Introduction
Poor survival rates after cardiac arrest can partly be explained by poor basic life support skills in medical professionals.
Aim
This study aimed to assess quality of basic life support in medical students and paramedics.
Materials and Methods
We conducted a prospective observational study with 100 early medical students (group A), 100 late medical students (group B) and 100 paramedics (group C), performing a 20-minute basic life support simulation in teams of two. Average frequency and absolute number of chest compressions per minute (mean (±SD)), chest decompression (millimetres of compression remaining, mean (±SD)), hands-off-time (seconds/minute, mean (±SD)), frequency of switching positions between ventilation and chest compression (per 20 minutes) and rate of sufficient compressions (depth ≥50mm) were assessed as quality parameters of CPR.
Results
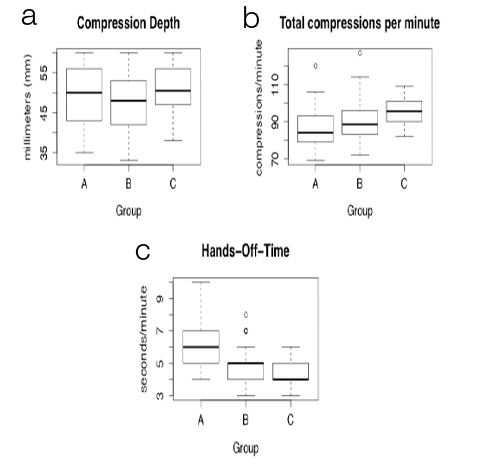
In groups A, B and C the rates of sufficiently deep chest compressions were 56%, 42% and 52%, respectively, without significant differences. Male gender and real-life CPR experience were significantly associated with deeper chest compression. Frequency and number of chest compressions were within recommended goals in at least 96% of all groups. Remaining chest compressions were 6 mm (±2), 6 mm (±2) and 5 mm (±2) with a significant difference between group A and C (p=0.017). Hands-off times were 6s/min (±1), 5s/min (±1) and 4s/min (±1), which was significantly different across all three groups.
Conclusion
Overall, paramedics tended to show better quality of CPR compared to medical students. Though, chest compression depth as an important quality characteristic of CPR was insufficient in almost 50% of participants, even in well trained paramedics. Therefore, we suggest that an effort should be made to find better ways to educate health care professionals in BLS.
Introduction
The annual incidence of out of hospital cardiac arrests treated by the emergency medical services is 38 per 100,000 population and the proportion that receive bystander cardiopulmonary resuscitation (CPR) is typically low [1,2]. Early recognition and immediate bystander CPR are critical determinates for survival after out-of-hospital cardiac arrest and high quality Basic Life Support (BLS) is the cornerstone for survival in patients with cardiovascular arrest [3]. Unfortunately, outcome of patients who suffer from a cardiac arrest out of hospital is still poor [4] and even quality of in-hospital CPR provided by medical professionals is often insufficient and thus associated with worse patient outcome [5–7]. Accordingly, existing data show that knowledge and retention of BLS skills is poor among paramedics as well as medical students [8–10] and a large part of residents entering work life have never performed BLS procedures beforehand [11–13]. This underlines the importance of education in BLS and regular assessment of skills. With this study we evaluated: (1) the quality of BLS given by medical students at the University of Cologne as well as paramedics; and (2) possible differences between early medical students, late medical students and paramedics.
Materials and Methods
Study cohort
We conducted a prospective observational study with 300 participants. Group A consisted of 100 early medical students (preclinical curriculum, between semester one and four), group B consisted of 100 late medical students (clinical curriculum, between semester five and ten) and group C consisted of 100 paramedics. The curriculum of the Medical School of the University of Cologne defines resuscitation courses in semester three, seven and nine. So most participants of group A had already obtained at least one BLS course and all participants of group B had at least one BLS, as well as an Advanced Life Support (ALS) course. Group A and B had overall obtained nine hours and 35 hours of resuscitation training, respectively. Participating paramedics were working in Cologne and had all obtained a BLS course in the past including at least four hours of training. All paramedics were currently taking or had already taken an BLS training program, consisting of approximately three more hours. How far they were advanced in their training program and their amount of professional experience were not recorded. All of participants participated voluntarily. The study was approved by the local ethics committee of the medical University of Cologne (15-225). Participants were assigned to teams of two persons and asked to perform a BLS stimulation.
