Penile Sarcoma: Report of a Rare Malignancy
Shiv Rajan1, Vijay Kumar2, Arun Chaturvedi3, Jeevan Ram Vishnoi4, Prashant Dontula5
1 Senior Resident, Department of Surgical Oncology, King Georges Medical University, Lucknow, U.P, India.
2 Associate Professor, Department of Surgical Oncology, King Georges Medical University, Lucknow, U.P, India.
3 Professor and Head, Department of Surgical Oncology, King Georges Medical University, Lucknow, U.P, India.
4 Senior Resident, Department of Surgical Oncology, King Georges Medical University, Lucknow, U.P, India.
5 Senior Resident, Department of Surgical Oncology, King Georges Medical University, Lucknow, U.P, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shiv Rajan, Senior Resident, Department of Surgical Oncology, King Georges Medical University, Shatabdi Building, Lucknow, U.P-226003, India.
E-mail: sivrajan.194@gmail.com
Penile cancer is an uncommon malignancy. Squamous cell carcinoma constitutes approximately 95% of all histology. Non-squamous malignancies are rare in penis. Sarcomas of penis are rarer among them. Spindle cell sarcoma is one of the extremely rare sarcoma of penis. To best of our knowledge, only two cases have been reported so far, one in English literature and other in Japanese. We are presenting this uncommon case of spindle cell sarcoma of penis, which was diagnosed with microscopy with its characteristic immunohistochemistry. The disease had an aggressive course with multiple recurrences in a short duration despite margin negative resection. Disease responded poorly with the chemotherapy and patient succumbed to the disease.
Chemotherapy, Penile cancer, Spindle cell sarcoma
Case Report
A 65-year-old man presented with a recurrent growth over the penis. He was twice operated for the same elsewhere. Initially he underwent glansectomy and bilateral inguinal lymph node biopsy 7 months back. The histopathology report showed, 1.5×1.5cm tumour in glans at periuretheral area. On microscopic examination, malignant spindle cells with squamoid appearance arranged in fascicular pattern were described. Urothelium was ulcerated with underlying tumour and adjacent squamous epithelium showed severe dysplasia. Proximal margin was clear. Left inguinal node biopsy specimen showed only two lymph nodes, which were free from metastasis and no lymph node were identified on right side specimen.
