Paediatric Extracranial Spinal Accessory Nerve Schwannoma: An Extremely Rare Case Report
Arunabha Chakravarti1, Sunil Garg2, Rahul Bhargava3
1 Professor, Department of Otorhinolaryngology- Head & Neck Surgery, Lady Hardinge Medical College & Associated Hospitals, New Delhi, India.
2 Senior Resident, Department of Otorhinolaryngology- Head & Neck Surgery, Lady Hardinge Medical College & Associated Hospitals, New Delhi, India.
3 Junior Resident, Department of Otorhinolaryngology- Head & Neck Surgery, Lady Hardinge Medical College & Associated Hospitals, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sunil Garg, Department of Otorhinolaryngology- Head & Neck Surgery, Lady Hardinge Medical College & Associated Hospitals, Shahid Bhagat Singh Marg, New Delhi-110001, India.
E-mail: dr.sunilgarg09@gmail.com
Schwannoma in head and neck region are quiet common and generally arise from last four cranial nerves. Spinal accessory nerve involvement is very rare. We are hereby presenting an extremely rare case of paediatric XI nerve schwannoma hitherto unreported in English medical literature till date.
Children, Parapharyngeal space, Nerve tumor
Case Report
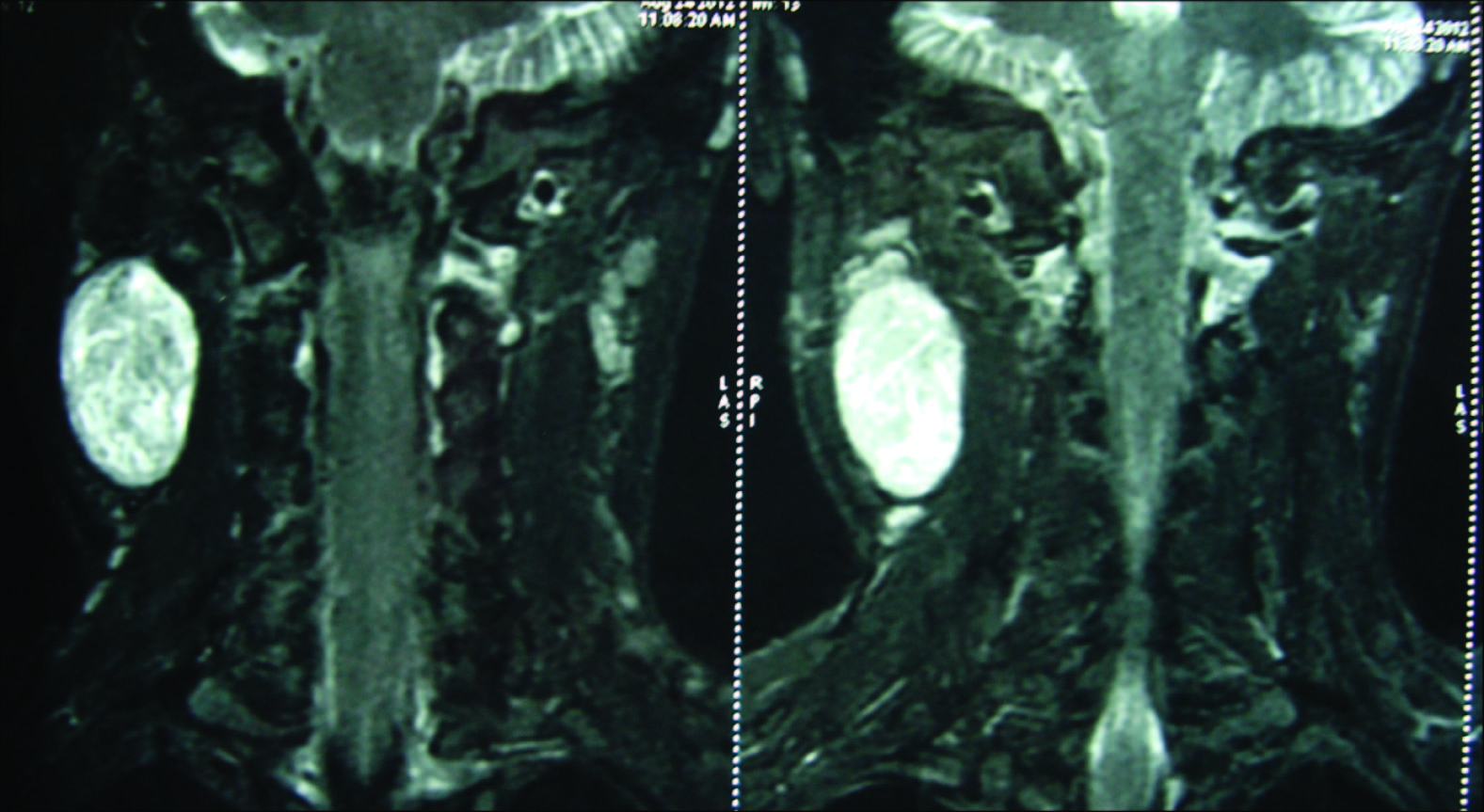
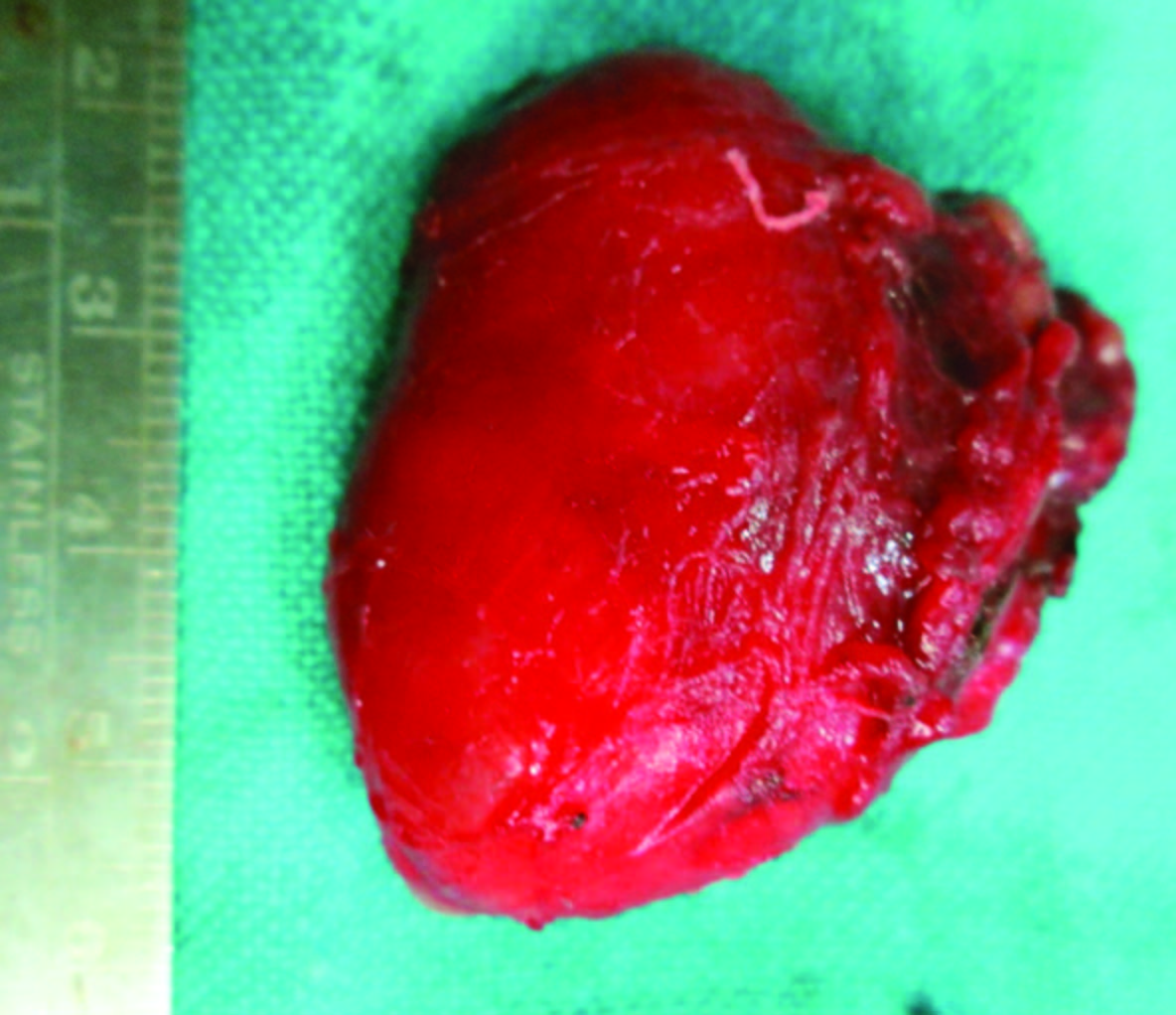
An 11-year-old boy presented with a mass on right side of neck for about 4 months, gradually increasing in size without any other associated symptom. On examination, it was 4x3cm in size, firm, non-tender, mobile from side to side, lying deep to upper 1/3rd of sternomastoid muscle. Oropharyngeal and indirect laryngoscopic examination did not show any abnormal finding. All cranial nerve and peripheral nerve examination was normal. CECT scan showed a biphasic enhancing mass of 4x3cm on the right side of neck deep to sternomastoid muscle and pushing internal jugular vein and common carotid artery anteromedially but did not suggest the