Basic Life Support Simulation
The study took place between April 2013 and August 2014. Medical students were observed at the Cologne Inter-Professional Skills Lab and Simulation Center (KISS) of the medical University of Cologne. Paramedics were observed in the “Medakademie” school in Cologne. Each group undertook a 20-minute BLS simulation using an advanced patient simulator (Resusci-Anne®, Laerdal Medical, Stavanger, Norway). The BLS simulation was composed of chest compressions and mask ventilation for an asystole patient. Chest compressions were performed while kneeling beside the CPR dummy. The simulation was preceded by a standardised invitation to perform BLS including mask ventilation for as long as 20 minutes without further specifications. Besides, students of group A were further introduced into mask ventilation and given the opportunity to practise before the simulation since they were not experienced in this topic.
Objectives and Outcome Measures
Data were collected using Laerdal PC Skill Reporter (ResusciAnne® Laerdal Medical, Stavanger, Norway). Mean chest compression frequency, compressions per minute (absolute count of compressions per minute), chest decompression (millimeters of compression remaining), hands-off-time (seconds per minute), how often the participants switch positions (per 20 minutes) and compression depth (in millimeters) were recorded by the manikin.
Recorded Covariables
Demographics recorded were age, sex, semester, CPR training beforehand (yes/no), real-life CPR experience (yes/no) and professional health care experience (paramedic). If at least one person of a team had professional experience (paramedic), the team was ranked as “with professional experience”.
Statistical Analysis
All data was evaluated team-wise (150 teams á 2 participants). Group characteristics were described using frequencies (percentage) or mean ± standard deviation (SD), as appropriate. Differences between two groups were evaluated with unpaired t-test for quantitative data and Chi-square test for qualitative data. All reported p-values are two-sided and considered statistically significant if lower or equal 0.05. Because of the explorative setting the significance level is not adjusted for multiple testing. Calculations were done with SPSS Statistics, Version 22.0 (IBM Corp., Armonk, NY, USA).
Results
A total of 300 people participated, no missings were registered, all data could be analysed. Demographic data are shown in [Table/Fig-1]. The mean age of participants was 24 years (group A), 26 years (group B) and 23 years (group C). Group B showed significantly more female participants compared to group C. In groups A and B significantly less participants had performed real-life CPR beforehand compared to group C. Total 88% of participants in group A and 96% of participants of group B have obtained resuscitation training at least within the last two months. Most importantly, group A showed a significantly higher amount of teams, which did not receive prior BLS training nor had prior BLS experience compared to the other groups. To balance this baseline difference and make groups comparable in this regard, for further analyses of outcome measures we excluded all teams (n=11) from group A, which haven’t had any prior BLS training. A summary of parameters surveyed is shown in [Table/Fig-2]. Regarding chest compression depth in millimetres group A and C produced only an average of 56% and 52% sufficient chest compressions (≥ 50 mm deep), respectively. For group B chest compressions were sufficient in only 42%. Compression depth was highest in group C with an average of 51 mm depth, showing a statistically significant difference in comparison to group B (p=0.010) [Table/Fig-3a]. Group B showed the lowest compression depth. Regarding compressions per minute group A performed significantly fewer compressions compared to group B and C (p=0.002 and p<0.001, respectively). Group C performed the most compressions per minute with a mean count of 95.4 compressions per minute [Table/Fig-3b]. Regarding compression frequency group C reached the highest number of 121.3 with a statistically significant difference between group A and C [Table/Fig-2]. Regarding hands-off-time group A showed significantly longer hands-off-time compared to group C and group B [Table/Fig-3c]. Group C managed an averaged hands-off-time of only 4.3 seconds per minute. Regarding position-switch per 20 minutes group B switched significantly more often than group A and C. Regarding remaining chest compression only group C provided a mean remaining compression of almost 5 mm, showing a statistically significant difference compared to group A (p=0.018). Regarding tidal volume group A produced a mean volume of 434.5 ml per ventilation, group C a significantly higher volume of 545.9 ml per ventilation (p<0.001). Group B lay in between with a mean tidal volume of 498.3 ml.
