Communicating (Open) Renal Hydatid Cyst Managed Successfully with Renal Sparing Approach
Priyank Yadav1, Alpana2, Vijay Sharma3, Devarshi Srivastava4, Hiralal5
1 Senior Resident, Department of Urology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Raebareli Road, Lucknow, Uttar Pradesh, India.
2 Junior Resident, Department of Radiology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Raebareli Road, Lucknow, Uttar Pradesh, India.
3 Senior Resident, Department of Urology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Raebareli Road, Lucknow, Uttar Pradesh, India.
4 Senior Resident, Department of Urology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Raebareli Road, Lucknow, Uttar Pradesh, India.
5 Additional Professor, Department of Radiology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Raebareli Road, Lucknow, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hiralal, Room No: 35, Department of Radiology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Raebareli Road, Lucknow-226014, Uttar Pradesh, India.
E-mail: hiralal2007@yahoo.co.in
Renal hydatid disease accounts for 2% of all cases of hydatid cysts. With the majority of isolated renal hydatid disease patients being asymptomatic, hydatid cysts grow slowly for several years. They may be associated with pressure symptoms or flank pain, depending on their size and location. Hydatiduria occurs in less than one-fifth of the patients. In the absence of hydatiduria, diagnosis is usually radiological. Surgery is the mainstay of treatment which is usually renal sparing surgery as most cysts are non-communicating. In cases of cyst communicating with the collecting system, nephrectomy remains the mainstay of treatment. We report a case of hydatiduria due to a communicating hydatid cyst diagnosed on CT urography, where a renal sparing approach was followed and the patient was managed with cystopericystectomy, closure of Pelvicalyceal System (PCS) and double J (DJ) stenting with an excellent result.