nerve of origin [Table/Fig-1]. FNAC of the lesion did not reveal any definitive diagnosis. MRI of the lesion showed homogenous, isointense signal on T1 weighted images and on Gadolinium-enhanced T1 weighted images showed higher intensity [Table/Fig-2]. Excision was planned under general anaesthesia. The patient was explained about the possible complications of surgery preoperatively. The tumour was dissected free from surrounding structures and removed in toto [Table/Fig-3]. Despite the use of nerve monitor during surgery, the nerve of origin could not be clearly identified. Specimen was sent for histopathology which was suggestive of schwannoma. In the postoperative period patient developed weakness of trapezius and sternocleidomastoid muscle on the right side [Table/Fig-4]. On follow-up there was no recurrence and the patient’s weakness improved significantly with physiotherapy.
Axial CT XI Nerve Schwannoma.

Specimen XI nerve schwannoma.
Postoperative picture of patient.

Discussion
Neck masses are quite common among paediatric patients. These can be conveniently divided into lymphomatous and non-lymphomatous; and benign and malignant. Malignancy is an exception than rule in paediatric patients as far as neck masses are concerned. The most common benign neck mass among this age group is reactive lymphadenopathy. Among all benign non-lymphadenomatous neck masses, tumours of nerve origin are rare, presenting in 2% cases only [1].
Schwannomas rise from the Schwann cells of the peripheral nerve sheath [2]. These are generally solitary and slow growing, well-encapsulated tumours that occur in the head and neck region in 25-45% of the cases [3]. Among adults, schwannomas are the most common tumours of nerve origin in head and neck region [1]. But these tumours are extremely rare in children and can be missed by clinicians easily. The age of presentation of schwannomas is between 20 and 50 years. Only approximately 10% of schwannomas are diagnosed in patients below 21 years of age [4–6].
