The Earliest Presenting Umbilical Port Site Hernia Following Laparoscopic Cholecystectomy: A Case Report
Rajeev Sharma1, Deeksha Mehta2, Manav Goyal3, Sanjay Gupta4
1 Professor, Department of General Surgery, Government Medical College and Hospital, Chandigarh, Punjab, India.
2 Senior Resident, Department of General Surgery, Government Medical College and Hospital, Chandigarh, Punjab, India.
3 Junior Resident, Department of General Surgery, Government Medical College and Hospital, Chandigarh, Punjab, India.
4 Assistant Professor, Department of General Surgery, Government Medical College and Hospital, Chandigarh, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Deeksha Mehta, 11-A, Harbans Nagar, Jalandhar City, Punjab-144002, India.
E-mail: deeksha_doc@yahoo.co.in
Port site hernia after laparoscopic surgery is a rare complication. Here we present a case of a 55-year-old female, diagnosed with an anterior abdominal wall hernia through the 10mm umbilical port, just two days after her laparoscopic cholecystectomy. The uniqueness of this case is its extremely early presentation. Patient presented with features of acute intestinal obstruction and due to prompt diagnosis and timely intervention, she underwent a successful reduction of hernia and an anatomical repair of the fascial and peritoneal defect through the midline laparotomy incision.
Acute intestinal obstruction, Midline laparotomy incision, Pregangrenous gut loop
Case Report
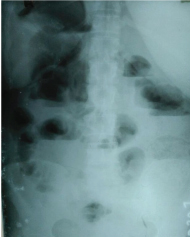
A 55-year-old female presented to emergency surgery ward with complaints of pain abdomen, distension abdomen, obstipation and two episodes of bilious vomiting since one day. Pain was diffusely present in whole abdomen. On examination, tenderness was present in the whole abdomen with specific guarding present in the periumbilical area. There was a gurgling sensation just beneath the skin indicating the possibility of an obstructed gut loop which was found to be irreducible. She had undergone laparoscopic cholecystectomy at our institute two days back and was discharged just one day back. Her routine hematological and biochemical workup was found within normal limits. Ultrasonogram (USG) abdomen [Table/Fig-1] indicated only the dilated small bowel loops all over abdomen and missed out on any midline fascial defect. Abdominal