Chronic kidney disease, Cystopericystectomy, Hydatiduria, Renal sparing surgery
Case Report
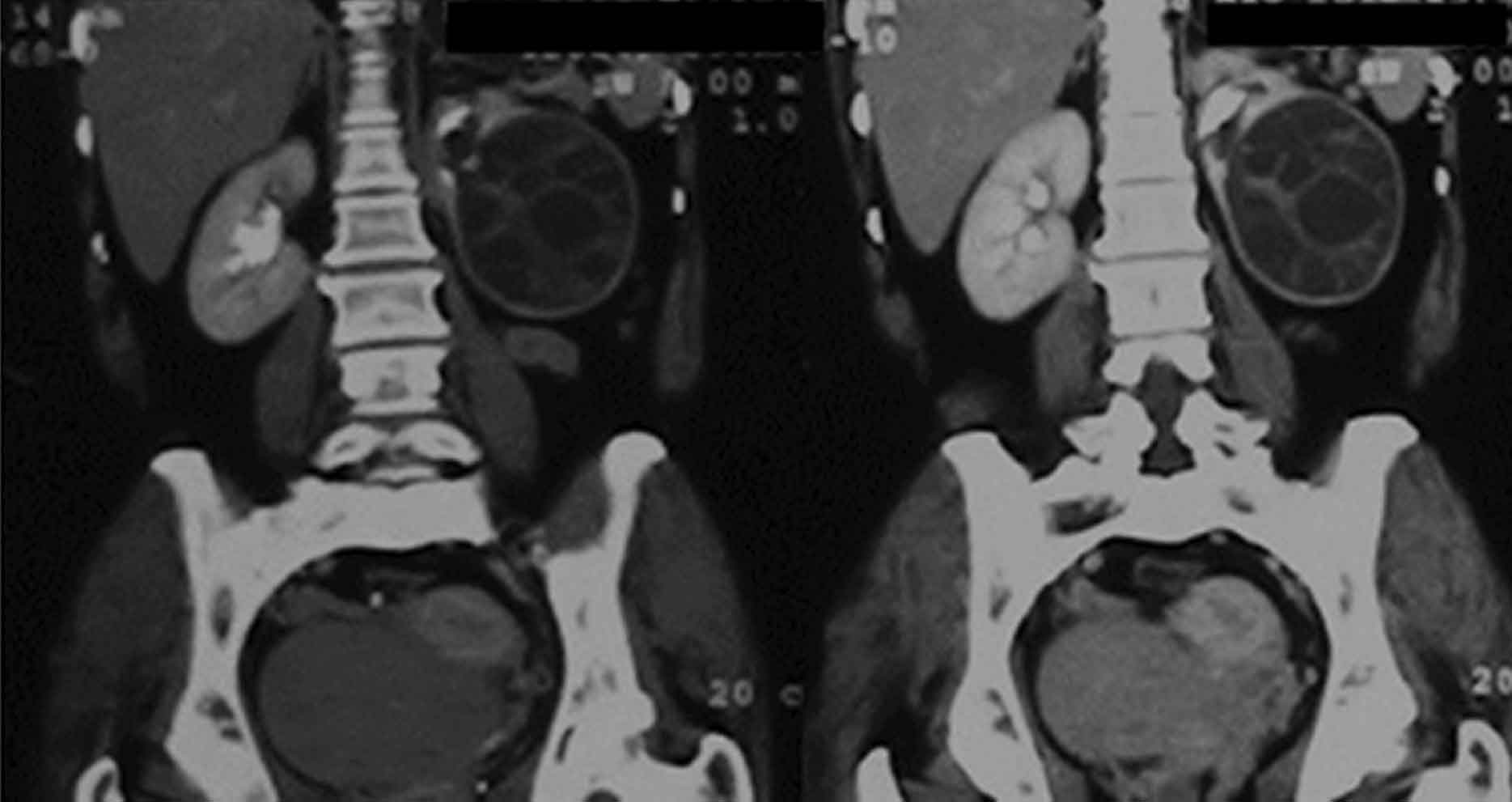
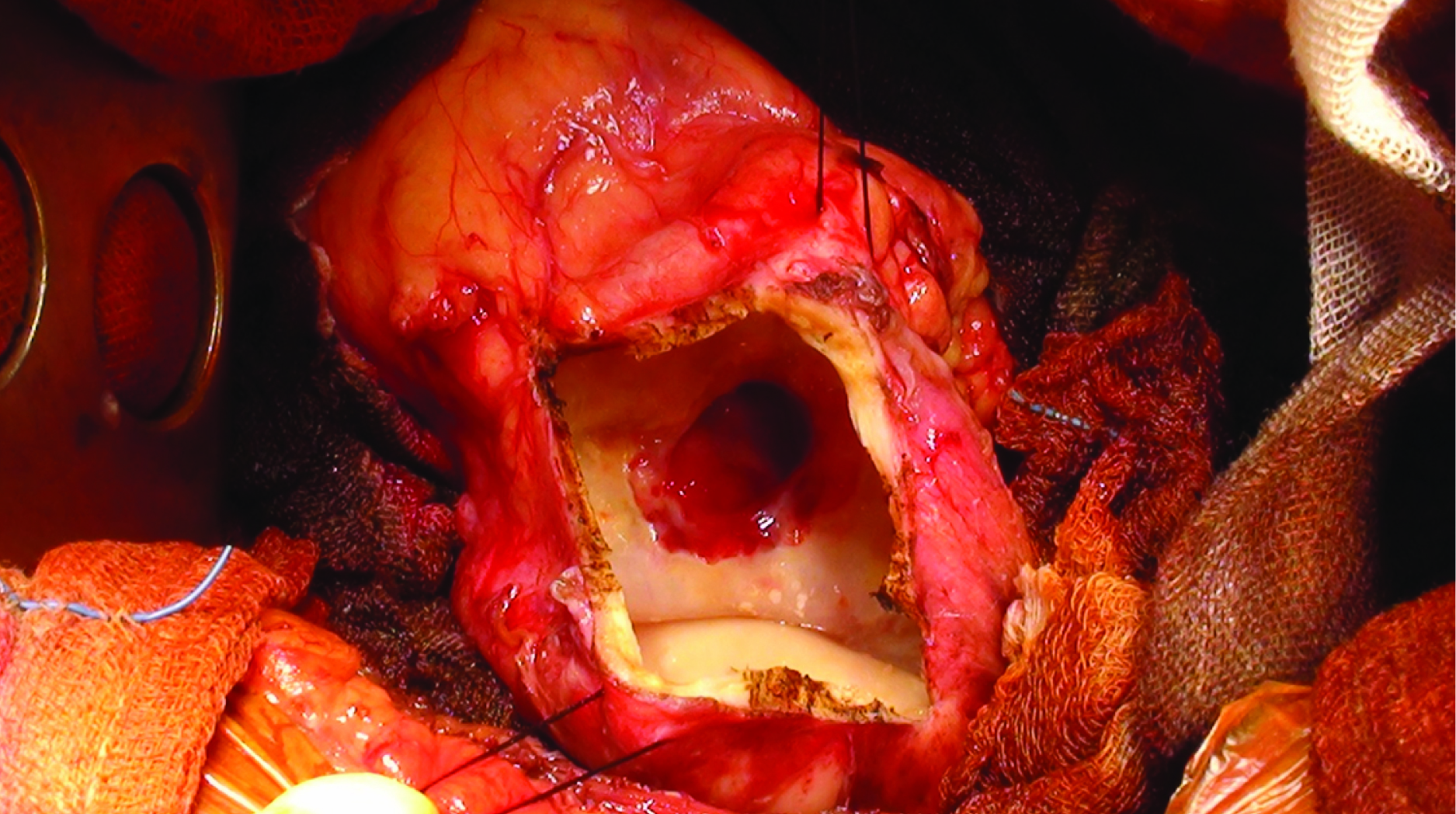
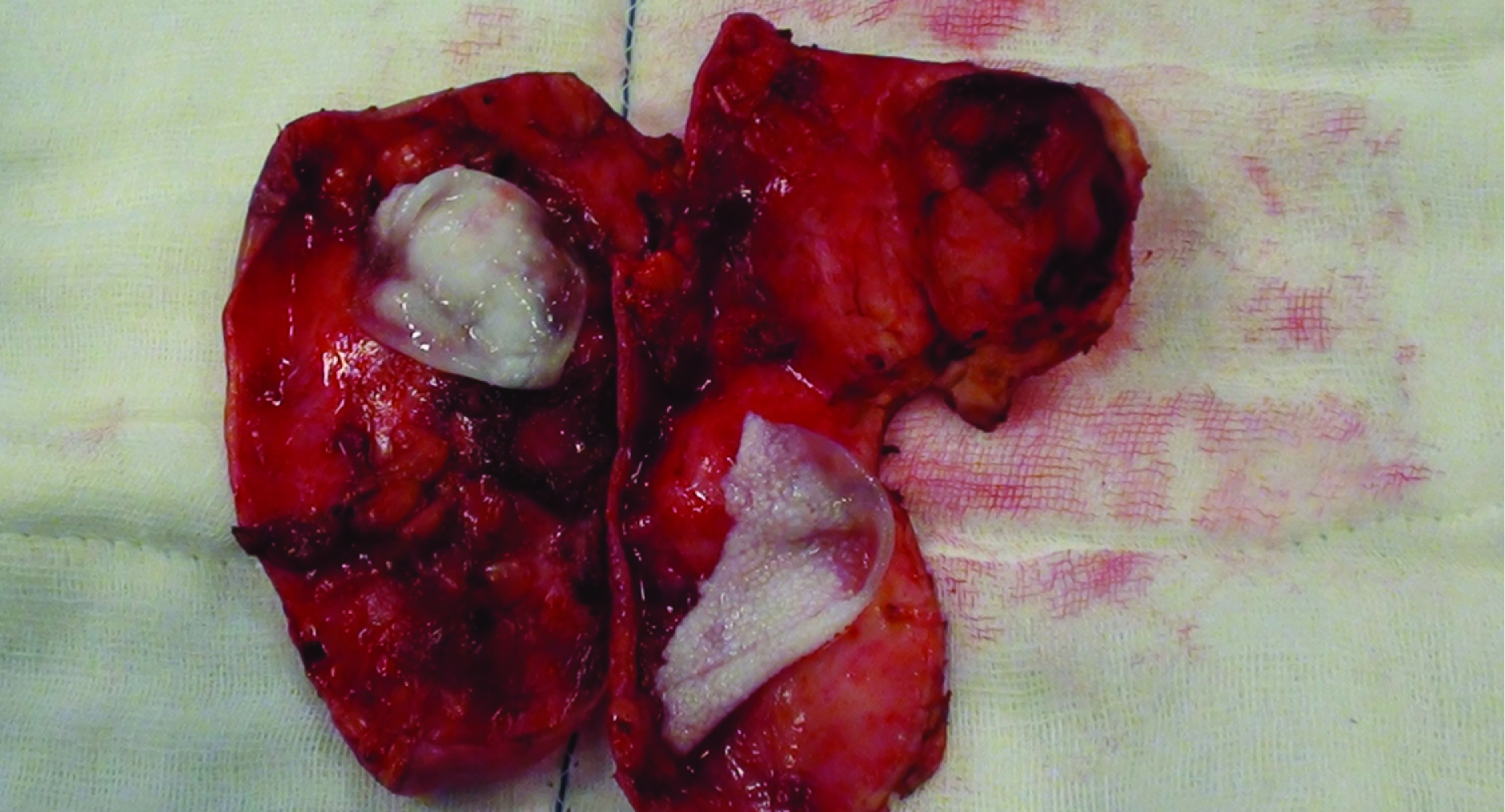
A 46-year-old female presented to the outpatient clinic at SGPGI, Lucknow, India, with complaints of left flank pain and passage of fleshy grape like vesicles in urine for last one year. There was no history of fever. On abdominal examination, there was no palpable lump. Ultrasonography showed an isolated multicystic lesion with internal echoes and floating membrane in the mid pole region of the left kidney. Contrast Enhanced CT (CECT) abdomen with CT urography revealed a 7.8 X 6.9 X 5.7 cm well-defined multiloculated cyst in the mid and lower pole of left kidney suggestive of hydatid cyst [Table/Fig-1] which was seen communicating with the collecting system of the adjacent midpole calyx. Hydatid serology was positive. Serum creatinine was 1.42 mg/dL. Glomerular Filtration Rate (GFR) as determined by the DTPA scan was 44 mLmin for the right kidney and 18 mL/min for the left kidney. She was started on oral Albendazole (400 mg twice daily). Four weeks later, she underwent left cystopericystectomy with left DJ stenting via open flank approach. The renal cyst was exposed and carefully mobilized all around. Povidone iodine (10%) soaked pads were placed all around the cyst. Cyst fluid was aspirated and spillage was avoided. A 1cm incision was given over the cyst wall and all cystic fluid and capsules were sucked out. Hypertonic saline was injected into the cyst and kept for 30 min. On further opening the cyst wall, the cyst cavity was seen to communicate with the PCS [Table/Fig-2]. Excision of the cyst was done followed by placement of a DJ stent with subsequent closure of PCS and renal capsule [Table/Fig-3]. Postoperative course was uneventful and the patient was discharged in healthy condition. Oral Albendazole was continued for 3 months. DJ stent was removed after 6 weeks and at 18 months of follow-up, the patient is asymptomatic. Postoperative GFR was 44 mL/min for the right kidney and 23 mL/min for the left kidney at 18 months after surgery.
CT urography-coronal reformats showing multiloculated hydatid cyst arising from mid and lower pole of left kidney communicating with PCS.
Intraoperative photograph showing communication of the renal hydatid cyst with the collecting system.
Resected specimen showing the laid open cyst cavity with 2 daughter cysts.
Discussion
Hydatid disease is a parasitic infestation caused by Echinococcus spp. (E. granulosus, E. vogeli and E. multilocularis). Renal-involvement is usually seen in disseminated disease, isolated involvement is extremely rare. There are no specific clinical symptoms and signs to diagnose renal hydatid disease [1]. Hydatid cysts grow slowly over a period of several years and may be associated with pressure symptoms or flank pain, depending on their size and location.
Hydatid cyst of the kidney can be of three types: closed type (with intact ectocyst, endocyst and pericyst), exposed cyst (without a pericyst) and open or communicating cyst (all the three layers have ruptured resulting in free communication with the collecting system) [2]. Ultrasonography is the initial investigation in the evaluation of the renal hydatid cyst since the presenting clinical features are usually nonspecific. CECT along with CT urography demonstrates the exact location of the cyst and communication with the PCS.