Extracranial head and neck schwannoma is a challenging condition to the head and neck surgeons. Diagnosis and treatment always pose great difficulty in treating these masses due to location of the tumour. It is difficult to diagnose these tumours by fine needle aspiration cytology because of inadequate and non-representative specimen obtained with it [7]. Specificity of FNAC has been found to be 20% only [8].
Ultrasonography is useful to rule out other neck swellings and also tells the relationship of the tumour to other structures but it is not sensitive enough to certainly diagnose schwannoma. It also tells us about relation of the tumour to the other neck structures. Identification of a nerve found directly entering and exiting a mass is pathognomic for a peripheral nerve sheath tumour but these findings are rarely encountered [9].
CECT is good tool to diagnose these tumours by using anatomical relationships of the tumour as well as physical characteristics of the nearby nerves. A dense central compartment with low area of enhancement at the periphery is seen on CECT of schwannoma. None of the features are pathognomic of schwannoma even on CECT scan [9]. MRI is quiet a useful imaging study for schwannoma of head and neck region, but it is not of much help for diagnosis of nerve of origin. Even the most reliable study done by Furukawa could not identify all schwannoma on imaging (except vagal and sympathetic chain) [10]. In a study by Hin-Lin Liu et al., the specificity of imaging studies in making the diagnosis of schwannoma was 38% [8]. The nerve of origin could be identified in 4% cases only. The diagnosis of schwannoma mainly relies on clinical suspicion; and confirmation is often obtained by means of surgical pathology.