Demographics (shown as mean ± SD or n (%)), evaluated team-wise.
| Parameters | Group A (preclinic teams) | Group B (clinic teams) | Group C (paramedic teams) | p-values |
|---|
| n = 50 | n = 50 | n = 50 | A vs B | B vs C | A vs C |
|---|
| Age in years (mean ± SD) | 24±3 | 26±3 | 23±5 | < 0.001 | < 0.001 | 0.304 |
| Female teams (à 2 participants) | 14 (28%) | 25 (50%) | 12 (24%) | 0.076 | 0.003 | 0.102 |
| Male teams (à 2 participants) | 17 (34%) | 11 (22%) | 27 (54%) |
| Mixed teams (1 male, 1 female) | 19 (38%) | 14 (28%) | 11 (22%) |
| Professional experience | 23 (46%) | 17 (34%) | 50 (100%) | 0,485 | < 0,001 | < 0,001 |
| CPR – training beforehand | 39 (78%) | 50 (100%) | 50 (100%) | < 0.001 | - * | < 0.001 |
| Real-life CPR experience | 18 (36%) | 7 (14%) | 45 (90%) | 0.004 | < 0.001 | < 0.001 |
Legend: * no p-value calculated
Summary of measured endpoints (shown as mean ± SD or n (%).
| Group A (preclinic teams) | Group B (clinic teams) | Group C (paramedic teams) | p-values |
|---|
| n = 39 | n = 50 | n = 50 | A vs B | B vs C | A vs C |
|---|
| Total number of compressions /min | 83.4±7.9 (100%)# | 90.1±10.8 (100%)# | 95.4±7.1 (100%)# | 0.002 | 0.005 | <0.001 |
| Compression frequency /min | 116.2±9.4 (95%)* | 118.9±12.5 (96%)* | 121.3±9.7 (100%)* | 0.259 | 0.295 | 0.014 |
| Compression depth [mm] | 50.0±7.7 | 47.3±7.2 | 50.7±5.6 | 0.092 | 0.01 | 0.611 |
| Chest compressions ≥ 50 mm | 22 (56%) | 21 (42%) | 26 (52%) | 0.177 | 0.316 | 0.679 |
| Remaining chest compression [mm] | 6.3±2.3 (41%)^ | 5.9±1.8 (36%)^ | 5.2±2.1 (56%)^ | 0.326 | 0.083 | 0.017 |
| Hands-off-time [s/min] | 6.4±1.5 | 4.9±1.1 | 4.3±0.7 | < 0.001 | 0.001 | < 0.001 |
| Tidalvolume [ml] | 434.5±138.5 | 498.3±145.7 | 545.9±134.7 | 0.039 | 0.093 | < 0.001 |
| Participants switch (per 20 minutes) | 8.0±2.5 (31%)° | 9.8±1.6 (60%)° | 9.0±2.1 (38%)° | < 0.001 | 0.041 | 0.047 |
Footnote: To balance the baseline difference regarding prior BLS training teams without prior BLS training were excluded (n=11) from group A, # percentage of teams with average total number of compressions per minute ≥ 60, * percentage of teams with average compression frequency per minute ≥ 100, ° percentage of teams with average participants switch of ≥ 10 per 20 minutes, ^ percentage of teams with average remaining compression depth ≤ 5mm.
Box plots of mean (a) compression depth (significant difference between group C and group B (p=0.010)), (b) total number of compressions per minute, where group A showed significantly less compressions compared to group B and C (p=0.002 and <0.001, respectively), (c) hands-off-time, where group C showed the lowest hands-off-time compared to group A and B (significant difference between group A and B (p<0.001), group B and C (p=0.001) and group A and C (p<0.001) compared between groups.
Since chest compression depth presented insufficient in large subsets of each group determinants of compression depth were further analysed. Significantly deeper chest compressions overall were associated with real-life CPR experience and male gender [Table/Fig-4]. Furthermore, teams with two paramedics (n=63) also showed significantly deeper chest compressions than teams with no professional experience (p=0.038).
