Cervical cancer is a major cause of mortality from cancer among women, especially in the developing world. Prevalence of cervical cancer has decreased significantly with the use of screening methods like the Pap test [1]. Colposcopy is an important diagnostic tool in the evaluation of patients with abnormal Pap smears. During a colposcopy procedure, it is crucial to visualize the entire transformation zone (TZ) as almost all manifestations of cervical carcinogenesis occur there. In roughly 10-20% of all patients, the entire transformation zone is not completely visualized [2–4], rendering the colposcopic examination incomplete and inconclusive. In such patients, cone biopsy is warranted for further diagnosis and management. Conization procedure carries significant morbidity, with potential complications like bleeding, infection and incompetent cervix. In order to minimize the use of conization and its associated complications, various techniques are used to improve the visualization of transformation zone like the use of endocervical speculums, osmotic dilatation and agents such as misoprostol and estradiol. In the present study, comparison of vaginal versus oral estradiol was done in overcoming non- visualization of the transformation zone.
Materials and Methods
The present study was a prospective randomized controlled trial conducted at a tertiary care hospital in New Delhi, India between 2009 and 2011. The study was conducted according to the principles of the Declaration of Helsinki and was approved by institutional ethical committee. Informed consent was taken from all the subjects. Sample size calculation was performed as per following hypothesis: based on a previous study by Aggarwal et al., assuming the difference in the efficacy of misoprostol compared to placebo in improving the visualization of the TZ to be 48.9% (78.9% with misoprostol and 30% with placebo), an alpha error of 0.05% and power of 80%, the study would require a minimum of 40 subjects who would be randomized into two groups [5].
Based on the initial clinical evaluation, 250 patients were screened with colposcopy. Indications for colposcopic examination included: unhealthy/ suspicious looking cervix on speculum examination, persistent discharge per vaginum not responding to conservative therapy, postcoital bleeding and postmenopausal females with inflammatory Pap smear. Pap smear examination was performed in all the study subjects. Of these, 40 patients who were found to have partial/non-visualization of transformation zone on colposcopic examination were serially recruited for the study. Recruitment was stopped once the minimum sample size criterion was met. Further, these subjects were allocated into two groups by a computerized randomization. In Group I, 25 μg Estradiol (E2, Sun Pharma) tablets were administered intravaginally by the patients for seven consecutive days and a repeat colposcopy was done on day 8. In group II, patients were prescribed 25μg of oral Estradiol (Lynoral, Sun Pharma) daily for seven consecutive days and a repeat colposcopy was done on day 8. The efficacy of the 2 regimens in improving the visualization of TZ and their adverse effect profile were compared. In addition, following prespecified subgroup analysis was done for the following: lips of the cervix (anterior or posterior) responding or not responding to the regimen. All abnormal areas (with Reid’s score ≥3) visualized on the cervix were biopsied and sent for histopathological examination. All patients who had persistent incomplete colposcopy despite the study drug administration underwent a colposcopy directed biopsy with endocervical curettage.
Following patients were excluded from the study: pregnant women, females with history of breast cancer, women with obvious growth on the cervix, females with coagulation disorders and hypertensive patients.
Results
Out of the total 250 patients screened with colposcopy, 40 had incomplete colposcopy exam due to either partial or non-visualization of the entire TZ, giving an overall incidence of incomplete colposcopy to be 16% [Table/Fig-1]. Mean age in Groups I and II was 44±3.4years and 46±2.6 years respectively (p-value 0.2). Both the groups were comparable in age distribution, parity and menstrual status [Table/Fig-2]. The efficacy of vaginal estradiol regimen was 70% as compared to 50% with the oral estradiol in overcoming incomplete colposcopy. However the difference was not statistically significant [Table/Fig-2]. Major adverse effects in the two groups included nausea and discharge per vaginum and their incidence was comparable [Table/Fig-2]. The response to the drug in relation to site of incomplete colposcopy has been described in [Table/Fig-3] and the final outcome for all patients is depicted in [Table/Fig-4].
Distribution of unsatisfactory colposcopy in patients screened for the study.
| Menstrual status | Unsatisfactory colposcopy(n=40) | Satisfactory colposcopy(n=210) | Total(n=250) |
|---|
| Premenopausal | 15(7.3%) | 189(92.7%) | 204 |
| Postmenopausal | 25(54% | 21(46%) | 46 |
Patient characteristics, drug efficacy and adverse effects for two study groups.
| Characteristics | Variables | Group-I (vaginal estradiol)n (%) | Group- II (Oral Estradiol)n(%) | p-value |
|---|
| Age distribution (in years) | ≤30 | 2(10) | 3(15) | 0.8 |
| 31-40 | 5(25) | 5(25) |
| 41-50 | 4(20) | 3(15) |
| ≥50 | 9(45) | 9(45) |
| Parity | ≤1 | 1(5) | 1(5) | 0.9 |
| 2 | 4(20) | 6(30) |
| ≥3 | 15(75) | 13(65) |
| Drug efficacy | Satisfactory colposcopy on repeat exam | 14(70) | 10(50) | 0.19 |
| Unsatisfactory colposcopy on repeat exam | 6(30) | 10(50) |
| Drug safety | All adverse effects | 4(20) | 5(25) | 0.8 |
| Nausea | 1(5) | 4(20) | 0.8 |
| Discharge per vaginum | 3(15) | 1(5) | 0.06 |
Correlation between site of unsatisfactory colposcopy and response to the drug in two groups
| Invisibility of transformation zone | No. of responders/total no. of patients : Group-I | No. of responders/total no. of patients : Group-II |
|---|
| On anterior lip | 3/4(75%) | 3/4(75%) |
| On PosteriorLip | 4/4(100%) | 2/6(33%) |
| Both lips | 7/12(58%) | 5/10(50%) |
| p=0.2(Chi-Square Test) | p=0.4(Chi-Square Test) |
Final Outcome in all patients.