Patient had local recurrence over distal penile stump 3 months after the first surgery. CT scan showed in homogeneous enhancing mass at penile stump with subcentimetric node bilateral inguinal area. He underwent partial penectomy. Histopathology showed 3.5×3×1.5cm tumour with involvement of skin, corpora cavenosa and spongiosa. Proximal margin and urethral margins were clear.
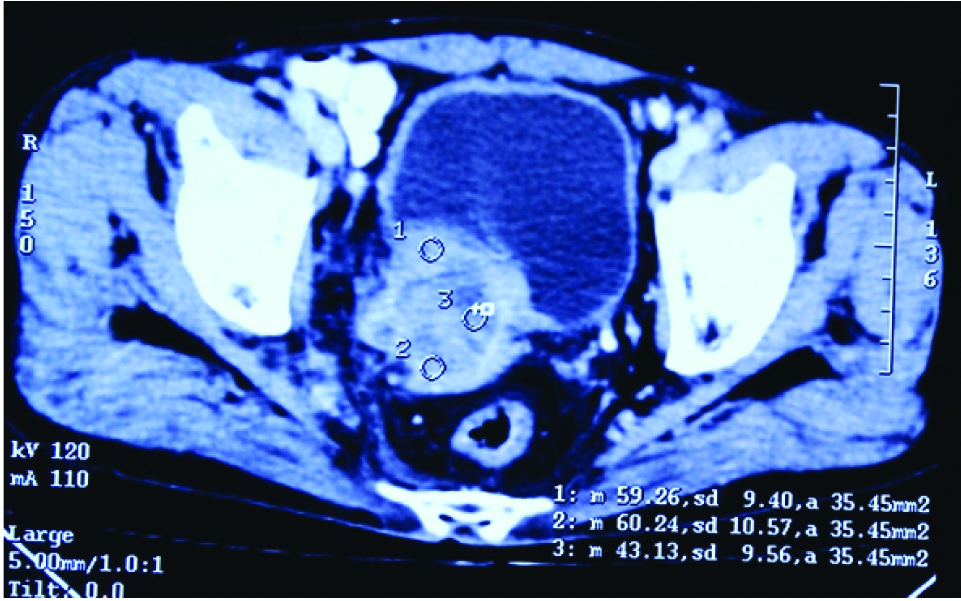
Patient again had second recurrence after 2 months and presented to our department this time. On examination, a fungating growth was present over the residual stump extending on to scrotal wall [Table/Fig-1]. Two, right inguinal nodes, firm, mobile, up to 1.5 cm were palpable. Biopsy of the lesion was taken at this time and subjected to both histopathology and immunohistochemistry. Histopathology showed malignant spindle cells arranged in fascicular pattern with similar description as in his first histopathology report [Table/Fig-2a,b]. Immunohistochemical examination was done which showed positivity for smooth muscle actin and desmin while caldesmon was negative [Table/Fig-3a-c]. Epithelial markers (panCK, EMA,CK8/18), vascular markers (CD34,CD31), and melanoma markers (S-100, HMB-45, Melan-A) were negative. Final diagnosis of low grade malignant spindle cell sarcoma of penis was made. CT scan showed 3×4×5 cm penile lesion with extension to scrotal wall. A separate inhomogeneous enhancing 6×5×6.5 cm retrovesical mass infiltrating posterior wall of urinary bladder, prostate and seminal vesicles with illdefined interface with right obturator internous muscle, levator ani and anterior rectal wall was identified [Table/Fig-4]. Other abdominal viscera and thorax showed no evidence of metastasis. So, patient was staged as recurrent stage III spindle sarcoma of penis.
Clinical picture showing a fungating growth present over the residual penile stump.

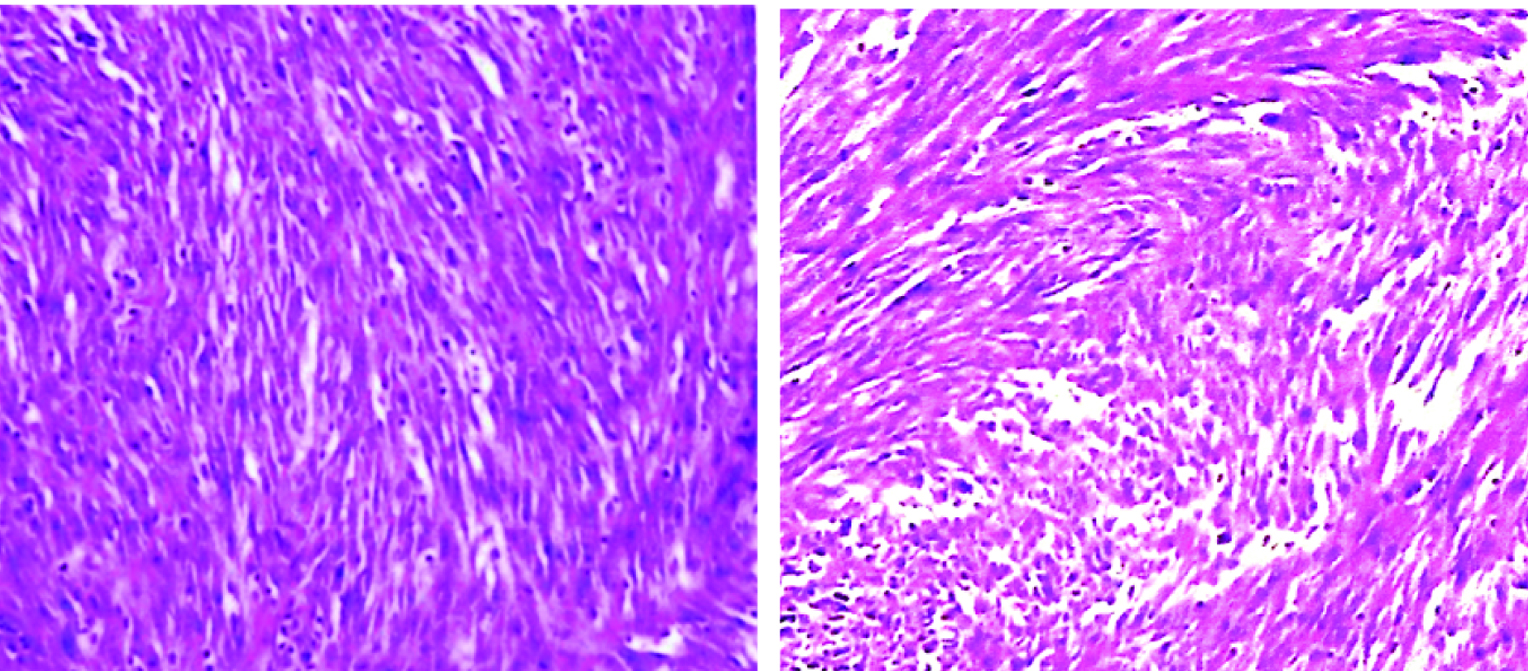
Microscopic picture showing malignant spindle cells with arranged in fascicular pattern. (2a: 40X and 2b: 20X magnification).
