Cortical Clefts and Cortical Bumps: A Continuous Spectrum
Asthik Biswas1, Farha Furruqh2, Suresh Thirunavukarasu3, Ravichandran Vivekandan4
1 Senior Resident, Department of Radiology, St John’s Medical College Hospital, Bengaluru, Karnataka, India.
2 Senior Resident, Department of Radiology, St John’s Medical College Hospital, Bengaluru, Karnataka, India.
3 Specialist Grade II, Department of Neurology, Indira Gandhi Government General Hospital and Post Graduate Institute, Puducherry, India.
4 Specialist Grade I, Indira Gandhi Government General Hospital and Post Graduate Institute, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Asthik Biswas, 78-Omkar Nagar, Arekere Mico Layout, Bannerghatta Road, Bengaluru-560076, Karnataka, India.
E-mail: asthikbiswas@gmail.com
Cortical ‘clefts’ (schizencephaly) and cortical ‘bumps’ (polymicrogyria) are malformations arising due to defects in postmigrational development of neurons. They are frequently encountered together, with schizencephalic clefts being lined by polymicrogyria. We present the case of an eight-year-old boy who presented with seizures. Imaging revealed closed lip schizencephaly, polymicrogyria and a deep ‘incomplete’ cleft lined by polymicrogyria not communicating with the lateral ventricle. We speculate that hypoperfusion or ischaemic cortical injury during neuronal development may lead to a spectrum of malformations ranging from polymicrogyria to incomplete cortical clefts to schizencephaly.
Brain, Development, Malformation, Polymicrogyria, Schizencephaly
Case Report
An eight-year-old boy presented with history of seizures, generalised tonic clonic in nature, lasting for three minutes, with post-ictal loss of consciousness. There was no history of fever, headache or vomiting. He had a birth history of asphyxia with a consequent low APGAR score and required ventilatory support for one week. His past history and family history was otherwise unremarkable. General physical examination was normal. Higher mental functions for his age and cranial nerve examination were normal. Spino motor system sensory and cerebellar examination were within normal limits. There were no meningeal signs.
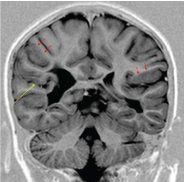
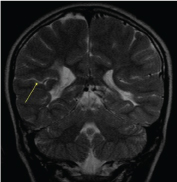
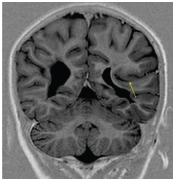
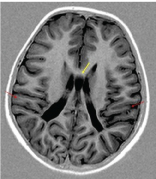
Blood glucose, serum electrolytes including calcium and magnesium were normal. An inter-ictal EEG was performed which was normal. MRI revealed a right sided CSF intensity cleft with apposed margins lined by grey matter which was communicating with the right lateral ventricle, suggestive of closed lip schizencephaly [Table/Fig-1,2]. A left sided cleft was noted which did not communicate with the lateral ventricle [Table/Fig-3]. The cleft was lined by polymicrogyria. Regions of polymicrogyria in bilateral temporoparietal cortex and an incidentally detected cavum septum pellucidum were also noted [Table/Fig-4].
Coronal T1 inversion recovery image showing a right sided cleft extending from the pial surface to the lateral ventricle with apposed margins (yellow arrow) suggestive of closed lip schizencephaly. Also, seen are regions of polymicrogyria (red arrows).
Coronal T2 weighted image showing the right sided CSF intensity cleft with apposed margins (yellow arrow).
Coronal T1 inversion recovery image showing a left sided deep cleft lined by polymicrogyria which is NOT communicating with the lateral ventricle (yellow arrow).
Axial T1 inversion recovery image showing cavum septum pellucidum (yellow arrow) and regions of polymicrogyria in bilateral temporo-parietal lobes (red arrows).
The patient was started on sodium valproate 200mg BD and showed good response. He is currently on daily antiepileptics for the last one year and has not had breakthrough seizures. He is doing well at school.
Discussion
Schizencephaly and polymicrogyria are developmental disorders which were classified as disorders of late neuronal migration and organization [1]. Advances in molecular biology, genetics and imaging have led to reclassification of the same under malformations secondary to post migrational development [2]. Since polymicrogyria lines schizencephalic clefts [3], it is reasonable to assume that a common aetiologic factor may predispose to these conditions. Varying severities of ischaemic insult, toxic and infectious causes have been proposed as the aetiologic factors by Barkovich an Kjos [4].
Schizencephaly consists of a cleft extending from the pial surface to the ventricle which is lined by grey matter. It was first described by Wadsworth and Yakolev in 1946 [5,6], Polymicrogyria consists of irregular gyri, regions of apparent thickened cortex and a stippled grey- white matter interface [7].
These malformations present with a wide spectrum of clinical manifestations, ranging from asymptomatic to epilepsy and developmental delay. This case illustrates features of both schizencephaly and polymicrogyria, and also an intermediate ‘incomplete cleft’ not fully satisfying the criteria for schizencephaly. We aimed to highlight that these malformations are part of a spectrum that arise due to varying severities of hypoxic insult.
Schizencephaly may be of the open or closed type. These are based on whether the cleft margins are separate or apposed [5,6]. It can be unilateral or bilateral, symmetric or asymmetric [4]. Association with optic nerve hypoplasia, pachygyria, polymicrogyria, heterotopia, and arachnoid cysts have been described [8].