Chest compression depth and association with covariables (results shown as mean ± SD).
| Gender Distribution | Female teams | Male teams | Mixed teams | p-values |
|---|
| n = 51 | n = 55 | n = 44 | female vs. male | female vs. mixed | male vs. mixed |
|---|
| Compression depth [mm] | 46.2±7.4 | 51.9±6.1 | 49.0±6.2 | < 0.001 | 0.049 | 0.022 |
| Real-life CPR experience | Real CPR teams | No real CPR teams | Mixed teams | p-values |
| n = 70 | n = 64 | n = 16 | real vs. no real | real vs. mixed | no real vs. mixed |
| Compression depth [mm] | 50.4±5.9 | 47.9±8.0 | 48.3±6.0 | 0.035 | 0.215 | 0.804 |
Discussion
A profound education in BLS is substantial for medical professionals, since patient outcome in case of cardiac arrest is critically dependant on quality of CPR. We performed this study to: (1) evaluate the quality of BLS given by medical students at the medical University of Cologne as well as paramedics; and (2) evaluate possible differences in quality between early medical students, late medical students and paramedics.
Importantly, we were able to show that essential quality parameters of BLS skills like depth of provided chest compressions were insufficient in large subsets of each cohort (in medical students as well as paramedics). To the best of our knowledge, this is the first study to describe BLS skills of 100 paramedics in comparison to medical students and we were able to show specific differences between groups that are likely related to training, experience and demographic factors.
ESC guidelines of 2010 and 2015 suggest that ideally chest compressions should be at least 50 mm deep and executed at a rate of at least 100 compressions per minute. Interruptions should be minimised and rescuers should change positions every two minutes to avoid fatigue. Furthermore the chest should be decompressed completely after compression. The 2010 ESC guidelines specify further that a patient should receive at least 60 compressions per minute [14,15]. Compression rates between 100 and 120 per minute [16] as well as minimised interruption in cardiac resuscitation [17,18] were recently also associated with best survival rates to hospital discharge in out-of-hospital cardiac arrest.
According to 2010 and 2015 guidelines, in our observation chest compression rate and absolute count of compressions per minute were sufficient. On the other hand, a mean remaining chest compression of 6 mm in our study could be optimised and chest compression depth was insufficient in all three groups, with only 56% and 52% of compressions ≥50 mm for group A and C, respectively and merely 42% ≥50 mm for group B. The latter is in line with previous studies that have suggested inadequate theoretical knowledge and skills of BLS in medical students [19,20]. As a possible explanation for poor performance it has been discussed that skills simply deteriorate after basic or advanced life support courses in as little as three to six months and regular refresher training could maintain better theoretical knowledge as well as practical skills [21–26]. In our observation on the other hand more than 80% of participants had received CPR training in the last two months and did not provide sufficient skills either, especially regarding chest compression depth. Furthermore the simulation for medical students took place at exam day, where they should have been prepared. The fact that our data show only an amount of 52% sufficient chest compressions in paramedics is alarming, since they count as well trained and experienced in basic life support skills. Therefore, we suggest that maybe training itself should be structured differently. In our case, we did not assess specific information about content or extent of previous training so no further conclusion can be drawn. Though, previous studies have suggested that CPR training should focus on real-life scenarios and practical experience for optimal outcome [27–29]. This as well is mentioned and emphasized in the 2015 ESC guidelines’ part on education [30]. Accordingly, we did find a positive association between real-life CPR experience and compression depth. Furthermore, teams comprised of two paramedics were superior with regards to compression depth compared with teams without any professional experience. These findings are as well in line with previous work that showed medical staff, frequently involved in resuscitation scenarios, superior in BLS knowledge compared with staff that have seldom or never performed CPR on patients [9]. Despite the distinct recommendation in 2010 and 2015 guidelines, the threshold of compression depth has also been discussed critically. Two previously published studies from Stiel and co-workers showed survival after out-of-hospital cardiac arrest best in patients that received chest compressions between 38-51 mm deep or 40.2-55.3 mm respectively [31,32].
As stated above we wanted not only to assess different quality parameters, but also compare them between groups. We did find significant differences with regard to chest compression depth, count of chest compressions per minute, tidal volume, hands-off-time, remaining chest compression and switch of participants per 20 minutes.
