All That Glitters is Not Gold: All Unilateral Oedema is Not DVT
Ashwal Adamane Jayaram1, Padmakumar Ramachandran2, Tom Devasiya3, Abdul Razak Uddina Kumeri4, Umesh Pai5
1 Assistant Professor, Department of Cardiology, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
2 Professor, Department of Cardiology, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
3 Professor, Department of Cardiology, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
4 Assistant Professor, Department of Cardiology, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
5 Assistant Professor, Department of School of Allied Health Sciences, Manipal University, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ashwal A. Jayaram, Assistant Professor, Department of Cardiology, Kasturba Medical College, Manipal University, Manipal-576104, Karnataka, India.
E-mail: dr.ashwal@gmail.com
Innominate vein stenosis or thrombotic occlusion can occur in dialysis patients. Central vein stenosis is a common problem in patients on dialysis. Placement of a central vein catheter for dialysis access increases the risk of central vein stenosis. Central vein stenosis sometimes can jeopardize the arteriovenous fistula and arteriovenous graft in the ipsilateral extremity unless recognized early and treated.
We describe three patients with left innominate vein stenosis who were known case of chronic kidney disease on haemodialysis and had a left brachio-cephalic fistula and presented with unilateral facial and upper limb oedema.
Haemodialysis, Innominate vein stenosis, Percutaneous intervention
Case Report
Case 1
A 51-year-old, man with a five year history of dialysis dependent renal failure and left brachio-cephalic arteriovenous fistula, presented with a three week history of gradually progressive haemifacial and unilateral upper limb swelling.