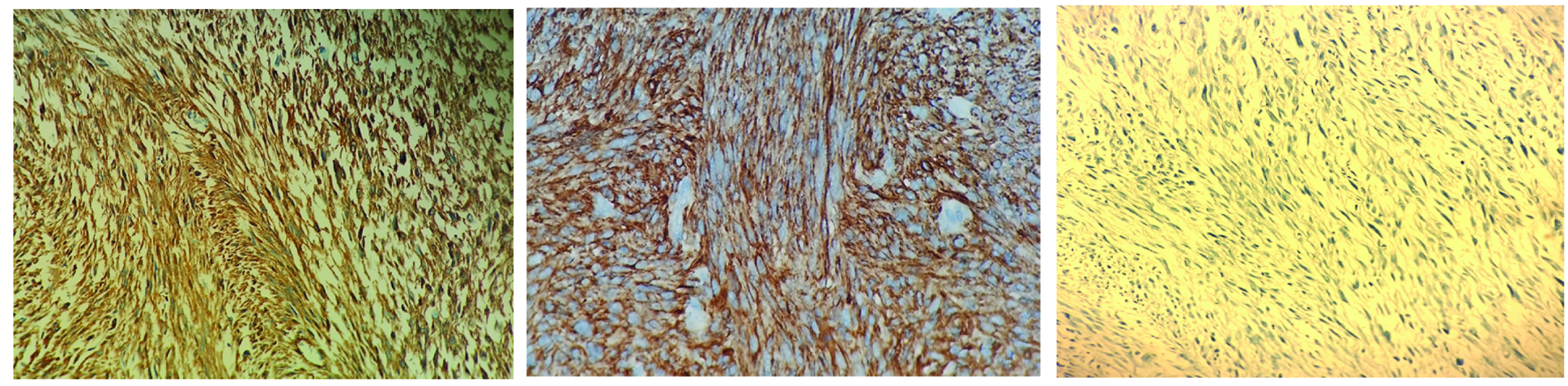
Imunnohistochemical examination showing positive staining of smooth muscle actin (3a) (20X) and desmin (3b) (40X), negative staining for caldesmon (3c) (20X).
CT scan showing retrovesical mass infiltrating posterior wall of urinary bladder, prostate and seminal vesicles.
Because of extensive unresectable nature of the disease, patient was planned for palliative chemotherapy. Ifosphamide and doxorubicin combination chemotherapy was started. Patient received 2 cycles of these at 3 weekly intervals but finally succumbed to the disease.
Discussion
Squamous cell carcinoma of penis is rare tumour with reported incidence up to 10% in developing countries of Asia, Africa, and South America [1]. Non-Squamous malignancies of penis, mesenchymal and lymphoid tumours, are even rarer. Mesenchymal tumours comprise less than 5% of all penile malignancies [2]. Soft tissue tumours of the penis comprise mainly of vascular sarcomas like Kaposi sarcoma, epithelioid hemangioendothelioma and angiosarcoma, followed by rhabdomyosarcoma and leiomyosarcoma [3]. Rare examples of additional sarcomas that have been reported include epithelioidsarcoma [4], osteosarcoma [5], ewing sarcoma [6] and clear cell sarcoma [7]. Spindle cell sarcoma of penis is extremely rare tumour of penis. After extensive search using terms penis or penile sarcoma, spindle cell sarcoma penis, primary penile sarcoma on pubmed and google scholar from 1970-2016, only two case reports of one patient each has been found. First case was reported in Japan at university of Tsukuba and second case was reported at Memorial Sloan-Kettering Cancer Center, New York, USA [8,9].