Discussion
Colposcopy has been an important method for evaluation of patients with abnormal Pap smear. According to the latest IFCPC [6] (International Federation Cervical Pathology and Colposcopy) guidelines, colposcopy examination should be assessed for 3 variables: adequate or inadequate with the reason cited (e.g., cervix obscured by blood/scarring), visibility of squamo-columnar junction and the transformation zone type. If the transformation zone/squamo-columnar junction is not completely visualized, it becomes necessary to perform conization. Such procedures are associated with significant morbidity and also, an adverse effect on reproductive potential. There have been few trials [7–10], which explored the utility of estrogens in improving visualization of the transformation zone during colposcopy. In a study by Saunders et al., 34 patients with partial or non-visualized transformation zone were administered either 30 μg of estradiol or placebo tablets daily for 10 consecutive days [7]. The overall response rate with estrogen was 65% versus 10% with the placebo (p<0.05). In a separate non-randomized study by Prednivilli et al., 100 μg of oral estradiol administered for 5 consecutive days allowed complete visualization of TZ in 16 out of 25 patients with previously non-visualized TZ (response rate of 64%) [8]. Nausea was the only reported adverse effect.
There have been few studies elucidating the efficacy of intravaginal estrogen administration in improving the visualization of TZ on colposcopy. Recently, Piccolo et al., studied 178 postmenopausal women who had partial or non-visualized TZ during colposcopy [9], of which 3-month intravaginal administration of estrogen resulted in a complete visualization of TZ in 73% of the patients during the follow-up colposcopy.
In another study by Richards et al., 54 patients with abnormal cervicovaginal smears with hypo-estrogenic state (postmenopausal or amenorrheic postnatal)) underwent colposcopic examination [10]. All of them had partial or non-visualized TZ and were treated with local estrogen cream applied twice a week for 6 weeks. A 32 of them had complete visualization of the TZ on follow up colposcopy. In addition, 40 patients had a normal pap smear after therapy. The authors concluded that the use of vaginal estrogen cream improves the visualization of transformation zone in colposcopy and also the accuracy of prediction of true pre-invasive disease.
In a recent randomized controlled trial conducted by us [4], a single dose of 200μg vaginal misoprostol was successful in 70% of patients in overcoming the non-visualization of TZ during colposcopy as compared to 82% with the administration of 50μg vaginal estradiol for 7 consecutive days. However, this difference was statistically non-significant.
In the present study, the efficacy of vaginal estradiol was 70% as compared to 50% with oral estradiol. Different dosages of estrogens have been used for a varying duration in different studies [4,7–10]. No single regimen has been found to be significantly superior to the others in improving the visualization of the TZ. In the present study, administration of the minimum possible dose of estradiol was done in order to minimize the incidence of side effects.
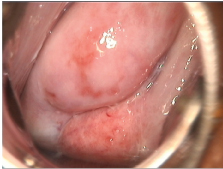
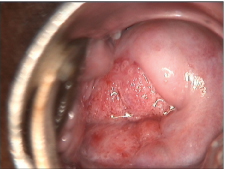
It is important to note that estradiol enabled complete visualization of the TZ in majority of the subjects, irrespective of route of administration [Table/Fig-5,6]. There is strong evidence that gonadal steroid hormones are important in regulation of cervical ripening [11]. It has been demonstrated that estrogens stimulate collagen degradation invitro, an effect that is blocked by progesterone [11]. Women with placental sulphatase deficiency have low levels of estrogen and do not undergo cervical ripening at term [10]. It is recognized that both oral contraceptive pills and pregnancy are associated with cervical eversion whereby columnar epithelium becomes visible on ectocervix [12,13].
A figure showing partial visualization of transformation zone on colposcopy.
Complete visualization of transformation zone after administrating medication.
Another important observation in our study was that the response to the drug varied with the site of non-visualization of transformation zone colposcopy. In Group I, patients with invisibility of transformation zone on posterior lip responded to a greater extent as compared to those with invisibility of transformation zone on anterior lip. Whereas, in Group II, subjects with involvement of anterior lip responded better as compared to those with involvement on posterior lip [Table/Fig-3]. This observation is along the similar lines in a different study by us [4] in which 65% of the patients with non- visualized posterior lip responded to 200μg of misoprostol as compared to 94% of the patients with involvement of anterior lip (p-value=0.05). In the same study, 81% of patients treated with 50μg of vaginal estradiol (for 7 days) with non-visualized anterior lip responded as compared to 84% patients with involvement on posterior lip(p=0.5). The reason for the difference in response of the anterior and posterior lips of the cervix to estrogens is unknown. Major adverse effects of the estrogen therapy were nausea and vaginal discharge, however, the difference was statistically non-significant [Table/Fig-2]. Response was comparable in premenopausal and postmenopausal women with the 2 drug regimens. Thus, menopausal status did not have any effect on response to the treatment.
Limitation
The present study could not be blinded and sample size was relatively small despite being statistically sufficient. More randomized trials with larger sample size are needed to confirm the findings.
Conclusion
In conclusion, both vaginal and oral estradiol have comparable efficacy in overcoming the partial or non-visualization of transformation zone on colposcopy with similar incidence of adverse effects.