radiographs revealed air fluid levels in the erect film [Table/Fig-2] and grossly dilated bowel loops in the supine film [Table/Fig-3], concentrated in the centre of the films indicating acute small intestinal obstruction. She was not subjected to the Contrast Enhanced Computerized Tomography (CECT) abdomen due to a clear cut obstructed herniated bowel loop palpable at the umbilical port on clinical examination and the patient was directly taken up for the surgery [Table/Fig-4].
Report of the ultrasound abdomen of the patient.
Xray abdomen erect of the patient.
X-ray abdomen supine of the patient.

Intestinal loop seen obstructed at the fascial defect.
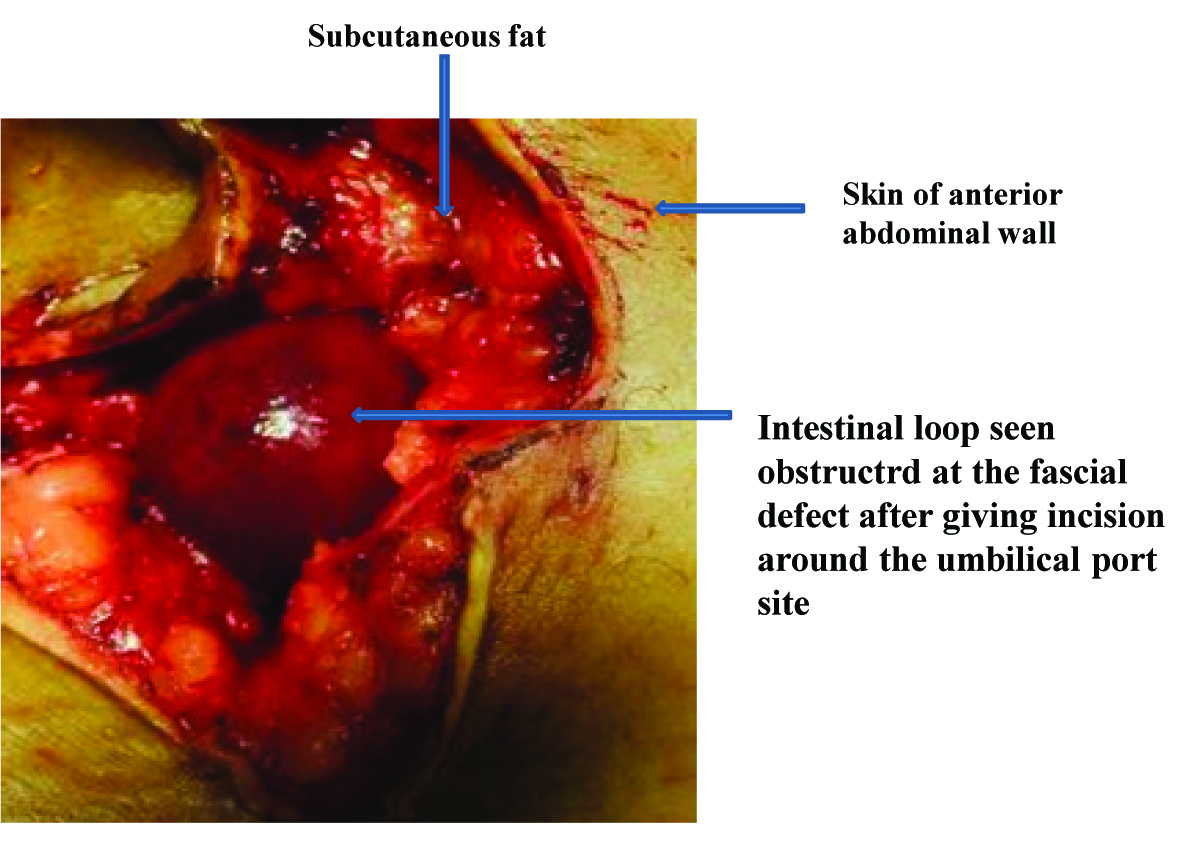
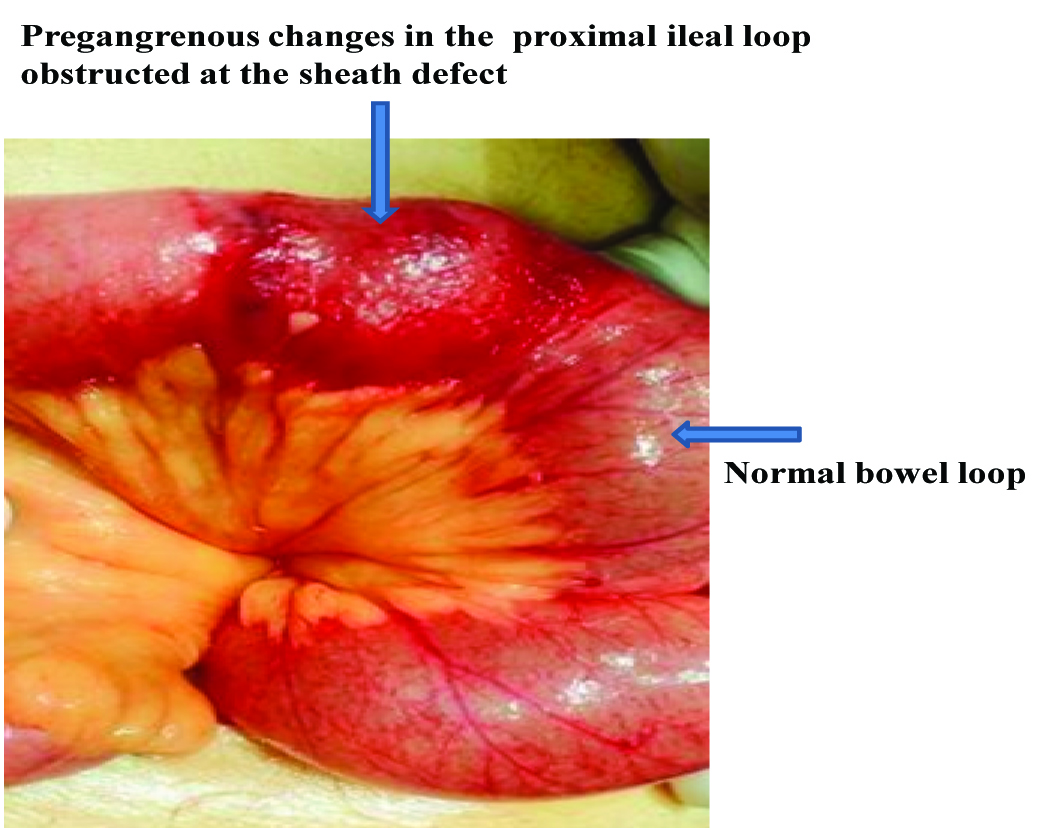
Surgery was taken up under general anaesthesia. The abdomen was opened through the midline laparotomy incision extending few centimeters above and below the umbilicus. Cherry coloured gut loop was found lying just below the skin, herniating out of the peritoneal and the fascial defect at the umbilical port site. The loop was obstructed at the fascial defect. The defected fascia and the peritoneum were carefully opened and the loop was delivered out. Pregangrenous changes were present at the part of the loop stuck at the defect [Table/Fig-5]. The proximal bowel was grossly dilated while the distal bowel was somewhat collapsed. The obstructed area was approximately one foot from the ileocaecal junction. Approximately 500 to 600 ml of dark red oedema fluid was also drained from the peritoneal cavity. The pregangrenous part of the ileum was kept under the warm saline soaked sponge and the patient was given 100% oxygen for full 5 minutes. The colour and the peristalsis of the gut loop were rechecked and were found to have grossly improved. The small intestine was decompressed antegrade and retrograde, the wash given and the abdomen was closed in layers with the proper anatomical repair of the fascia and the peritoneum. The patient remained well in the postoperative period and the bowel sounds returned on the third postoperative day and the patient passed stools and flatus on the fourth postoperative day. Patient was allowed liquids on the third postoperative day and was discharged on full oral diet and treatment on the seventh postoperative day with a healthy stitch line.