Polymicrogyria is a malformation of cortical development consisting of excessive small gyri with narrow sulci and an irregular, ‘bumpy’ appearance of the cortical surface and grey-white matter junction [8]. It may be focal, multifocal or diffuse, unilateral or bilateral [9]. It most commonly occurs in the perisylvian regions [10], although involvement of most cortical regions have been described [9].
These malformations are now classified under malformations of post migrational development [2]. MRI is useful for diagnosing disorders of cortical development. Schizencephaly can be diagnosed upon identifying a CSF filled cleft lined by gray matter that extends from the pial surface to the ventricle [8]. Polymicrogyria is diagnosed by the presence of increased cortical thickness, an abnormal gyral pattern, and irregularity of the cortical-white matter junction [7].
Normal development of the nervous system begins with primary neurulation (at 3-4 weeks), followed by development of the prosencephalon (2-3 months), neuronal proliferation (3-4 months), neuronal migration (3-5 months), neuronal organization (5 months to after birth) and myelination (after birth) [3]. Neuronal migration begins in the eighth week of gestation with the neurons migrating radially outward from the germinal matrix in the walls of the lateral ventricles to form the cerebral cortex [11]. Interruption of the normal processes of development due to lack of normal gene expression, by either an abnormal gene or interference of normal gene function due to external causes such as infection or ischaemia can lead to schizencephaly and polymicrogyria [12].
Schizencepalic clefts are lined by polymicrogyria [3]. The theory supporting this association is that schizencephaly and polymicrogyria arise due to hypoperfusion or ischaemic cortical injury with mild ischaemic insult causing polymicrogyria without cortical infolding and more severe insults resulting in clefts lined by polymicrogyria [4,13]. Barkovich has postulated that cortical infolding of various depths lined by dysplastic cortex could indicate that schizencephaly and polymicrogyria share a common pathogenesis [4]. This theory explains our patients imaging findings with varying degrees of ischaemic insult occurring during development leading to schizencephaly, an incomplete cortical cleft and polymicrogyria. A similar imaging finding has been described by Leventer et al., as a ‘novel’ form of polymicrogyria. It consisted of a cleft lined by polymicrogyria directed towards the lateral ventricle but not communicating with it. The authors in the study postulated that such a cleft may be an incomplete form of schizencephaly and that a spectrum of clefting may exist ranging from schizencephaly to deep clefts lined by polymicrogyria but not communicating with the ventricles [9].
Conclusion
We thus highlight that schizencephaly and polymicrogyria are part of a continuum of disorders of cortical development at the post migrational level.
[1]. Barkovich AJ, Kuzniecky RI, Jackson GD, A developmental and genetic classification for malformations of cortical developmentNeurology 2005 65(12):1873-87. [Google Scholar]
[2]. Barkovich AJ, Guerrini Kuzniecky RI, A developmental and genetic classification for malformations of cortical development: update 2012Brain 2012 135(5):1348-69. [Google Scholar]
[3]. Argyropoulou MI, Rossi A, Gunny RS, Paediatric neuroradiology In: Adam A, Dixon AK, Gillard JH, Schaefer-Prokop CM, editorsPaediatric neuroradiology 2014 6th editionChurchill Livingstone:1992 [Google Scholar]
[4]. Barkovich AJ, Kjos BO, Schizencephaly: Correlation of clinical findings with MR characteristicsAJNR Am J Neuroradiol 1992 13:85-94. [Google Scholar]
[5]. Yakovlev PI, Wadsworth RC, Schizencephalies; a study of the congenital clefts in the cerebral mantle; clefts with fused lipsJ Neuropathol Exp Neurol 1946 5:116-30. [Google Scholar]
[6]. Yakovlev PI, Wadsworth RC, Schizencephalies; a study of the congenital clefts in the cerebral mantle; clefts with hydrocephalus and lips separatedJ Neuropathol Exp Neurol 1946 5:169-206. [Google Scholar]
[7]. Barkovich AJ, Hevner R, Guerrini R, Syndromes of bilateral symmetrical polymicrogyriaAJNR Am J Neuroradiol 1999 20:1814-21. [Google Scholar]
[8]. Razek AAKA, Kandell AY, Elsorogy LG, Disorders of cortical formation: MR imaging featuresAJNR Am J Neuroradiol 2009 30:4-11. [Google Scholar]
[9]. Leventer RJ, Jansen A, Pilz DT, Clinical and imaging heterogeneity of polymicrogyria: a study of 328 patientsBrain 2010 133:1415-27. [Google Scholar]
[10]. Leventer R (2007). Polymicrogyria and related disorders of cortical development: a clinical, imaging, and genetic study. In: Child Health Institute. Melbourne, Australia: University of Melbourne 411 [Google Scholar]
[11]. Rakic P, Neuronal migration and contact guidance in the primate telencephalonPostgraduate Medical Journal 1978 54:25-40. [Google Scholar]
[12]. Barkovich AJ, Congenital Malformations of the Brain and SkullBy A James Barkovich - Pediatric Neuroimaging 2006 4th editionPhiladelphiaLippincott Williams & Wilkins:322 [Google Scholar]
[13]. Barth PG, Disorders of neuronal migrationCan J Neurol Sci 1987 14(1):1-16. [Google Scholar]