Osseous Consolidation of an Aseptic Delayed Union of a Lower Leg Fracture after Parathyroid Hormone Therapy – A Case Report
Ilko Kastirr1, Sebastian Radmer2, Reimer Andresen3, Hans-Christof Schober4
1 Medical Assistant, Institute of Diagnostic and Interventional Radiology/Neuroradiology, Westkuestenklinikum Heide, Germany.
2 Head of the Centre for Orthopaedics, Berlin, Germany.
3 Head of the Institute of Diagnostic and Interventional Radiology/Neuroradiology, Westkuestenklinikum Heide, Germany.
4 Head, Department of Internal Medicine I, Municipal Hospital Suedstadt Rostock, Germany.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ilko Kastirr, Institute of Diagnostic and Interventional Radiology/Neuroradiology, Westkuestenklinikum Heide Esmarchstr. 50, 25746 Heide, Germany.
E-mail: ikastirr@wkk-hei.de
The absence of osseous consolidation of a fracture within the normal time period is defined as delayed union or non-union. Both for the patient and from a socio-economic point of view, impaired fracture healing represents a major problem. Risk factors for a delayed fracture healing are insufficient immobilisation, poor adaptation of the fracture surfaces, interposition of soft tissue in the fracture gap, as well as circulation disturbances, metabolic disease, smoking and infections. In animal studies, a positive effect of parathyroid hormone (PTH) on fracture healing has been shown. PTH has a direct stimulatory effect on osteoblasts and osteoclasts. In addition, it appears to influence the effect of osseous growth factors. Few cases with the empiric off-label use of PTH that showed a tendency to support delayed or non-union fractures have been published. We report about a patient with a fracture of the lower leg and no osseous consolidation after 7 months. Four Months after therapy with 20 μg teriparatide per day for 8 weeks the fracture was consolidated and the patient had regained full and pain free weight bearing capacity of the leg with no reported side effects.
Crural fracture, Impaired bone healing, Off-label use, Teriparatide
Case Report
A 49-year-old, male patient had suffered a distal lower leg fracture in a skiing accident in November of 2010. Osteosynthetic treatment using medullary nails was declined by the patient, so a plate osteosynthesis of the fibula and tibia was performed at the patient’s request. The operation went without complications and there were no post-op infections. In the medical history there were no chronic diseases, no diabetes mellitus and the patient denied a smoking habit or regular medication. The physical examination showed normal vital parameters as well as laboratory values within the normal range; especially the leukocyte count and C-reactive protein were within normal range. With a serum level of > 30 ng/ml, a vitamin D deficiency was ruled out. At 4-week intervals, clinical examinations and conventional X-rays in two planes were performed for follow-up. In the first X-ray follow-up in January 2011, visible but poor callus formation around the fracture site was found and there were no signs of loosening or fracture of the osteosynthesis material and no advancing dislocation of the fracture fragments was seen [Table/Fig-1]. Over the following months the edges of the fractures showed increasing sclerosis with no bone bridges in the fracture gap. The patient reported unaltered levels of pain while putting weight on the leg. Seven months after the fracture event, there was still insufficient consolidation of the fracture [Table/Fig-2], and the patient was only able to place limited weight on the affected limb, leading to pain. The diagnosis of an oligotrophic delayed union was given. As the patient refused to have further surgery an empiric off-label use of parathyroid hormone (PTH) was suggested and explained to him, which the patient agreed to. Therapy was then started with 20μg per day of teriparatide, the 1-34 fragment of recombinant human parathyroid hormone, over a period of 8 weeks. During the follow-up visits the patient reported no side effects and no changes in calcium and phosphate levels were observed. 4 months after completion of the PTH therapy, osseous consolidation of the fractures was observed indicated by bone bridges within the fracture gap. Upon complete and pain-free weight bearing of the leg, the osteosynthesis material was removed [Table/Fig-3]. The patient remained free of symptoms. The therapy was well tolerated and there was no need to discontinue it as no side effects were experienced by the patient.
Plate osteosynthesis of a distal lower leg fracture. Poor initial callus formation in postoperative follow-up.