Group A performed significantly worse than the other groups with regards to hands-off time. It seems that switching positions and starting compressions again took longer in this group. This could be due to lack of experience. Group B and C performed better in this regard. This might be associated with higher numbers of previous training courses and real-life-experience. Furthermore, group A showed significantly lower tidal volumes per ventilation than group C, despite the possibility to practice mask ventilation before the simulation. It seems that practising mask ventilation for a few minutes does not provide enough experience to perform it sufficiently on a patient. Regarding chest compression depth on the other hand group A performed similarly to group C, suggesting that compression depth is not strictly dependent on experience of the rescuer. These two groups had similar gender distributions. Despite their humble amount of resuscitation training (nine vs. 35 hours) in comparison to group B, group A provided better results with regards to compression depth, though statistically not significant (p=0.092) and similar results with regards to compressions per minute, remaining chest compression and tidal volume.
Group B was only able to produce 42% of sufficient chest compressions (≥50 mm deep) altogether and performed significantly worse with regards to compression depth in millimetres compared to group C. Interestingly, group B also presented a significantly higher count of female participants. When analysed further, we saw an association between female gender and lower compression depth. This is in line with previously published data, that found not only male gender but also physical fitness associated with deeper chest compressions [33,34]. Group B also switched positions significantly more often than group A. This could be due to earlier physical exhaustion in female participants. In this context, it has been suggested previously that a rotation of rescuers every minute could provide more sufficient chest compressions [35] and most recently that the use of the dominant hand during chest compressions could also provide better results [36]. It may be of use pointing these two variations out to female participants in life support training. Further research should be obtained to evaluate and compare education strategies in terms of objective outcomes, focusing on helping female rescuers to improve their skills.
Group C performed best in comparison to the other groups with regards to compressions per minute, hands-off time, remaining chest compressions and tidal volume per ventilation. This may be due to a higher amount of hands-on-experience and could support stated-above theory that education should focus on real-life scenarios to gain more routine and provide better outcomes. Nevertheless, as mentioned above, even paramedics provided insufficient chest compressions in 48%, a fact that should be addressed in future research to find ways to further improve BLS quality in this important group.
Limitation
There are some limitations to our study. It was a single-centre study including only medical students of the University of Cologne and one paramedic school. A multi-centre observational study of several medical schools would be useful to get a better overview of BLS quality of medical professionals and students. Additionally, this would allow for a comparison between different countries, Universities and different education systems and curricula. We did not assess specific information about content of resuscitation training and the amount of professional experience in paramedics was not recorded. The possibility of drawing conclusions on possible influences of these parameters on performance is therefore limited but would definitely be of interest. Another limitation is of course, that participants knew that this was only a simulation not an exam or real-life situation. So we don’t know how it translates to real-life CPR and further studies focusing on this question would be of interest. Regarding the comparison of groups, one has to say that naturally groups A, B and C were not easily comparable due to their diversity. Paramedics are well trained healthcare professionals and therefore familiar with basic life support in their daily life. Nevertheless, since there are no data comparing BLS quality of medical students and paramedics in this manner yet, we think this comparison is valuable.
Conclusion
We conducted a CPR-training study to assess and compare BLS skills in medical students as well as paramedics. To our knowledge, there exists no data comparing practical skills between these two groups yet. Paramedics were superior with regards to hands-off time, whereas with regards to compression rates and compression depth we did not find a significant difference between them and early medical students. Overall, chest compression depth was insufficient (<50 mm depth) in large subsets of groups and was positively associated with male gender and real-life CPR experience. Most importantly, we could show that even in paramedics important parameters of basic life support were insufficient to a large amount. This provides evidence that further effort will be necessary to find an optimal way of educating our doctors-to-be and maybe especially paramedics to improve quality of BLS skills.
Competing Interests
The authors declare that they have no competing interests. This manuscript including its data, figures and tables does not overlap with previous publications, has not been published previously and is not under consideration elsewhere.
Legend: * no p-value calculated
Footnote: To balance the baseline difference regarding prior BLS training teams without prior BLS training were excluded (n=11) from group A, # percentage of teams with average total number of compressions per minute ≥ 60, * percentage of teams with average compression frequency per minute ≥ 100, ° percentage of teams with average participants switch of ≥ 10 per 20 minutes, ^ percentage of teams with average remaining compression depth ≤ 5mm.