Since schwannoma displace the nerve fibres as they grow, the postoperative neural function can be preserved by intracapsular dissection. But despite intracapsular dissection, nerve sacrifice is needed in 56% cases and of the remaining 44% of patients, 64% cases have permanent deficits and 29% have transient deficits [11].
Cervical schwannomas originate from spinal nerves, last four cranial nerves and occasionally from the sympathetic chain [12]. Patients with these tumours generally present between 20 and 50 year of age, they are extremely rare in children. There is paucity of published literature of extracranial head and neck XI nerve schwannoma in paediatric age group.
Schwannomas of spinal accessory nerve are quiet rare in occurrence. There are only three cases reported in the literature till date of intrasternomastoid type of spinal accessory nerve schwannoma which were found in adults [13]. No age predilection or sex preponderance can be documented due to few number of cases reported. In the case presented here, CT scan and MRI of the neck could not clearly demonstrate the diagnosis as well as nerve of origin. FNAC, done twice, was inconclusive. Nerve of origin was confirmed only after excision of the tumour when patient developed weakness of trapezius and sternocleidomastoid muscles during postoperative period.
Conclusion
We are presenting this case due to its rarity as well as its presentation in childhood being the first case to be reported in world medical literature. We recommend that schwannoma should also be included as a differential diagnosis in childhood neck masses. Pre-operative counselling of the patient regarding morbidity (postoperative) is essential in suspected cases of schwannoma and a written consent should always be taken prior to surgery.
Declaration of the conflicting interests
The authors declared no potential conflicts of interest with respect to and/or publication of the article.
Funding
Authors received no financial support for the research, authorship and/or publication of the article.
Ethical Approval
Consent was taken from parents of the children for surgery and publication of the case report.
[1]. Mackenzie K, Connolly AAP, Paediatric neck masses - a diagnostic dilemmaJournal of Laryngology and Otology 1997 111:541-45. [Google Scholar]
[2]. Kanatas A, Mucke T, Houghton D, Mitchell AD, Schwannomas of the head and neckOncol Rev 2009 3:107-11. [Google Scholar]
[3]. Colreavy MP, Lacy PD, Hughes J, Head and neck schwannomas: a 10 years reviewJ Layngol Otol 2000 114:119-24. [Google Scholar]
[4]. Gupta D, Benign solitary schwannomasCancer 1969 24:355-66. [Google Scholar]
[5]. Katz AD, Passy V, Kaplan N, Neurogenous neoplasms of the major nerves of head and neckArchives of Surgery 1971 103:51-56. [Google Scholar]
[6]. Al-Ghamdi S, Black MJ, Lafond G, Extracranial head and neck schwannomasThe Journal of Otolaryngology 1992 21(3):186-88. [Google Scholar]
[7]. Yu GH, Sack MJ, Baloch Z, Gupta PK, Difficulties in the fine needle aspiration (FNA) diagnosis of schwannomaCytopathology 1999 10:186-94. [Google Scholar]
[8]. Liu HL, Yu SY, Li GK, Wei WI, Extracranial head and neck schwannomas: a study of the nerve of originEur Arch Otorhinolaryngol 2011 268:1343-47. [Google Scholar]
[9]. Kami YN, imaging findings of neurogenic tumours in the head and neck regionDentomaxillofacial Radiology 2012 41:18-23. [Google Scholar]
[10]. Furukawa M, Furukawa MK, Katoh K, Tsukuda M, Differentiation between schwannoma of the vagus nerve and schwannoma of the cervical sympathetic chain by imaging diagnosisLaryngoscope 1996 106(12 Pt 1):1548-52. [Google Scholar]
[11]. Valentine J, Expected neurologic outcomes for surgical management of cervical neurilemomasLaryngoscope 1998 108:1009-13. [Google Scholar]
[12]. Cashman E, Skinner LJ, Timon C, Thyroid swelling: an unusual presentation of a cervical sympathetic chain schwannomaMedscape J Med 2008 10:201 [Google Scholar]
[13]. Agarwal A, Intrasternomastoid spinal accessory nerve schwannoma: clinical and radiological correlationNeurology India 2005 53(5):347-48. [Google Scholar]