On examination there was oedema of the left face and upper limb with dilated veins over the face and neck. His blood pressure was 150/90mmHg in the right upper limb.
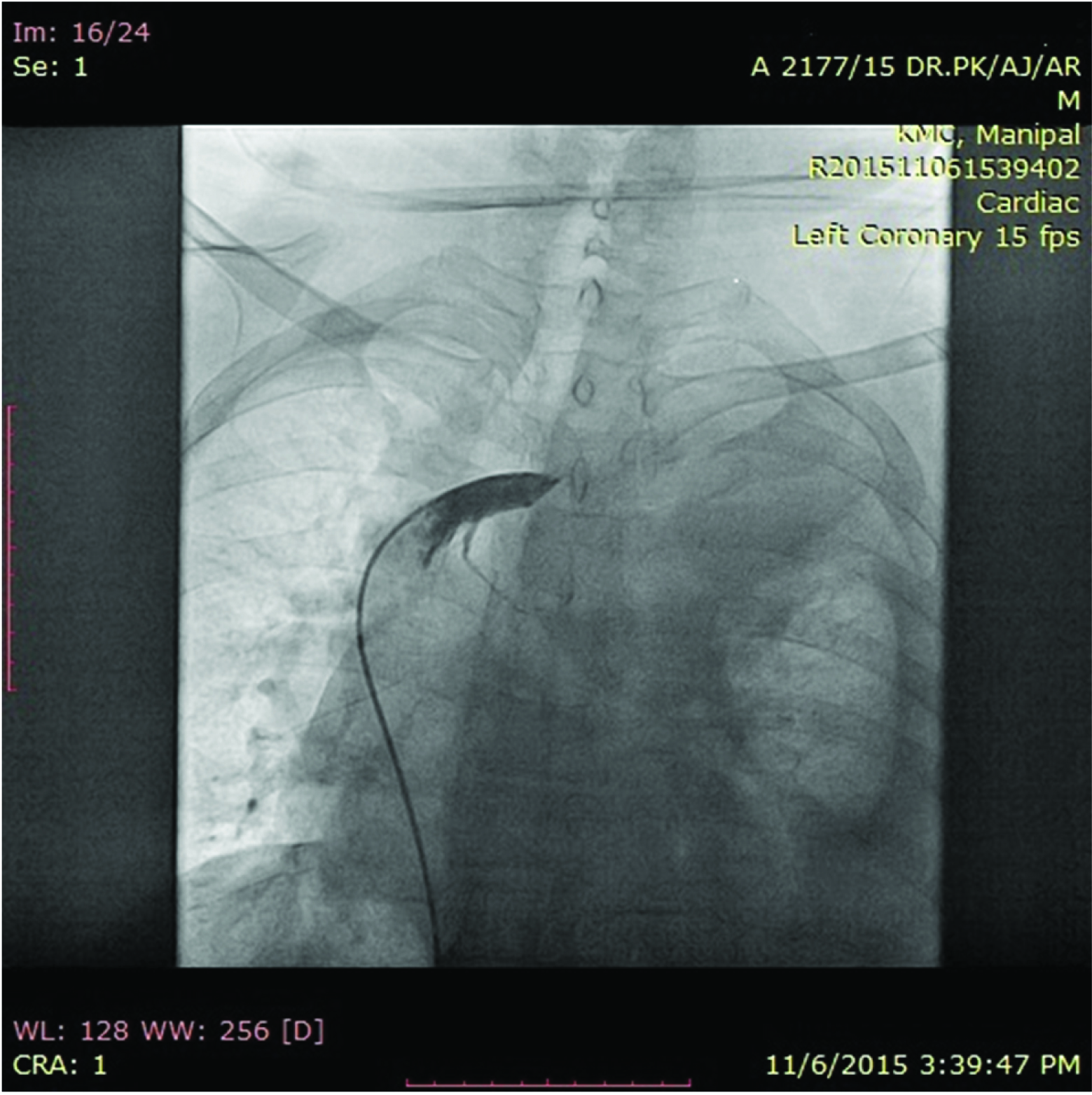
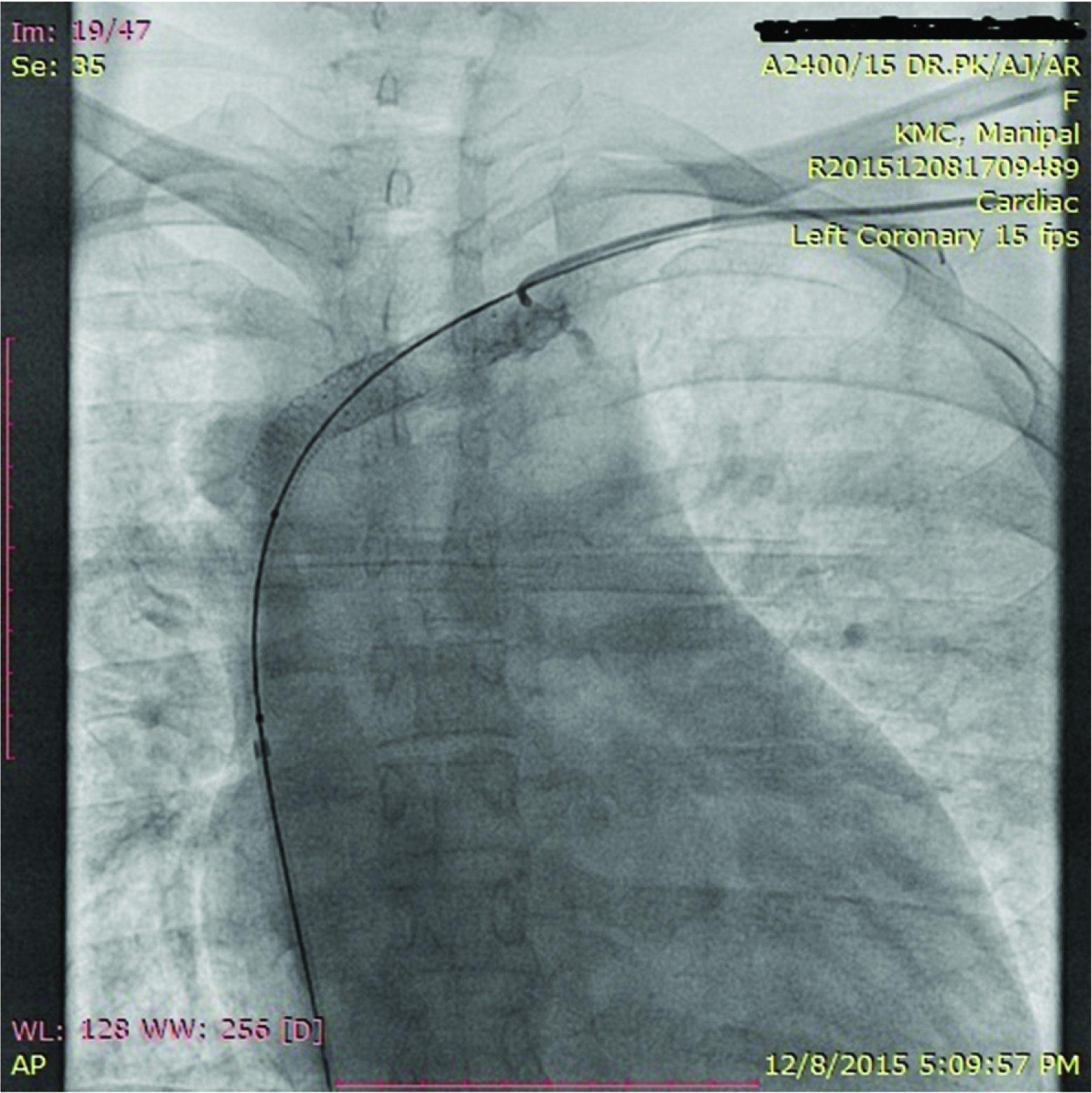
Left upper limb doppler was done which showed no evidence of venous thrombosis or arterial occlusion. A central venogram revealed a left innominate vein 100% stenosis at the junction with the superior vena-cava (SVC) [Table/Fig-1]. Access through the femoral vein and basilica vein was achieved and percutaneous transluminal angioplasty and stenting was done. The patient on subsequent follow-up showed a significant decrease in the hemifacial and upper limb oedema.
Selective angiography of left innominate vein shows 100% occlusion.
Case 2
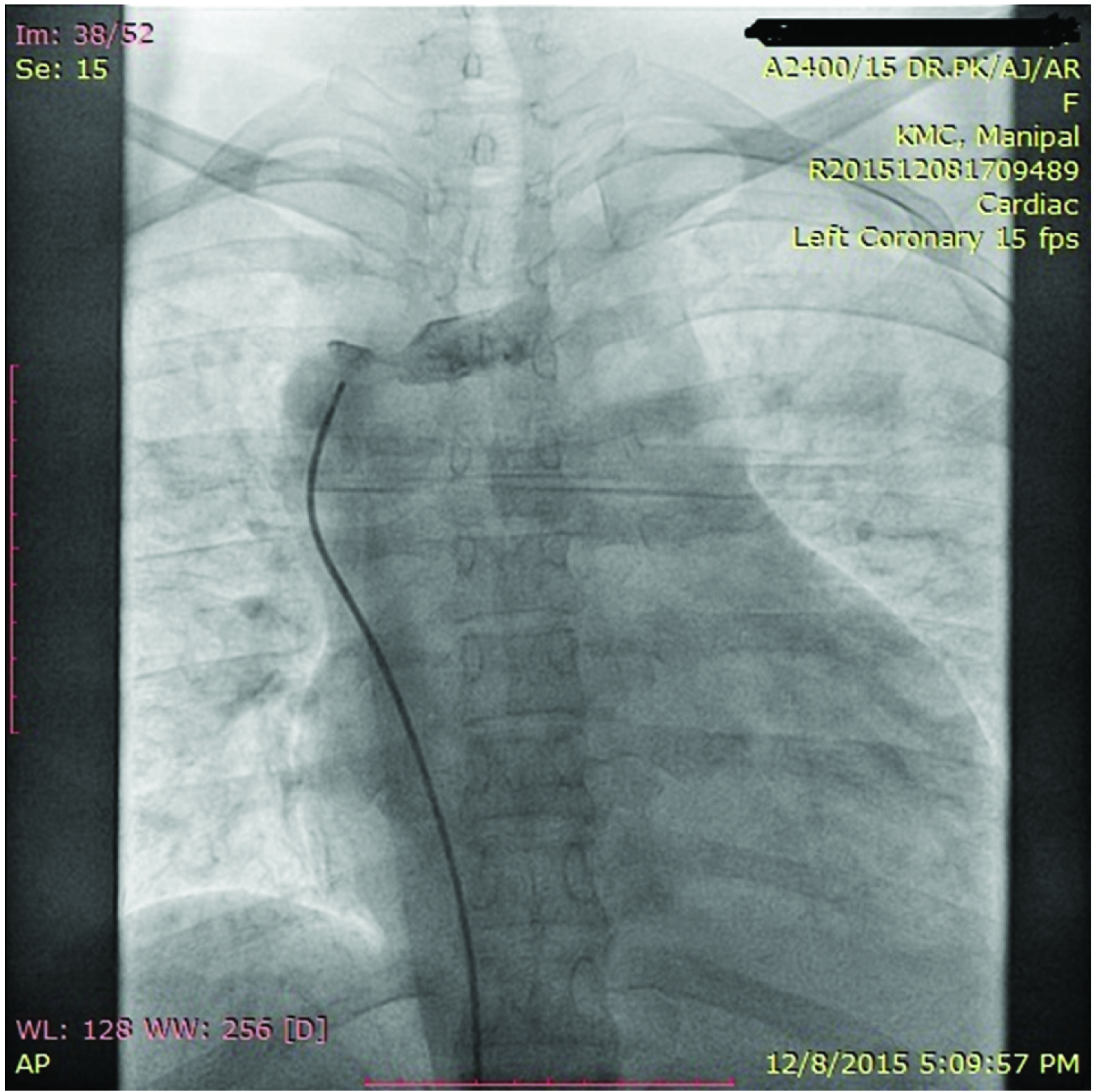
