Fine Needle Aspiration Cytology (FNAC) is one of the most common modalities employed for investigation of thyroid tumours. Cytomorphology and diagnostic Immunocytochemical (IC) markers including Thyroglobulin (Tg), Calcitonin (Cal) and Carcinoembryonic Antigen (CEA) have been widely studied in thyroid tumours.
We studied p63 and Bcl-2 expression in thyroid tumours on FNAC and biopsy specimens and their correlation with other diagnostic immunocytochemical markers.
Materials and Methods
This prospective study was conducted in the Departments of Pathology and Surgery, in a tertiary health care centre in Indian metropolitan city from November 2007 to April 2009. The inclusion criteria for the cases were: 1) patients presenting with neck mass with clinico-radiological suspicion of thyroid malignancy; and 2) clinically benign appearing thyroid swelling, but diagnosed as malignancy upon cytology/histopathology. Cases proved to be benign on cytology/ histopathology was excluded from the study.
Detailed history was recorded and examination was done. Neck radiography, Ultrasonography (USG), Thyroid Function Tests (TFT), thyroid scan, any prior cytological/ histological findings, and other relevant investigations were included wherever available.
FNAC was performed in all cases as per the standard technique using a 23/24 gauge needle, under aseptic precautions. Multiple smears were prepared, of which 2-3 were processed as air dried, methanol fixed, Giemsa stained smears. Rest were fixed in acetone and preserved for Immunocytochemistry (IC). Grossly haemorrhagic and large volumes of aspirates were processed for cell block preparation along with smears. Formalin fixed paraffin embedded cell block sections were studied for morphology and immunocytochemistry wherever required.
Formalin fixed paraffin embedded tissue sections from excision specimens were processed as per standard procedure. Morphological features were studied in detail and tumour typing performed on both cytology smears and histopathology (HPE) specimens. Immunocytochemistry was done on FNA smears and deparaffinized tissue sections by staining with Avidin-biotin complex method using Diamino benzidine as chromogen. Bcl-2 and p63 was done in all cases. For Bcl-2 (Anti Bcl-2 Oncoprotein) - >25% of cells with cytoplasmic staining was considered as positive result; and p63 (p63 Ab-4) – nuclear staining was considered as positive. For other diagnostic markers (applied as and when required depending on morphology) i.e., Tg, Cal and CEA – definite cytoplasmic staining was considered positive. For interpretation of immunocytochemistry, 500 cells were counted and percentage of positive tumour cells was calculated. Intensity of staining was graded as:
0 – negative
1+ – weak
2+ – moderate
3+ – strong
Staining Intensity score (SI) was calculated by multiplying percentage of tumour cells staining positive by intensity of staining for all markers. Excision specimens were available in 20 cases and Cyto-Histological Correlation (CHC) was performed.
Statistical Analysis
Statistical Analysis was performed with Student ‘t’-test, Fisher-Exact test and p-value less than 0.05 was taken as significant. Spearman’s correlation coefficient (ρ) was used to calculate correlation between immunocytochemical markers.
Results
A total of 35 cases were included in the study. The age at presentation ranged from 12-75 years (mean age 43.8 ± 16.99 years) with 1:1.8 male to female ratio. Anaplastic carcinoma (ATC) presented at a greater age (mean age at presention 61.4±7.4 years t-test, p-value <0.05) than in well differentiated thyroid cancer (WDTC, 40.97±16.4 years), the latter group including Follicular Carcinoma (FTC), PTC and MTC. Most patients presented [Table/Fig-1] with a progressively increasing swelling in the neck, few had pain in swelling, hoarseness, compressive symptoms, cervical lymphadenopathy and weight loss. Most cases were clinically euthyroid, and occasional cases were subclinical hyperthyroid (6.9%). Cervical lymph node (cx LN) metastases were seen in four cases (11.4%) and distant metastases (11.4%) detected in liver (5.7%), bone (8.57%), mastoid (2.86%), brain (2.86%), lungs (2.86%) and orbit (2.86%), including multiple sites (5.7%). Unusual presentations included papillary thyroid carcinoma metastatic to cervical lymph node with cystic change, recurrent follicular carcinoma presenting as a sternal mass and metastatic Follicular Variant of Papillary Carcinoma Thyroid (FV-PTC).