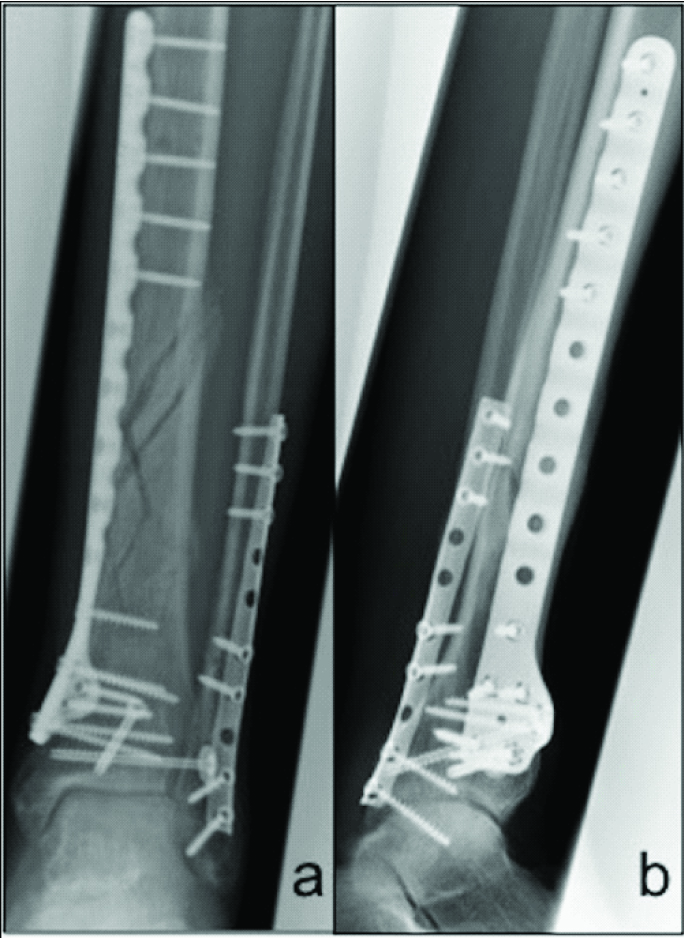
Visible fracture gaps 7 months after fracture. Still inadequate callus formation.
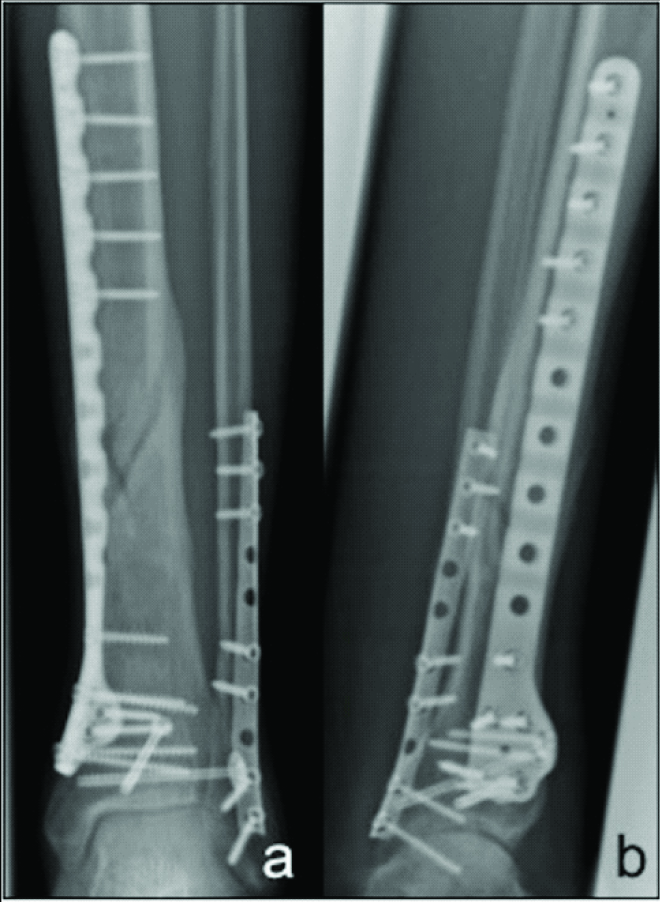
4 months after PTH therapy. Status post removal of the osteosynthesis material. Consolidation of the fracture gaps.