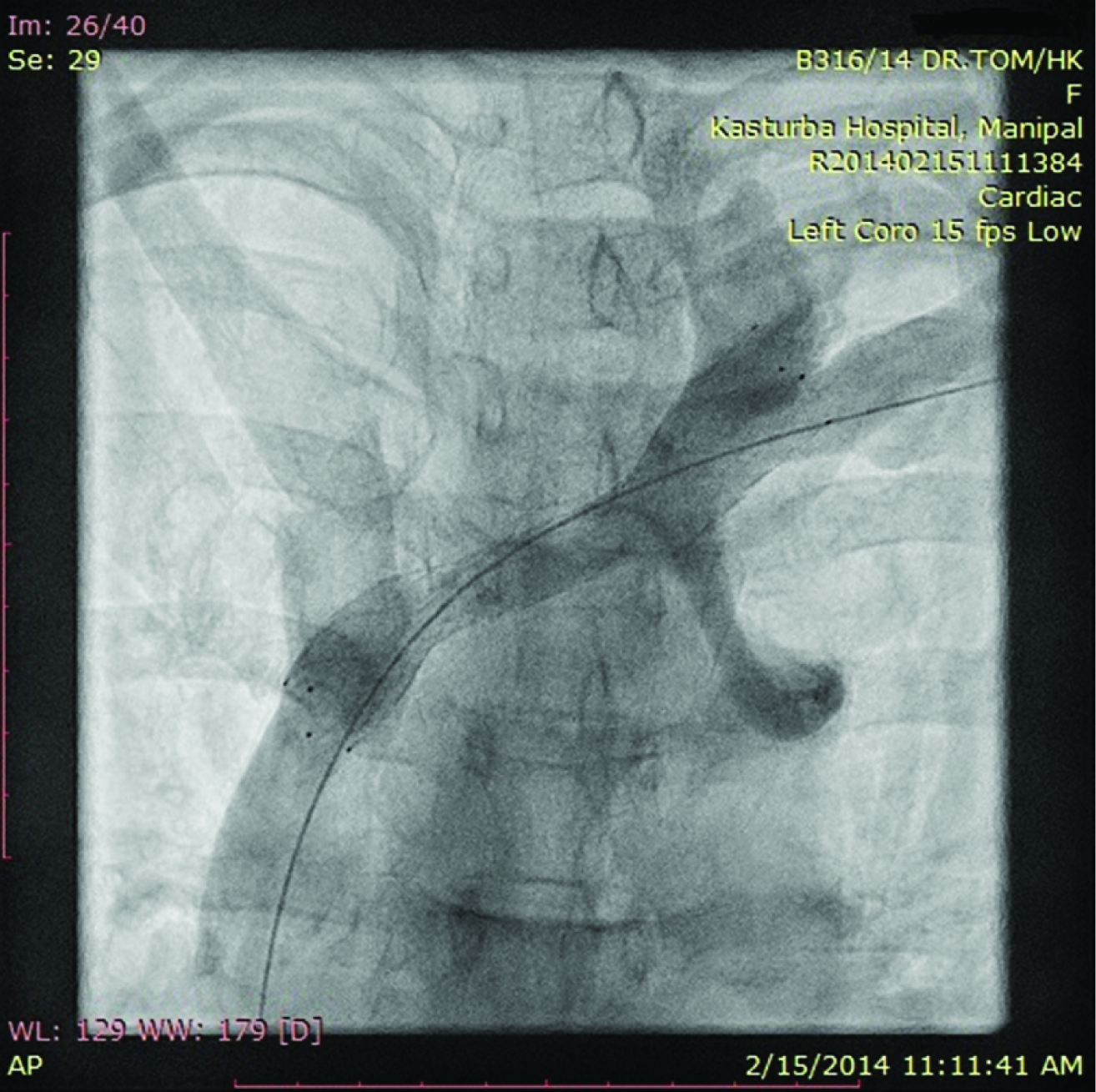
A 31-year-old woman presented with three year history of dialysis dependent renal failure and left brachio-cephalic arteriovenous fistula and two weeks history of gradually increasing swelling of unilateral left upper limb. Central venogram showed left innominate vein stenosis 80% at the junction with the SVC [Table/Fig-2]. Percutaneous stenting was done through the right femoral vein access and post procedure follow-up, the oedema of the left hand was significantly reduced.
Selective angiography of SVC and Innominate vein shows left innominate vein stenosis 80% at the junction with the SVC.
Case 3
A 47-year-old woman with two year history of dialysis dependent renal failure presented with failure and left brachio-cephalic arteriovenous fistula and one week history of gradually increasing swelling of unilateral left upper limb swelling. Central venogram showed left innominate vein stenosis 90% at the junction with the SVC [Table/Fig-3]. Percutaneous stenting was done through the right femoral vein access and post procedure follow-up, the oedema of the left hand was significantly reduced.
Central venogram showed left innominate vein stenosis 90% at the junction with the SVC. We can also see the stent placed across the lesion.
Method
After informed consent was taken, right femoral vein and left basilica vein access was taken with 6 French sheaths. Selective angiography of the innominate vein and SVC revealed left innominate vein stenosis. Lesion was crossed from the SVC using J tipped Terrumo (Medtronic) & 6 French 3.5 curve Judkins right guide (Cordis). Then the Judkins right catheter (Cordis) was exchanged with Mullins sheath (Cook). A 3.5 curve 6 French Judkins catheter was used to give injections from the left basilic vein.