Clinical characteristics of the patients.
| Clinical characteristics | No. of cases n=32 | % |
|---|
| Neck mass | 33 | 94.3 |
| Hoarseness | 4 | 11.4 |
| Compression | 3 | 8.6 |
| Wt loss | 1 | 2.8 |
| Cx LAP | 5 | 14.3 |
| Cystic | 1 | 2.8 |
| Cervical lymph node metastases | 4 | 11.4 |
| Distant metastases | 4 | 11.4 |
The cytomorphologic features [Table/Fig-2] were studied in detail including cellular arrangement, cellular and nuclear morphology and other features including haemorrhage, necrosis, tumour diathesis, absence of colloid and amyloid. Additionally, there were psammoma bodies (3 cases, 8.57%) and features of lymphocytic thyroiditis (1case, 2.86%) that were associated with papillary thyroid carcinoma. Cytomorphology was supplemented by immunocytochemistry that played an important role in diagnosis, particularly in medullary carcinoma and anaplastic carcinoma. The main pitfalls we encountered were follicular lesions which require HPE for decision on malignancy and cases where the swelling yielded cystic aspirate with low cellularity.
a-c) FNA smears showing Giemsa stain: (a) Three dimensional groups and microfollicles of monotonous cells with nuclear crowding and overlapping (FTC x400). (b) Mono layered sheets, papillary fragments with fibrovascular core and regular borders (PTC, x200); inset - nuclear features of PTC (arrowhead - intranuclear inclusion) (x400) . (c) High cellularity with fish school pattern and spindle cells (MTC, x200); inset – plasmacytoid cells mixed with smaller oval cells (x400). (d) Large cells with pleomorphic nuclei (ATC, H&Ex400); inset - FNA smear showing pleomorphic tumour giant cell (Giemsa x400). (e) PTC – Papillae containing fibrovascular cores lined by low columnar epithelial cells (H&E x200); inset-optically clear nuclei (arrow - intranuclear inclusion) (x400). (f) MTC – Spindle cells arranged in fascicles with fine nuclear chromatin (x400).
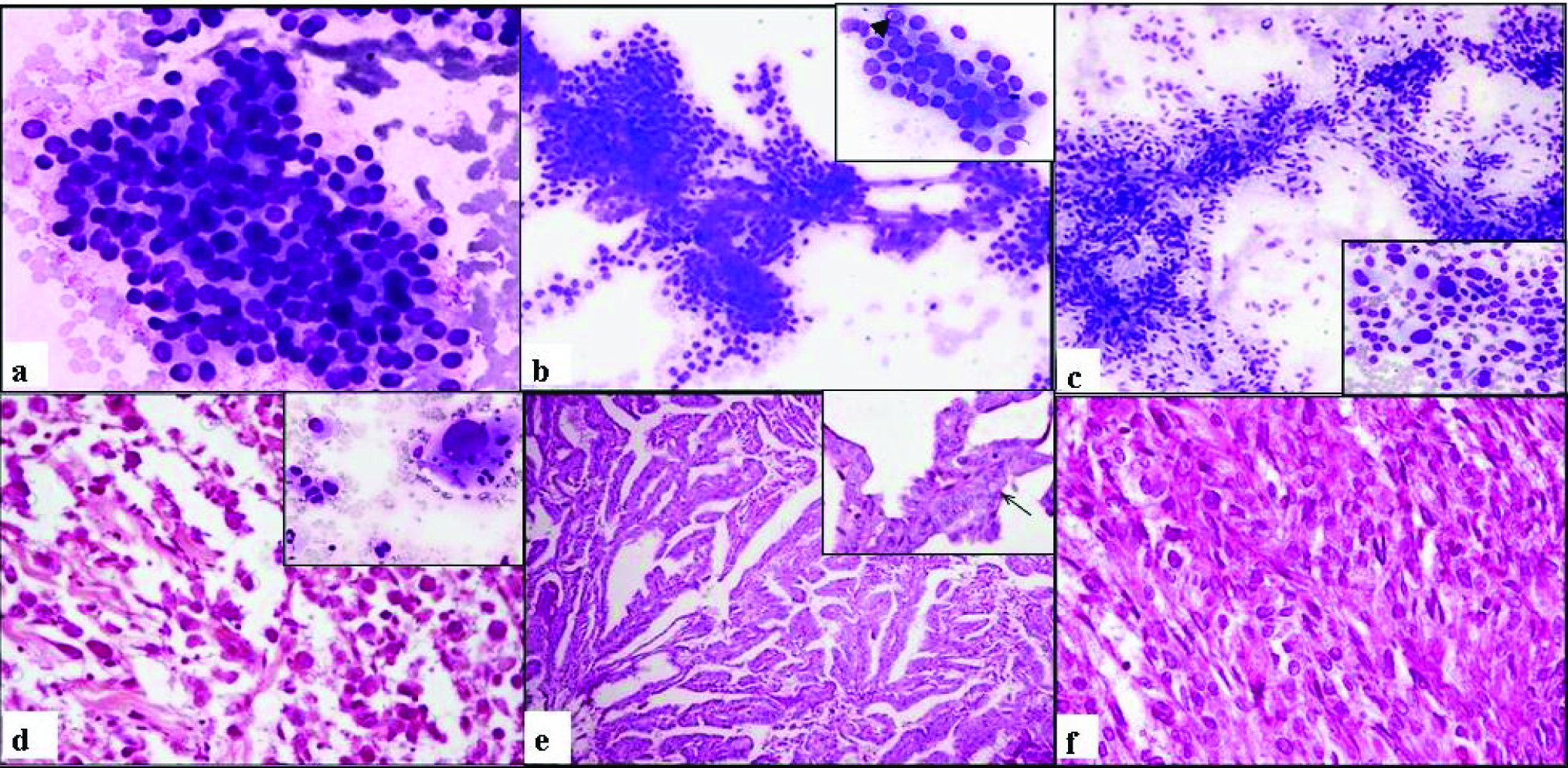