Discussion
The lack of restoration of osseous continuity of a fractured bone for more than 9 months with no signs of progress during the last three months is defined by the US Food and Drug Administration as a non-union. Fractures with a prolongated healing process but with the potential to consolidate are called delayed unions [1,2]. Impairment of fracture healing occurs at rates between 6-16% in fractures of the long bones after both conservative therapy and surgical treatment. An estimate of the normal time to consolidation for tibial shaft fractures lies around 4 months. For the patient this means immobility, persistent pain and thus a loss of quality of life, reduced productivity and potentially a loss of income. The healthcare system is burdened with costs for further operations, medication, hospitalisation and absence from work [1–3].
The healing of a bone after a fracture requires a well-regulated interplay of biochemical and biomechanical processes. In primary bone healing osteoclasts can directly overcome the fracture gap and create Haversian canals and osteoblast can fill the defect with lamellar bone. The much more common secondary fracture healing, in which the fracture ends diverge, with bleeding into and collection of bone and cell debris in the fracture gap, takes place in several phases. In the inflammatory phase, immune cells, and platelets are activated by the metabolites of the fracture haematoma. Mesenchymal stem cells are stimulated to differentiate into fibroblasts, chondroblasts and osteoblasts. A network of fibrin threads, collagens and sprouting capillaries develops and bridges the fracture ends. Osteoblasts fill the spaces with osteoid and activated chondroblasts form hyaline cartilage around the fracture gap. Hardening of the callus occurs through the incorporation of hydroxylapatite. In the final phase of remodelling, the woven bone is transformed into lamellar bone by migrating osteoclasts and osteoblasts, which recreate the original stability [4,5].
In each phase, disturbances can impair or interrupt bone healing. Large-scale necrosis, a lack of vascularisation or poor circulation due to diabetes mellitus and smoking or PAOD, but also infections or medication such as NSAIDs, corticosteroids or cytostatics can impair callus formation in the inflammatory phase. If there is a lack of fracture healing accompanied by missing or insufficient callus formation, one refers to it as an atrophic or oligotrophic non-union [1,3].
Inadequate immobilisation of the fracture can impede healing. Excessive movement of the fracture ends can promote the formation of fibrous tissue in the fracture gap and prevent ossification [5]. As a reaction to instability, an excessive formation of callus tissue around the fracture gap is often seen, but this does not correspond to better stability. In these cases, one refers to as hypertrophic non-union. Other biochemical factors can have a negative effect on fracture healing, e.g., a vitamin D deficiency can prevent calcification of the bone matrix formed. Osteoporosis, malnutrition, anaemia, chronic hypoxia and increased age have been described to limit the healing capacity [1,5].
To improve bone healing, local procedures such as the implantation of autologous or allogeneic bone or bone substitute materials and/or the intraoperative injection of growth factors into the fracture gap have been applied for a number of years. The experimental use of osteoporosis medications such as bisphosphonates or strontium ranelate in several studies has shown that they can have a positive effect on callus size and durability. However, both substances inhibit bone resorption and may thus have an inhibitory effect in the phase of remodelling [2,3,6].