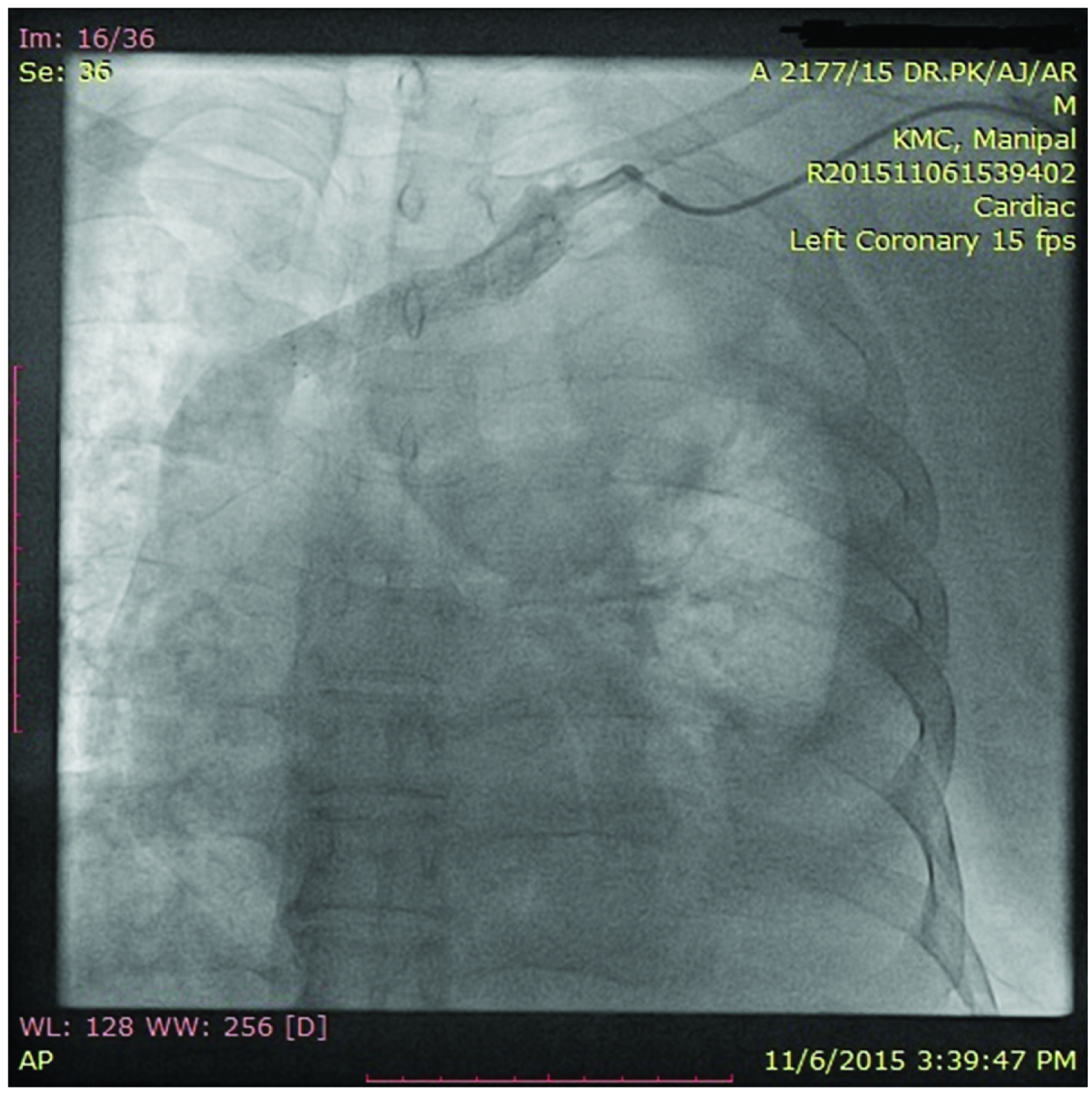
In the first case, lesion was predilated with 8x30mm Scuba stent balloon (Medtronic) at 12 atm and 10x60mm Complete SE vascular self-expanding stent (Medtronic) deployed and post dilated at 10 atm with 10x30 mm Scuba stent balloon (Medtronic) without any complications [Table/Fig-4].
Central venogram showing fully expanded stent at the SVC-Innominate vein junction with good flow.
In the second case, 10 x40mm complete SE self-expanding vascular stent (Medtronic) deployed distallyand 10x37mm Scuba balloon expandable stent (Medtronic) deployed at 12 atm proximally. Post procedure uneventful with good flow [Table/Fig-5].
Central venogram showing fully expanded stent at the SVC-Innominate vein junction with good flow.
