Pregnancy with Pemphigoid Gestationis: A Rare Entity
Anshuja Singla1, Sneha Shree2, Sumita Mehta3
1 Assistant Professor, Department of Obstetrics and Gynecology, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India.
2 Senior Resident, Department of Obstetrics and Gynecology, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India.
3 Senior Specialist, Department of Obstetrics and Gynecology, Babu Jagjivan Ram Hospital, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anshuja Singla, Assistant Professor, Department of Obstetrics and Gynecology, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi-110095, India.
E-mail: dranshuja@gmail.com
Pemphigoid Gestationis (PG) is a rare autoimmune blistering disease with an incidence of 1/50000 pregnancies. Presentation in the second or third trimester is most common and tends to recur in subsequent pregnancies with earlier onset and a more severe course. Direct Immunofluorescence (DIF) staining is confirmatory on skin biopsy specimen. A 24-year-old female presented at 6 months period of gestation with increased blood pressure records. On examination, there were fresh bullous lesions along with old healed scar marks on the abdomen and limbs. Termination of pregnancy was done due to high BP. Patient delivered a fresh still birth weighing 750 gm. No postpartum flare ups were seen and she was discharged on prednisolone in a satisfactory condition.
Autoimmune, Dermatosis, Direct immunofluorescence, Prednisolone, Pruritus
Case Report
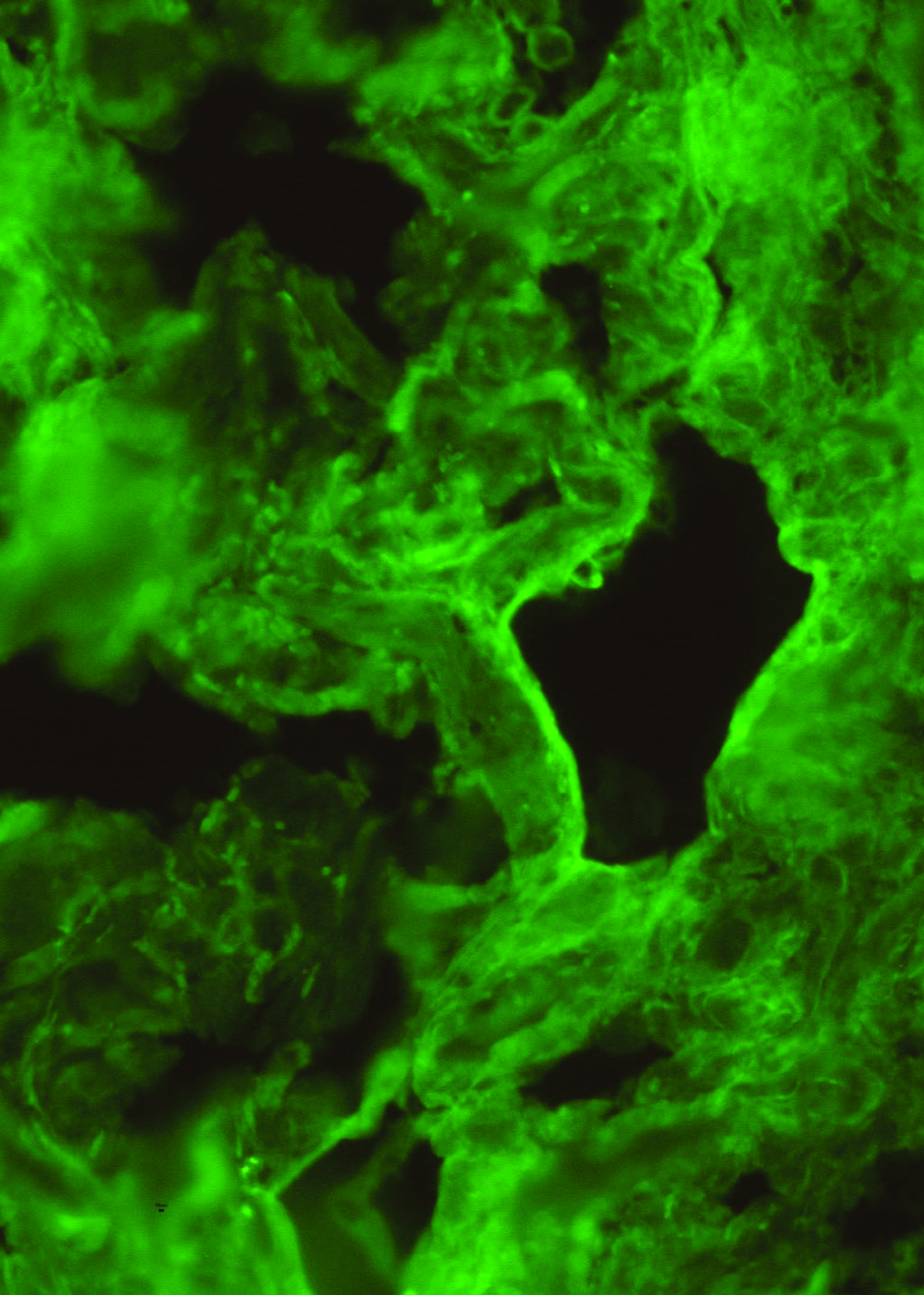
A 24-year-old unbooked G2P1L0 (2nd gravida, para 1 but no living issue) presented at 6 months amenorrhea with increased Blood Pressure (BP) records. She was diagnosed Pemphigoid Gestationis (PG) in her first pregnancy after confirmation on skin biopsy and direct immunofluorescence (DIF) [Table/Fig-1]. There were no postpartum flare-ups though she continued irregular and self medication of prednisolone. On examination, there were fresh bullous lesions along with old healed scar marks on the abdomen and limbs [Table/Fig-2,3]. Uterus corresponded to 24-26 weeks of gestation with a single live fetus. She was started on antihypertensive drugs and dermatology review was done. Prednisolone (15 mg OD) was started. Strict maternofetal surveillance was done. Her haemogram, RFT, liver function tests, fundus and ultrasound for kidneys were normal. Due to uncontrolled BP, decision for termination was taken. Patient delivered a still birth weighing 750 gm. No postpartum flare ups of PG were noted. She was discharged on prednisolone in a satisfactory condition.
Immunofluorescence stain showing C3 positive at dermoepidermal junction (X 250).