Treatment options for renal hydatid disease include medical treatment, percutaneous intervention, open surgery and minimally invasive surgery. Medical treatment with benzimidazoles such as albendazole has been recommended for lung and liver hydatid disease but no data are available on the efficacy of medical treatment in patients with renal hydatid cysts. Medical treatment should be used prophylactically against spillage before and after surgery. Percutaneous management can be a safe option for non-communicating cysts, with a theoretical but small risk of fatal anaphylaxis.
Surgery is the treatment of choice for most renal hydatid cysts since all other methods are suboptimal [3]. Surgical options include renal sparing surgery or nephrectomy depending upon residual renal function, hydatid cyst size, number, location (including connection with the collecting system), and expertise of performing surgeon. Renal sparing surgery is presently the most common approach for non-communicating cysts. It is performed in more than 75-80% of the cases. Nephrectomy (25% cases) is the treatment of choice for complicated renal hydatid cysts (communicating cysts, multiple cysts) and extensive renal disease where partial removal can lead to relapse and incomplete cure. A renal sparing surgery as well as nephrectomy can be performed laparoscopically or via open approach. The first laparoscopic partial nephrectomy for renal hydatid was performed by Basiri et al., who removed a 4.4-cm calcified lower pole renal mass using transperitoneal approach, without opening the cyst [4]. The first retroperitoneal approach for the same was reported by Ozden et al., [1]. Since then, several reports of laparoscopic partial nephrectomy and pericystectomy have been published [5,6]. However, all these reports describe the management of a typically “closed” cyst which does not communicate with the pelvicalyceal system.