For more than 10 years, parathyroid hormone has been used for fracture prophylaxis in osteoporosis. In controlled, double-blind, randomised studies, an accelerating effect of PTH on the healing of pelvic, femoral neck and distal radial fractures has been observed in postmenopausal women. In various different animal experimental studies of different fracture models, it was shown that the administration of PTH accelerates fracture healing and increases the callus volume and mineral salt content in the fracture area, while simultaneously increasing the resistance to traction [2,6–9]. PTH intervenes at different points of bone metabolism. On the one hand, by stimulating vitamin D synthesis in the kidneys, it leads to an increased uptake of calcium in the intestines, which is required for mineralisation of the bone matrix. It has been shown that PTH can stimulate the differentiation of osteoblasts and chondroblasts [10]. Whereas the physiological effect mainly comprises an activation of the osteoclasts for bone resorption, intermittently administered PTH can shift the relation of bone resorption and genesis via a direct activation of osteoblasts in the direction of osteogenesis [2,3,6,10]. PTH thus plays a central role in the coupling of osteogenesis and osteolysis and is an important regulator in the process of remodelling. These properties suggest that it would be suitable for application in the treatment of non-unions. A possible positive effect of PTH on the healing of non-unions has already been observed in a few case in which it has been given as an empiric off-label treatment. For example non-unions of femoral and humeral shaft fractures have shown clinical improvement and radiologic evidence of consolidation of the fractures with no side effects experienced by the patients [1–3,11].
In the case reported here after a fracture of the lower leg and osteosynthetic treatment, callus formation was visible but poor and the patient did not experience consolidation or pain-free weight bearing of the affected leg. As the patient did not show any signs of infection or metabolic and biological risk factors, a failure of the suboptimal osteosynthesis and thus insufficient immobilisation is probably responsible for development of the delayed union. The formation of fibrotic tissue promoted by the excessive movements may have been the reason for the lack of consolidation in this case [5]. A PTH-mediated, increased activation and differentiation of osteoblasts in the fracture gap would conceivably explain the fracture healing after therapy.
Conclusion
The consolidation of a delayed union of the lower leg fracture after PTH therapy shown here supports the observations of other authors that the intermittent administration of PTH can promote the healing of impaired union fractures. As the present case report concerns a single patient, it cannot be proven that healing would not have occurred without PTH therapy. Further studies with larger patient populations for dose finding and with a control group to verify the effect of PTH, e.g., using osteogenic markers, will have to be conducted in the future in order to confirm the positive tendency.
[1]. Paridis D, Karachalios T, Atrophic femoral bone non-uniontreated with 1-84 PTHJ Musculoskelet Neuronal Interact 2011 11(4):320-23. [Google Scholar]
[2]. Pietrogrande L, Raimondo E, Teriparatide in the treatment of non-unions: Scientific and Clinical EvidencesInjury 2013 44(1):54-57. [Google Scholar]
[3]. Brunnemann CE, Reisinger EC, Ganzer D, Schober HC, Parathyroid hormone injection to counteract delayed bone fracturesDtsch Med Wochenschr 2010 135(31/32):1538-41. [Google Scholar]
[4]. Marsell R, Einhorn TA, The Biology of fracture healingInjury 2011 42(6):551-55. [Google Scholar]
[5]. Haffner-Luntzer M, Liedert A, Ignatius A, Mechanobiology and bone metabolism: Clinical relevance for fracture treatmentUnfallchirurg 2015 118(12):1000-06. [Google Scholar]
[6]. Barvencik F, Medication and bone metabolism: Clinical importance for fracture treatmentUnfallchirurg 2015 118(12):1017-24. [Google Scholar]
[7]. Aspenberg P, Genant HK, Johansson T, Nino AJ, See K, Krohn K, Teriparatide for acceleration of fracture repair in Humans: A prospective, randomized, double-blind study of 102 postmenopausal women with distal radial fracturesJBMR 2010 25(2):404-14. [Google Scholar]
[8]. Holzer G, Majeska RJ, Lundy MW, Hartle JR, Einhorn TA, Parathyroid hormone enhances fracture healing. A preliminary reportClin Orthop Relat Res 1999 366:258-63. [Google Scholar]
[9]. Della Rocca GJ, Crist BD, Murtha YM, Parathyroid hormone: is there a role in fracturehealing?J Orthop Trauma 2010 24:31-35. [Google Scholar]
[10]. Chen G, Deng C, Li YP, TGF-β and BMP signaling in osteoblast differentiation and bone formationInt J Biol Sci 2012 8(2):272-88. [Google Scholar]
[11]. Oteo-Alvaro A, Moreno E, Atrophyc humeral shaft non-union treated with teriparatide (rh PTH 1-34): A case reportJ Shoulder Elbow Surg 2010 19:22-28. [Google Scholar]