On FNAC, diagnosis of PTC was made in 12 cases (34.2%), MTC in 7 (20%) cases, ATC in 5 (14.3%) cases. Follicular lesions may have overlapping features and FN was considered in 9 cases (25.7%), with differential diagnoses of FTC in 6 cases (17.14%), and adenomatous goiter as a differential in 2 (5.7%) cases. Extrathyroid malignancy was considered in 2 cases (5.7%), and excluded using IC. Possibility of variants was considered on cytology in 4 cases (11.4%), including PTC (FV-PTC 2 cases, tall cell variant 1 case), and MTC (mucoepidermoid /mucin secreting – 1 case). Cell block was made in 14 (40%) cases, sections from which showed optimum morphology, and also allowed IC.
Histopathology [Table/Fig-2] was available in 20 cases [Table/Fig-3], wherein PTC was diagnosed in 8 cases (40%), including 6 (30%) Classical Papillary Thyroid Carcinoma (CPTC) and 2 (10%) FV-PTC; 7 cases (35%) were diagnosed as FTC (all with capsular invasion), while vascular invasion was seen in 2 cases (10%); 2 cases (10%) were diagnosed as minimally invasive FTC and one case (5%) as FTC with focal insular component. 4 cases (20%) were diagnosed as MTC and 1 case as ATC (5%).
Cytohistological correlation between diagnoses.
| Histo diagnosisn | Cyto-correlationn (%) | Non correlationn (Cyto Diagnosis) |
|---|
| CPTC | 6 | 5 (83.3%) | 1(CCG) |
| FTC | 7 | 6 (85.7%) | 1(CCG) |
| FV-PTC | 2 | 1(50%) | 1(FN) |
| MTC | 4 | 4(100%) | 0 |
| ATC | 1 | 1(100%) | 0 |
| Total | 20 | 17 (85%) | 3(15%) |
CPTC: Classical Papillary Thyroid Carcinoma, FTC: Follicular Thyroid Carcinoma, FV-PTC: Follicular Variant of Papillary Carcinoma Thyroid, MTC: Medullary Carcinoma, ATC: Anaplastic Carcinoma
Sensitivity was calculated as TP/(TP+FN) and positive predictive value (PPV) as TP/(TP+FP), where TP = number of true positive cases, FP = number of false positive cases and FN = number of false negative cases. Out of 20 cases of thyroid malignancy, for which HPE was available, diagnosis of thyroid malignancy was given on FNAC in 18 cases (90%), which is equivalent to sensitivity of the procedure. Two cases were false negative, both diagnosed as Cystic Colloid Goiter (CCG) on FNAC. One was diagnosed as PTC on excision and the other case was minimally invasive FTC. All cases diagnosed as malignant or with suspicion of malignancy on FNA cytology were reported as malignant on histopathology, wherever the latter was available. Therefore PPV was calculated to be 100%.
