROBE checklist for observational studies, conducted on the factors associated with NSIs in health care occupations. The personnel in these occupations are in direct contact with different patients everyday and consequently are exposed to higher risk. The questions that were formulated to extract information regarding NSIs from the study participants were diverse in different studies; therefore, it was difficult to compare the results of the selected studies and common findings were reported. Furthermore, attempts were made to include all the published literature on the risk factors and factors associated with NSIs in health care occupations, but it is likely that some important findings, especially conference proceedings and dissertations, have not been included mainly because of the type of the search strategy adopted in this review article.
Conclusion
The results demonstrated that device, location, or action cannot be separately considered as responsible for all types of NSIs, but each of them in turn can contribute to the injury. Safety devices must be used more frequently by HCWs, and educational programs with close monitoring for practices to reduce the NSIs must be developed and administered. Furthermore, attention should be paid to decreasing excessive workloads and to sufficient training for particular work duties among the HCWs. Hospitals can decrease NSIs by creating work environment that has adequate staff and resources. Minimizing emotional exhaustion at work as well as providing safety-engineered devices and equipment can be useful in this regard. Periodic training on appropriate and safe work procedures should be provided for HCWs so that injuries can be avoided.
The intermittent preventive educational program for personnel, especially the young nurses, should be emphasized. Hospitals should reduce such injuries by establishing desirable work environments through providing sufficient staff and safety equipment, and implement organizational programs.
[1]. Vaz K, McGrowder D, Alexander-Lindo R, Gordon L, Brown P, Irving R, Knowledge, awareness and compliance with universal precautions among health care workers at the University Hospital of the West Indies, JamaicaInt J Occup Environ Med 2010 1(4):171-81. [Google Scholar]
[2]. Gourni P, Polikandrioti M, Vasilopoulos G, Mpaltzi E, Gourni M, Occupational Exposure to blood and body fluids of nurses at Emergency departmentHealth Sci J 2012 6(1):60-68. [Google Scholar]
[3]. Honda M, Chompikul J, Rattanapan C, Wood G, Klungboonkrong S, Sharps injuries among nurses in a Thai regional hospital: prevalence and risk factorsInt J Occup Environ Med 2011 2(4):215-23. [Google Scholar]
[4]. Jahan S, Epidemiology of needlestick injuries among health care workers in a secondary care hospital in Saudi ArabiaAnn Saudi Med 2005 25(3):233-38. [Google Scholar]
[5]. Chow J, Rayment G, Wong J, Jefferys A, Suranyi M, Needle-stick injury: a novel intervention to reduce the occupational health and safety risk in the haemodialysis settingJ Ren Care 2009 35(3):120-26. [Google Scholar]
[6]. Taleet M, Kandeel A, El-Shoubary W, Bodenschatz C, Khairy I, Oun S, Occupational exposure to needlestick injuries and hepatitis B vaccination coverage among health care workers in EgyptAm J Infect Control 2003 31(8):469-74. [Google Scholar]
[7]. Zhang M, Wang H, Miao J, Du X, Li T, Wu Z, Occupational exposure to blood and body fluids among health care workers in a general hospital, ChinaAm J Ind Med 2009 52(2):89-98. [Google Scholar]
[8]. Hassanpour Dehkordi A, Mohammadi N, NikbakhtNasrabadi A, Hepatitis-related stigma in chronic patients: A qualitative studyAppl Nurs Res 2015 29:206-10. [Google Scholar]
[9]. Nsubuga FM, Jaakkola MS, Needle stick injuries among nurses in sub-Saharan AfricaTrop Med Int Health 2005 10(8):773-81. [Google Scholar]
[10]. Mohammadi N, Hassanpour Dehkordi A, Nikbakhat Nasrabadi A, Iranian patients with chronic hepatitis struggle to do self-careLife Sci J 2013 10(1):457-62. [Google Scholar]
[11]. Gershon RR, Mitchell C, Sherman MF, Vlahov D, Lears MK, Felknor S, Hepatitis B vaccination in correctional health care workersAm J Infect Control 2005 33(9):510-18. [Google Scholar]
[12]. Hassanpour Dehkordi A, Mohammadi N, NikbakhtNasrabadi A. Self-care in patients with chronic hepatitis: Redesigning Orem’s self-care theory. Faculty of Nursing and Midwifery, Tehran University of Medical Sciences, PhD Thesis, 2013 [Google Scholar]
[13]. Hassanpour Dehkordi A, The concept of self-care in patients diagnosed with chronic hepatitis: a Rodgers evolutionary approachJ Urmia Nurs Midwifery Faculty 2014 12(6):477-90. [Google Scholar]