In a communicating cyst, pericystectomy is feasible but at the point of communication with the collecting system, the cyst wall is precarious. Improper closure of the collecting system can lead to urinary fistula. Perhaps for this reason, there have been no reports of laparoscopic approach for the management of communicating hydatid cyst. The reports describing the open renal sparing approach for the management of gross hydatiduria have recommended wedge resection/ partial nephrectomy/ partial pericystectomy followed by capitonnage but have not specifically commented on the repair of the pelvicalyceal system, probably suggesting non-communication at the time of surgical resection [7]. In case of partial cyst excision, it is recommended to inject scolicidal agent before opening the cyst [8]. For a cyst communicating with the collecting system, this may mean direct instillation of the scolicidal agent into the collecting system which can have significant complications. Most of the scolicidal agents are also sclerosants which can damage the urothelium. In fact, even for simple renal cysts planned for sclerotherapy, communication with the collecting system precludes instillation of sclerosant [9]. A viable hydatid cyst has a relatively high intracystic pressure (54 ± 21 cmH2O) which means that if the scolicidal agent is injected before opening the cyst, it requires a higher pressure which increases the chances of entry into the PCS [10]. Therefore, the scolicidal agent must be injected only after opening the cyst for communicating hydatid cysts. Watertight closure of the PCS following cyst excision is of utmost importance. Placement of DJ stent ensures a low pressure system which may decrease the chances of urinary leak. The stent can be easily placed through the opening in the PCS identified at the time of cyst excision. Following closure of PCS, a standard renorrhaphy is done.
In our case, we did a successful renal sparing surgery in a complicated renal hydatid cyst (communicating with the PCS) with excellent patient recovery. The main concern in our patient was to save the progression to chronic kidney disease. As such, our patient had a borderline serum creatinine and the global preoperative GFR was 62 mL/min. A total nephrectomy in our patient would have rendered her as CKD 3 as per K/DOQI classification [11]. By attempting renal sparing surgery the patient was able to retain the compromised kidney. To our knowledge, this is one of the very few cases of communicating renal hydatid cyst managed successfully with renal sparing and repair of the PCS.
Conclusion
The renal sparing surgery may be a feasible approach in patients with renal hydatid disease with communicating cyst and borderline renal function. The focus should be on minimizing spillage, avoiding instilling scolicidal agent before opening the cyst to avoid entry into the PCS, complete removal of the cyst wall and adequate closure of the PCS. As laparoscopic surgery continues to evolve, what we have performed via open approach may soon be replicated laparoscopically.
[1]. Ozden E, Bostanci Y, Mercimek MN, Yakupoglu YK, Yilmaz AF, Sarıkaya S, Renal hydatid cyst treatment: retroperitoneoscopic “closed cyst” pericystectomyInt J Urol 2011 18(3):237-39. [Google Scholar]
[2]. Mongha R, Narayan S, Kundu AK, Primary hydatid cyst of kidney and ureter with gross hydatiduria: A case report and evaluation of radiological featuresIndian J Urol 2008 24(1):116-17. [Google Scholar]
[3]. Rexiati M, Mutalifu A, Azhati B, Diagnosis and surgical treatment of renal hydatid disease: a retrospective analysis of 30 casesPLoS ONE 2014 9(5):e96602 [Google Scholar]
[4]. Basiri A, Nadjafi-Semnani M, Nooralizadeh A, Case report: laparoscopic partial nephrectomy for isolated renal hydatid diseaseJ Endourol 2006 20(1):24-26. [Google Scholar]
[5]. Divarci E, Ulman I, Avanoğlu A, Retroperitoneoscopic laparoscopic treatment of renal hydatid cyst in a childJ Pediatr Surg 2010 45(1):262-64. [Google Scholar]
[6]. Aggarwal S, Bansal A, Laparoscopic management of renal hydatid cystJSLS 2014 18(2):361-66. [Google Scholar]
[7]. Gharde P, Wagh D, Patil A, Left renal hydatid cyst presenting as hematuria and macroscopic hydatiduria since last ten yearsTrop Parasitol 2012 2(1):58-60. [Google Scholar]
[8]. Shukla A, Garge S, Verma P, A case of large renal hydatid cystSaudi J Kidney Dis Transpl 2011 22(3):538-40. [Google Scholar]
[9]. Lee J, Darcy M, Renal cysts and urinomasSemin Intervent Radiol 2011 28(4):380-91. [Google Scholar]
[10]. Tsimoyiannis EC, Siakas P, Glantzounis G, Tsimoyiannis JC, Karayianni M, Gossios KJ, Intracystic pressure and viability in hydatid disease of the liverInt Surg 2000 85(3):234-36. [Google Scholar]
[11]. Kidney National Foundation K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratificationAm J Kidney Dis 2002 39(2 Suppl 1):S1-266. [Google Scholar]