Overall cytohistological correlation [Table/Fig-3] for tumour typing was observed in 85% (17 cases), out of 20 cases available for histopathology. Follicular neoplasm is a grey area on cytology; the possibility of Follicular carcinoma/follicular neoplasm was given in 85.7% (6 out of 7) cases diagnosed on biopsy as follicular carcinoma. One case showed scant cellularity on FNAC with cystic macrophages. Diagnostic cytohistological correlation was 83.3% for classical PTC (5 out of 6) cases. One case was diagnosed as cystic colloid goiter. Follicular variant of papillary thyroid carcinoma was diagnosed in 50% (1 out of 2) cases. The other case was that of thyroid carcinoma with metastases to liver, bones and scalp; it was diagnosed as follicular carcinoma on FNA, but histopathology revealed features of FV-PTC. Medullary carcinoma revealed varied cytomorphological patterns, and diagnosis of MTC was made accurately on FNAC in 100% (4 cases), with the aid of immune markers. Histopathological correlation was available for anaplastic carcinoma in one case which was clinched on cytology. FNAC came out to be fairly accurate in typing the thyroid tumours with 85% (17 of 20 cases) overall correlation with biopsy diagnosis of however, for variant forms, it may not always be accurate.
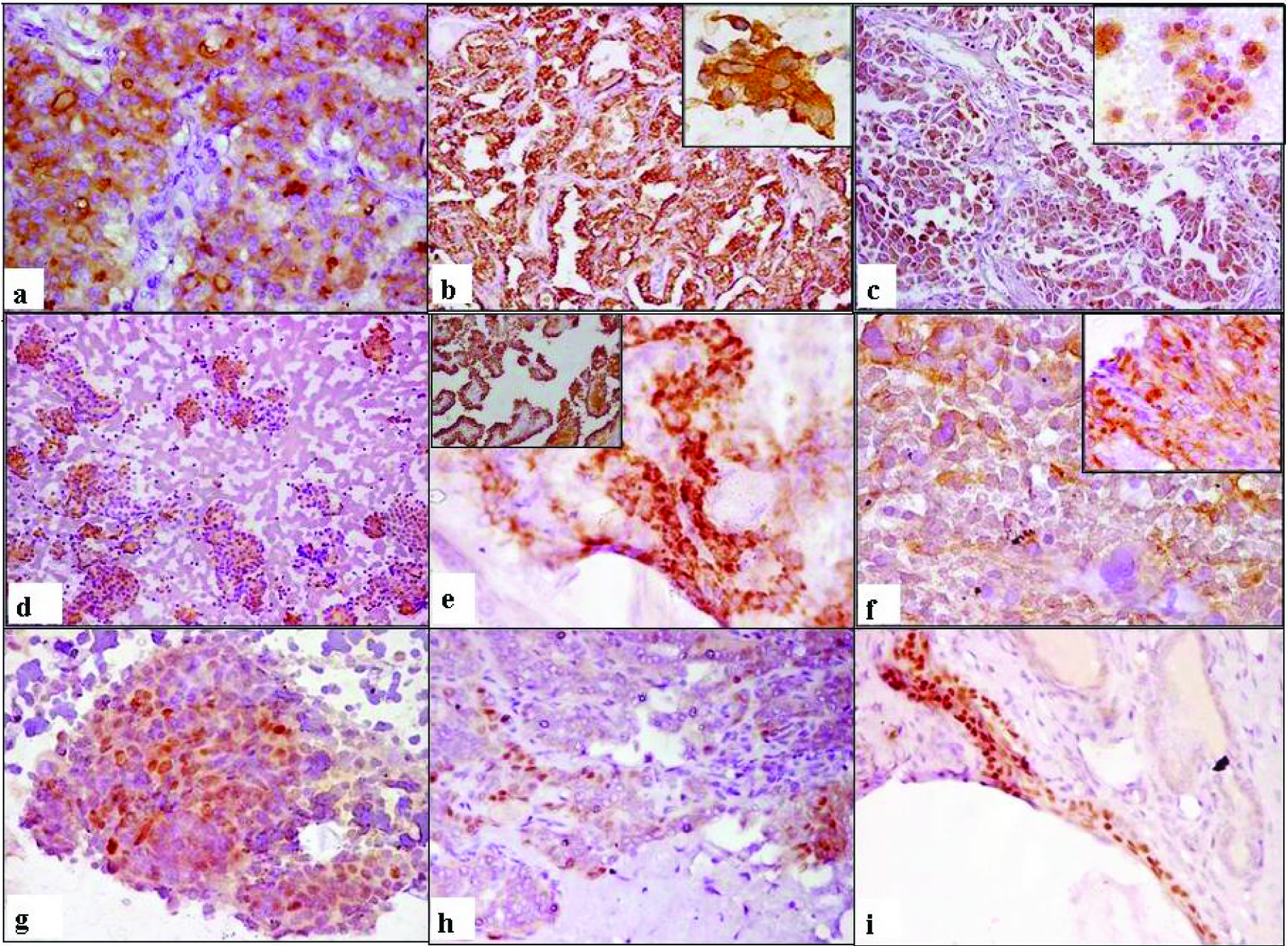
Immunocytochemistry [Table/Fig-4]: Bcl-2 expression was observed in all papillary carcinomas (100%) and most (88.89%) of follicular carcinomas. The mean staining intensity was significantly higher (t-test, p-value < 0.05) in FTC (190.94 ± 87.06) than in PTC (113.12 ± 60.19). Majority of medullary carcinoma cases expressed Bcl-2 (83.33%), with mean SI 