Spindle cell tumours have spindle shaped malignant cells arranged in different patterns with variable mitotic activity. IHC is excellent tool to differentiate the types of spindle cell tumours. Differential diagnosis of spindle cell neoplasm includes spindle cell melanoma (S-100 +), vascular spindle cell tumours, dermatofibrosarcoma protuberans and neural spindle cell tumours (all CD34 +), spindle cell tumours of smooth muscles (caldesmon +) and skeletal muscle (caldesmon), and spindle cell carcinoma (CK and EMA +). In our case IHC was positive for SMA & desmin only and negative for caldesmon, CD 34, CD31, CK, EMA, CK 8/18, S-100, HMB-45 & melan-A. Based on these finding definitive diagnosis of spindle cell sarcoma was made [10].
Given the relative rarity of spindle cell sarcoma no standardized treatment algorithm exists. In general, Non- squamous malignancies of the penis are primarily treated surgically, with the goal of complete excision at the time of treatment. The utilization of lymphadenectomy is less clear in these malignancies, but aggressive approaches should be considered in appropriate patients [9]. We are presenting this case of spindle cell sarcoma of penis, as it is exceedingly rare malignancy. There is little information available on the clinical and pathological aspect of this entity.
Conclusion
Immunohistochemistry should be used for correct pathological diagnosis of spindle cell sarcoma. As with squamous cell carcinoma of penis, surgery appears to be the curative treatment of resectable disease. Local recurrence at primary site despite clear margin implies importance of genetic changes that might be essential to tailor the surgical extent and utilization of chemotherapy, radiotherapy and targeted therapy for the treatment of this rare tumour.
[1]. Pow-Sang MR, Ferreira U, Pow-Sang JM, Nardi AC, Destefano V, Epidemiology and natural history of penile cancerUrology 2010 76(2):S2-6. [Google Scholar]
[2]. Lucia MS, Miller GJ, Histopathology of the malignant lesions of the PenisUrol Clin North Am 1992 19(2):227-46. [Google Scholar]
[3]. Dominici A, Rose AD, Stomaci N, Pugliese L, Posti A, Nesi G, A Rare case of Leiomyosarcoma of the penis with a reappraisal of the literatureInt J Urol 2004 11(6):440-44. [Google Scholar]
[4]. Colombo F, Franceschelli A, Schiavina R, Gentile G, Passaretti G, Martorana G, Epithelioid sarcoma of the penis: a case reportJ Sex Med 2013 10(11):2871-74. [Google Scholar]
[5]. Edwards AT, Somerville JJ, Primary osteosarcoma of penisBr J Urol 1990 66(5):552-53. [Google Scholar]
[6]. Ma Z, Brimo F, Zeizafoun N, Primary Ewing’s Sarcoma/Primitive Neuroectodermal Tumour (ES/PNET) of the penis: a report of an extraordinarily unusual site and a literature review of extraskeletal Ewing’s sarcomaInt J SurgPathol 2013 21(1):63-67. [Google Scholar]
[7]. Ito T, Melamed J, Perle MA, Alukal J, Clear cell sarcoma of the penis:a case reportAm J Clin Exp Urol 2015 3(1):43-47. [Google Scholar]
[8]. Kimura T, Oikawa T, Ikeda A, Yoshino T, Suetomi T, Miyazaki J, Spindle Cell Sarcoma of the Penis: A Case ReportHinyokika Kiyo 2012 58(6):299-305. [Google Scholar]
[9]. Moses KA, Sfakianos JP, Winer A, Bernstein M, Russo P, Dalbagni G, Non-squamous cell carcinoma of the penis: single-center, 15-year experienceWorld J Urol 2014 32(5):1347-53. [Google Scholar]
[10]. Rekhtman N, Bishop JA, Quick Reference Handbook for Surgical Pathologists 2011 HeidelbergSpringer [Google Scholar]