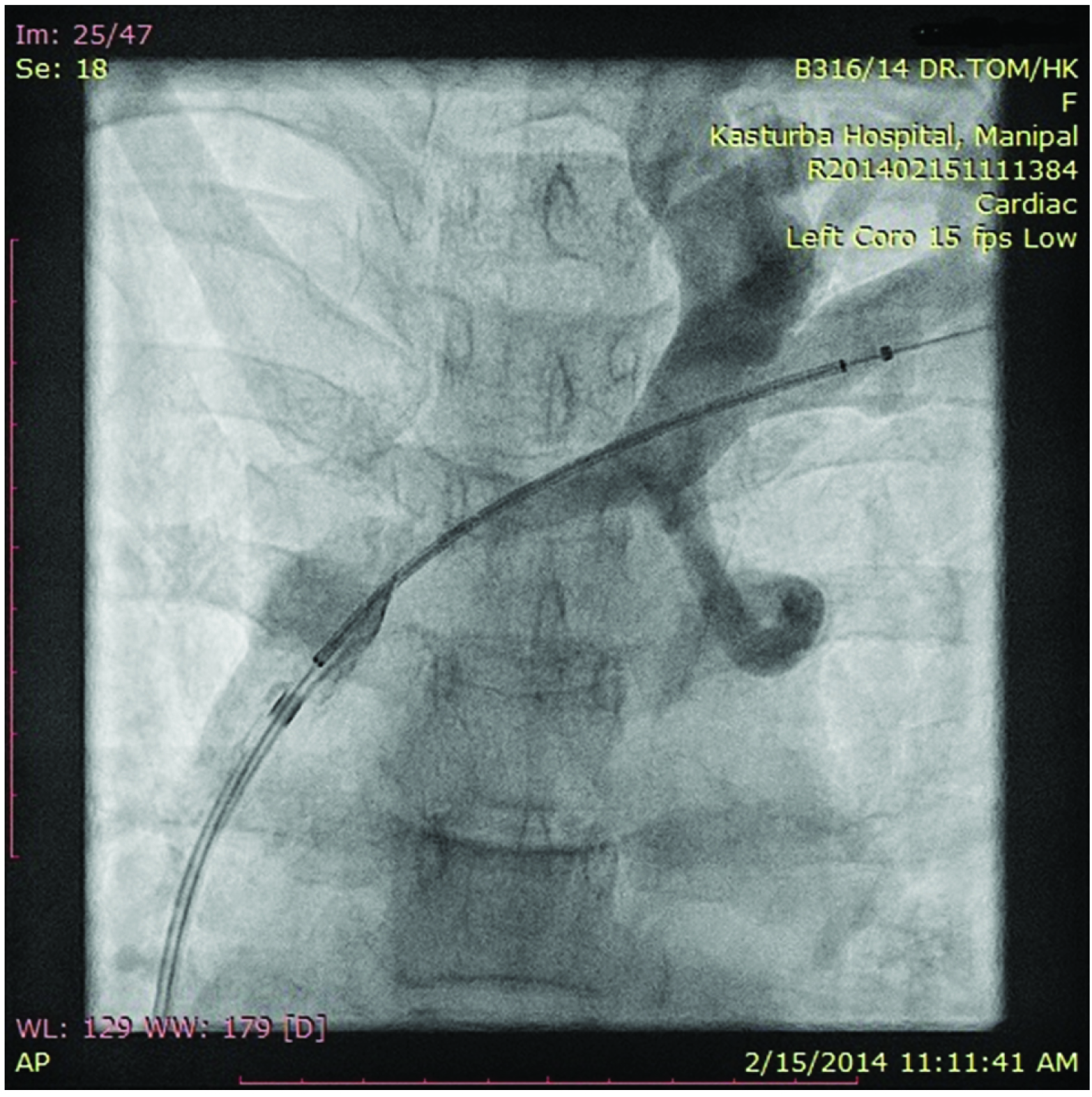
In the third case, lesion was predilated with 4x40mm Mustang (Boston Scientific) balloon at 8 atm and 7x30mm Optopro balloon (Cordis) at 8 atm. 14x80mm Zilver (Cook) stent was deployed at 8 atm and post dilated with 10x40mm Optopro Balloon (Cordis)at 16 ATM [Table/Fig-6]. No post procedure complications occurred.
Central venogram showing fully expanded stent at the SVC-Innominate vein junction with good flow.