Pregangrenous changes in the proximal ileal loop
Discussion
Incisional hernia is a well known complication after any open abdominal surgery. This is a rare complication that can also occur after laparoscopic surgeries. The incidence of port site hernia after laparoscopic surgery lies between 0.38% to 5.4% with overall incidence of 1.7% [1]. Incidence of port site hernia increases with the size of the trocar [1]. There are other risk factors also involved in causing port site hernia like the incision enlargement, the wound infection, diabetes mellitus, obesity, the type of trocar used, male sex, connective tissue disorders and most importantly the defective closure of the fascial defect at the port site [2]. There are reports of herniation occurring even via the peritoneal defects below the repaired fascial layer. Therefore the fascial as well as the peritoneal repair of port sites should be done wherever safely possible. In our case at the time of laparoscopic cholecystectomy, umbilical port was inserted by 10mm trocar by the open technique as a part of protocol followed by our surgical unit. The open technique of insertion though a safer technique than closed, is more notorious for causing hernia. Though laparoscopic surgery offers an important contribution to the reduction of all the typical complications related to open surgery, it can be associated with a specific type of incisional hernia through the trocar site causing complications such as small bowel obstruction [3]. Port-site hernia can cause a whole range of presentations ranging from being asymptomatic to serious complication like strangulated bowel hernia. The interval between operation and diagnosis of port site hernia varies considerably. Asymptomatic patient may present very late. The bowel involvement can occur in the form of bowel incarceration, bowel obstruction or bowel evisceration. All these are considered surgical emergencies that can present few days to weeks after surgery [4]. Our case is probably the earliest presenting obstructed port site incisional hernia, so far reported in the literature. Such an early presentation in our case was probably due to inadequate fascial closure at the umbilical port site. So, this case further authenticates the need for proper fascial closure at the port site to prevent the development of hernia later. Direct repair of the port site is the conventional method of the closure of the port-site. Many other newer methods are being introduced like 2 S-retractor technique [5], using skin hooks in sheaths, using modified aptos needle technique etc. In addition, a newer technique of port plug with a bioabsorbable hernial plug, without suturing has also been introduced.
Conclusion
So, it would be safe to conclude that the possibility of port site hernia after laparoscopic cholecystectomy should be kept in mind while checking on a follow up case of laparoscopic cholecystectomy. Prompt intervention in a case of suspected hernia can surely reduce the dreaded events like the strangulation and the sepsis. So, to prevent such an unfavourable situation at a later date, the fascial as well as the peritoneal layers should always be repaired at the port site.
[1]. Bunting D, Port-site hernia following laparoscopic cholecystectomyJSLS 2010 14:490-97. [Google Scholar]
[2]. Comajuncosas J, Hermoso J, Gris P, Risk factors for umbilical trocar site incisional hernia in laparoscopic cholecystectomy: A prospective 3-year follow up studyAm J Surg 2014 207(1):1-6. [Google Scholar]
[3]. Pamela D, Roberto C, Francesco LM, Umberto M, Carla M, Vincenzo N, Trocar site hernia after laparoscopic colectomy: a case report and literature reviewISRN Surgery 2011 2011:725601:7 [Google Scholar]
[4]. Khurshid N, Chung M, Horrigan T, Manahan K, Geisler JP, 5- millimeter trocar-site bowel herniation following laparoscopic surgeryJSLS 2012 16:306-10. [Google Scholar]
[5]. Aziz HH, A simple technique of laparoscopic port closureJSLS 2013 17(4):672-74. [Google Scholar]