[1]. Atwood C, Eisenberg MS, Herlitz J, Rea TD, Incidence of EMS-treated out-of-hospital cardiac arrest in EuropeResuscitation 2005 67(1):75-80. [Google Scholar]
[2]. Grasner JT, Herlitz J, Koster RW, Rosell-Ortiz F, Stamatakis L, Bossaert L, Quality management in resuscitation–towards a European cardiac arrest registry (EuReCa)Resuscitation 2011 82(8):989-94. [Google Scholar]
[3]. Sasson C, Rogers MAM, Dahl J, Kellermann AL, Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysisCirc Cardiovasc Qual Outcomes 2010 3(1):63-81. [Google Scholar]
[4]. Wik L, Kramer-Johansen J, Myklebust H, Sørebø H, Svensson L, Fellows B, Quality of cardiopulmonary resuscitation during out-of-hospital cardiac arrestJAMA 2005 293(3):299-304. [Google Scholar]
[5]. Abella BS, Alvarado JP, Myklebust H, Edelson DP, Barry A, O’Hearn N, Quality of cardiopulmonary resuscitation during in-hospital cardiac arrestJAMA 2005 293(3):305-10. [Google Scholar]
[6]. Abella BS, Sandbo N, Vassilatos P, Alvarado JP, O’Hearn N, Wigder HN, Chest compression rates during cardiopulmonary resuscitation are suboptimal: a prospective study during in-hospital cardiac arrestCirculation 2005 111(4):428-34. [Google Scholar]
[7]. Thorén AB, Axelsson A, Holmberg S, Herlitz J, Measurement of skills in cardiopulmonary resuscitation–do professionals follow given guidelines?Eur J Emerg Med 2001 8(3):169-76. [Google Scholar]
[8]. Zaheer H, Haque Z, Awareness about BLS (CPR) among medical students: status and requirementsJ Pak Med Assoc 2009 59(1):57-59. [Google Scholar]
[9]. Roshana S, Batajoo Kh, Piryani Rm, Sharma Mw, Basic life support: knowledge and attitude of medical/paramedical professionalsWorld J Emerg Med 2012 3(2):141-45. [Google Scholar]
[10]. Chamberlain DA, Hazinski MF, Education in resuscitationResuscitation 2003 59(1):11-43. [Google Scholar]
[11]. Promes SB, Chudgar SM, Grochowski CO, Shayne P, Isenhour J, Glickman SW, Gaps in procedural experience and competency in medical school graduatesAcad Emerg Med 2009 16(Suppl 2):S58-62. [Google Scholar]
[12]. Wu EH, Elnicki DM, Alper EJ, Bost JE, Corbett EC Jr, Fagan MJ, Procedural and interpretive skills of medical students: experiences and attitudes of fourth-year studentsAcad Med 2008 83(10 Suppl):S63-67. [Google Scholar]
[13]. Wu EH, Elnicki DM, Alper EJ, Bost JE, Corbett EC Jr, Fagan MJ, Procedural and interpretive skills of medical students: experiences and attitudes of third-year studentsAcad Med 2006 81(10 Suppl):S48-51. [Google Scholar]
[14]. Monsieurs KG, Nolan JP, Bossaert LL, Greif R, Maconochie IK, Nikolaou NI, European Resuscitation Council Guidelines for Resuscitation 2015Resuscitation 2015 95:1-80. [Google Scholar]
[15]. Nolan JP1, Soar J, Zideman DA, Biarent D, Bossaert LL, Deakin C, European Resuscitation Council Guidelines for Resuscitation 2010 Section 1. Executive summaryResuscitation 2010 81(10):1219-76. [Google Scholar]
[16]. Idris AH, Guffey D, Pepe PE, Brown SP, Brooks SC, Callaway CW, Chest compression rates and survival following out-of-hospital cardiac arrestCrit Care Med 2015 43(4):840-48. [Google Scholar]
[17]. Bobrow BJ, Clark LL, Ewy GA, Chikani V, Sanders AB, Berg RA, Minimally interrupted cardiac resuscitation by emergency medical services for out-of-hospital cardiac arrestJAMA 2008 299(10):1158-65. [Google Scholar]
[18]. Brouwer TF, Walker RG, Chapman FW, Koster RW, Association between chest compression interruptions and clinical outcomes of ventricular fibrillation out-of-hospital cardiac arrestClinical Perspective. Circulation 2015 132(11):1030-37. [Google Scholar]