Discussion
One of the important causes for central vein stenosis is the insertion of a central venous catheter but, in up to 40% of patients, cause can be unknown [1,2]. Some studies have shown up to 42% patients on haemodialysis with central vein catheters can have stenosis/angulations of the central veins [2]. Incidence of such deformities is almost double in patients having history of central vein catheterization (15 out of 23 patients (65%) versus 14 out of 46 patients (30%); p=0.009) [3].
The vessel, the population studied and the type of catheter influence the incidence of central vein stenosis [4]. Focal endothelial denudation in vessels due to early intimal following the use of central vein catheters is the main reason for the stenosis [5]. Thickening of the wall of vein and enhanced smooth muscle cell production due to longer duration of catheter use causes thrombus and collagen formation.
The management of central vein stenosis includes observation of the patient, radiological intervention/angioplasty or surgery. Asymptomatic stenosis, even if it is greater than 50%, may not require treatment. In a retrospective study of 35 patients on haemodialysis with asymptomatic central vein stenosis, 28% of the patients in whom the lesions were left untreated remained asymptomatic and none of them progressed [6]. Percutaneous intervention with transluminal angioplasty is the treatment of choice as the surgical therapy of these central lesions remains very complex. Stent placement is justified as its use will clearly result in one or more of the following benefits: extends access life, saves an otherwise failed access and avoids surgery. As per available reports; primary patency rates following the venous use of stents have been relatively poor, being approximately 20% at one year [7–9]. This approach is in consent with the Kidney Disease Outcomes Quality Initiative guidelines for vascular access [10]. Guidelines recommend that stent placement should be considered in cases of acute elastic recoil of the vein (greater than 50% stenosis) after balloon angioplasty and in patients with recurrent stenosis within a three-month period post-angioplasty [3].
Conclusion
Our patient presented with a near-total central vein stenosis and was successfully treated with balloon angioplasty and stent placement. Central vein stenosis is a common problem in many patients with central venous catheters for haemodialysis. They improve significantly in terms of the oedema of the hand, face and percutaneous angioplasty with stenting is very effective alternative treatment to surgery in these patients.
[1]. Oguzkurt L, Tercan F, Yildirim S, Torun D, Central venous stenosis in haemodialysis patients without a previous history of catheter placementEur J Radiol 2005 55(2):237-42. [Google Scholar]
[2]. Taal MW, Chesterton LJ, McIntyre CW, Venography at insertion of tunneled Internal jugular vein dialysis catheters reveals significant occult stenosisNephrol Dial Transplant 2004 19(6):1542-45. [Google Scholar]
[3]. Gottmann U, Sadick M, Kleinhuber K, Central vein stenosis in a dialysis patient: a case reportJournal of Medical Case Reports 2012 6:189 [Google Scholar]
[4]. MacRae JM, Ahmed A, Johnson N, Levin A, Kiaii M, Central vein stenosis: a common problem in patients on haemodialysisASAIO J 2005 51(1):77-81. [Google Scholar]
[5]. Forauer AR, Theoharis C, Histologic changes in the human vein wall adjacent to indwelling central venous cathetersJ Vasc Interv Radiol 2003 14(9 Pt 1):1163-68. [Google Scholar]
[6]. Levit RD, Cohen RM, Kwak A, Shlansky-Goldberg RD, Clark TW, Patel AA, Asymptomatic central venous stenosis in haemodialysis patientsRadiology 2006 238(3):1051-56. [Google Scholar]
[7]. Quinn SF, Schuman ES, Hall L, Venous stenoses in patients who undergo haemodialysis: treatment with self-expandable endovascular stentsRadiology 1992 183(2):499 [Google Scholar]
[8]. Vorwerk D, Guenther RW, Mann H, Venous stenosis and occlusion in haemodialysis shunts: follow-up results of stent placement in 65 patientsRadiology 1995 195(1):140 [Google Scholar]
[9]. Gray RJ, Horton KM, Dolmatch BL, Use of Wallstents for haemodialysis access-related venous stenoses and occlusions untreatable with balloon angioplastyRadiology 1995 195(2):479 [Google Scholar]
[10]. Vascular Access Work GroupClinical practice guidelines for vascular accessAm J Kidney Dis 2006 48(Suppl 1)S248-73 [Google Scholar]