[14]. Shiao JSC, Lin MS, Shih TS, Jagger J, Chen CJ, National incidence of percutaneous injury in Taiwan healthcare workersRes Nurs Health 2008 31(2):172-79. [Google Scholar]
[15]. Hassanpour Dehkordi A, Khaledi Far A, Effect of exercise training on the quality of life and echocardiography parameter of systolic function in patients with chronic heart failure: a randomized trialAsian J Sports Med 2015 6(1):e22643 [Google Scholar]
[16]. Merchant RC, Update on emerging infections: news from the Centers for Disease Control and Prevention. Updated U.S. Public Health Service guidelines for the management of occupational exposures of HIV and recommendations for postexposure prophylaxisAnn Emerg Med 2006 47(5):492-95. [Google Scholar]
[17]. Rodrigues C, Needle stick injuries & the health care worker–the time to act is nowIndian J Med Res 2010 131:384-86. [Google Scholar]
[18]. Tadesse M, Tadesse T, Epidemiology of needlestick injuries among health-care workers in Awassa City, Southern EthiopiaTrop Doct 2010 40(2):111-13. [Google Scholar]
[19]. Wilburn SQ, Eijkemans G, Preventing needlestick injuries among healthcare workers: A WHO-ICN collabourationInt J Occup Env Heal 2004 10(4):451-56. [Google Scholar]
[20]. Norsayani MY, Hassim IN, Study on incidence of needle stick injury and factors associated with this problem among medical studentsJ Occup Health 2003 45(3):172-78. [Google Scholar]
[21]. Lotfi R, Gashtasbi A, Needle stick and sharps injuries and its risk factors among health center personnel (Astara Iran, 2006)J Babol Univ Med Sci 2008 10(4):71-77. [Google Scholar]
[22]. Smith DR, Wei N, Wang RS, Needlesticks and Sharps Injuries Among Chinese Hospital NursesAdv Exp Prev 2004 7(1):11-12. [Google Scholar]
[23]. Ashat M, Bhatia V, Puri S, Thakare M, Koushal V, Needle stick injury and HIV risk among health care workers in North IndiaIndian J Med Sci 2011 65(9):371-78. [Google Scholar]
[24]. Yenesew MA, Fekadu GA, Occupational exposure to blood and body fluids among health care professionals in bahir dar town, northwest ethiopiaSaf Health Work 2014 5(1):17-22. [Google Scholar]
[25]. Rampal L, Zakaria R, Sook LW, Zain AM, Needle stick and sharps injuries and factors associated among health care workers in a Malaysian hospitalEur J Soc Sci 2010 13(3):354-62. [Google Scholar]
[26]. Bijani B, Azimian J, Soleymani M, Mohammadi N, Epidemiology and risk factors of needle stick injuriesJ Shahid Beheshti School Nurs Midwifery 2013 22(78):1-9. [Google Scholar]
[27]. Habib H, Khan EA, Aziz A, Prevalence and factors associated with needle stick injuries among registered nurses in public sector tertiary care hospitals of pakistanInt J Collabourative Res Intern Med Public Health 2011 3(2):124-30. [Google Scholar]
[28]. Martins A, Coelho AC, Vieira M, Matos M, Pinto ML, Age and years in practice as factors associated with needlestick and sharps injuries among health care workers in a Portuguese hospitalAccident Anal Prev 2012 47:11-15. [Google Scholar]
[29]. Jagger J, Hunt EH, Pearson RD, Sharp object injuries in the hospital: causes and strategies for preventionAm J Infect Control 1990 18(4):227-31. [Google Scholar]
[30]. McGeer A, Simor AE, Low DE, Epidemiology of needlestick injuries in house officersJ Infect Dis 1990 162(4):961-64. [Google Scholar]
[31]. Dessie M, HIV infection among orthopedic in-patients at dil chora referral hospital, ethiopiaEast Cent Afr J Surg 2010 15(1):78-80. [Google Scholar]
[32]. Gatley M, Worsley M, Preventing needlestick injuriesBMJ 1991 302(6785):1147 [Google Scholar]
[33]. Parsa-Pili J, Izadi N, Golbabaei F, Factors associated with needle stick and sharp injuries among health care workersInt J Occup Hyg 2014 5(4):191-97. [Google Scholar]
[34]. Afridi AA, Kumar A, Sayani R, Needle stick injuries–risk and preventive factors: a study among health care workers in tertiary care hospitals in PakistanGlob J Health Sci 2013 5(4):85-92. [Google Scholar]
[35]. Aiken LH, Sloane DM, Klocinski JL, Hospital nurses’ occupational exposure to blood: prospective, retrospective, and institutional reportsAm J Public Health 1997 87(1):103-07. [Google Scholar]
[36]. Goldwater PN, Law R, Nixon AD, Officer JA, Cleland JF, Impact of a recapping device on venepuncture-related needlestick injuryInfect Control Hosp Epidemiol 1989 10(1):21-25. [Google Scholar]
[37]. Asadi Noughabi AA, Zandi M, Mehran A, Alavian M, Hasanpour Dehkordi A, The assessment of education’s effect on quality of life in patients under p-d feron treatmentRazi J Med Sci 2007 14(56):21-28. [Google Scholar]