Old healed scar marks along with a few fresh lesions over lower limbs.

Fresh bullous lesions over abdomen.

Discussion
Pemphigoid Gestationis (PG) also known as herpes gestationis is a rare autoimmune blistering disease with an incidence of 1/50000 pregnancies [1]. Presentation in the second or third trimester is most common and tends to recur in subsequent pregnancies with earlier onset and a more severe course [1,2]. Pathogenesis is autoimmune with damage to dermoepidermal junction leading to blister formation. The inciting event is unknown [3]. Presentation of PG is variable with pruritus being the main symptom and patients present with erythematous urticarial plaques which progress to tense blisters and bullae. Periumbilical area is usually the first site of involvement with sparing of face and mucus membranes. Main differential diagnosis is Polymorphic Urticarial Papules and Plaques of Pregnancy (PUPPP). The confirmatory diagnosis is by DIF staining on skin biopsy specimen [2].
The course of disease is unchanged in pregnancy. Usually remittance is noted in the postpartum period, though exacerbations have been documented with subsequent pregnancies, menstruation and OCP use [2]. Fetal growth restriction and premature delivery (20%) and neonatal skin involvement (10%) have been seen [1]. Thomas et al., report a case of PG that presented for the first time in the postpartum period, associated with a low birth weight baby [4]. The condition responds to topical and oral glucocorticoids and oral antihistamics. A high index of suspicion of such a rare dermatosis should be kept in mind in a pregnant woman with dermatological lesions. Steroid use is associated with a good prognosis.
Conclusion
PG is a rarely reported disease. We intend, by reporting this, that clinicians should have awareness regarding this condition when a patient presents with such lesions so that treatment should be started early as the disease responds well to steroids. Also, these cases should not be missed as postpartum flare-ups have also been observed.
[1]. Semkova K, Black M, Pemphigoid gestationis: current insights into pathogenesis and treatmentEur J Obstet Gynecol Reprod Biol 2009 145:138 [Google Scholar]
[2]. Jenkins RE, Clinical features and management of 87 patients with pemphigoid gestationisClin Exp Dermatol 1999 24:255 [Google Scholar]
[3]. Al-Fouzan AS, Galadari I, Oumeish OY, Herpes gestationis (pemphigoid gestationis)Clin Dermatol 2006 24:109-12. [Google Scholar]
[4]. Thomas S, Rajan U, George S, George M, CASE REPORT: Postpartum pemphigoid gestationisIndian Journal of Dermatology 2012 57(2):146-48. [Google Scholar]