[19]. Grześkowiak M, The effects of teaching basic cardiopulmonary resuscitation–a comparison between first and sixth year medical studentsResuscitation 2006 68(3):391-97. [Google Scholar]
[20]. Suzuki A, Suzuki Y, Takahata O, Fujimoto K, Nagashima K, Mamiya K, A survey of 3,303 6th-year medical students from 36 universities concerning knowledge of resuscitation–more than 80% of medical students can not perform standard cardiopulmonary resuscitation?Masui 2001 50(3):316-22. [Google Scholar]
[21]. Pande S, Pande S, Parate V, Pande S, Sukhsohale N, Evaluation of retention of knowledge and skills imparted to first-year medical students through basic life support trainingAdv Physiol Educ 2014 38(1):42-45. [Google Scholar]
[22]. Smith KK, Gilcreast D, Pierce K, Evaluation of staff’s retention of ACLS and BLS skillsResuscitation 2008 78(1):59-65. [Google Scholar]
[23]. Woollard M, Whitfeild R, Smith A, Colquhoun M, Newcombe RG, Vetteer N, Skill acquisition and retention in automated external defibrillator (AED) use and CPR by lay responders: a prospective studyResuscitation 2004 60(1):17-28. [Google Scholar]
[24]. Berden HJ, Willems FF, Hendrick JM, Pijls NH, Knape JT, How frequently should basic cardiopulmonary resuscitation training be repeated to maintain adequate skills?BMJ 1993 306(6892):1576-77. [Google Scholar]
[25]. Woollard M, Whitfield R, Newcombe RG, Colquhoun M, Vetter N, Chamberlain D, Optimal refresher training intervals for AED and CPR skills: a randomised controlled trialResuscitation 2006 71(2):237-47. [Google Scholar]
[26]. Mpotos N, De Wever B, Cleymans N, Raemaekers J, Valcke M, Monsieurs KG, Efficiency of short individualised CPR self-learning sessions with automated assessment and feedbackResuscitation 2013 84(9):1267-73. [Google Scholar]
[27]. Reznek MA, Rawn CL, Krummel TM, Evaluation of the educational effectiveness of a virtual reality intravenous insertion simulatorAcad Emerg Med 2002 9(11):1319-25. [Google Scholar]
[28]. Schaefer JJ, Grenvik A, Simulation-based training at the University of PittsburghAnn Acad Med Singapore 2001 30(3):274-80. [Google Scholar]
[29]. Devitt JH, Kurrek MM, Cohen MM, Cleave-Hogg D, The validity of performance assessments using simulationAnesthesiology 2001 95(1):36-42. [Google Scholar]
[30]. Bhanji F, Donoghue AJ, Wolff MS, Flores GE, Halamek LP, Berman JM, Part 14: EducationCirculation 2015 132(18 suppl 2):S561-S573. [Google Scholar]
[31]. Stiell IG, Brown SP, Christenson J, Cheskes S, Nichol G, Powell J, What is the role of chest compression depth during out-of-hospital cardiac arrest resuscitation?Crit Care Med 2012 40(4):1192-98. [Google Scholar]
[32]. Stiell IG, Brown SP, Nichol G, Cheskes S, Vaillancourt C, Callaway CW, What is the optimal chest compression depth during out-of-hospital cardiac arrest resuscitation of adult patients?Circulation 2014 130(22):1962-70. [Google Scholar]
[33]. Russo SG, Neumann P, Reinhardt S, Timmermann A, Niklas A, Quintel M, Impact of physical fitness and biometric data on the quality of external chest compression: a randomised, crossover trialBMC Emerg Med 2011 11:20 [Google Scholar]
[34]. Sayee N, McCluskey D, Factors influencing performance of cardiopulmonary resuscitation (CPR) by Foundation Year 1 hospital doctorsUlster Med J 2012 81(1):14-18. [Google Scholar]
[35]. Hasegawa T, Daikoku R, Saito S, Saito Y, Relationship between weight of rescuer and quality of chest compression during cardiopulmonary resuscitationJ Physiol Anthropol 2014 33:16 [Google Scholar]
[36]. Wang J, Tang C, Zhang L, Gong Y, Yin C, Li Y, Compressing with dominant hand improves quality of manual chest compressions for rescuers who performed suboptimal CPR in manikinsAm J Emerg Med 2015 33(7):931-36. [Google Scholar]