136.17±82.52. Conversely, only 2/5 (40%) of anaplastic carcinoma cases showed focal weak expression of Bcl-2 (mean SI= 16.4). Cytohistological correlation for Bcl-2 was 88.24%. For statistical analysis, the data was subdivided into two subgroups; the criterion for downregulation was taken as <50% of the tumour cells showing Bcl-2 [3]. Anaplastic carcinoma showed significant down regulation of Bcl-2 (Fischer-exact test, p = 0.001) as compared to Well Differentiated Thyroid Carcinomas (WDTC), the latter group including FTC, PTC and MTC [Table/Fig-5].
Immunocytochemistry: (a-b)Tg: (a) FTC, tissue section IC x200 (b) PTC tissue section IC x200; inset FNA smear ICx400. (c) Cytoplasmic Cal expression in MTC, tissue section IC x200, inset FNA smear IC x400. (d-f) Cytoplasmic Bcl-2 staining: (d) FTC, FNA smear IC x100; (e) PTC, FNA smear IC x400, inset – tissue section IC x200; (f) MTC, FNA smear IC x400, inset – tissue section IC x200. (g-i) Focal nuclear positivity for p63 in PTC (g) FNA smear IC x400; (h) tissue section ICx200; (i) PTC with cystic change, tissue section IC x 200.
Downregulation of Thyroglobulin and BCl-2 in anaplastic carcinoma.
| Thyroglobulin n(%) (Fischer-exact test; p-value= 0.016) |
|---|
| SI | (FTC + PTC) | ATC | TOTAL |
|---|
| >261.75 | 14 (63.6%) | 0 | 14 |
| <261.75 | 8 (36.4%) | 5 (100%) | 13 |
| TOTAL | 22 | 5 | 27 |
| Bcl-2 n (%) (Fischer-exact test; p-value= 0.001) |
| % of positive cells | WDTC (FTC + PTC + MTC) | ATC | TOTAL |
| >50% | 23 (82.1%) | 0 | 23 |
| <50% | 5 (17.9%) | 5 (100%) | 10 |
| TOTAL | 28 | 5 | 33 |
SI: Staining Intensity, WDTC: Well Differentiated Thyroid Carcinomas, FTC: Follicular Thyroid Carcinoma, MTC: Medullary Carcinoma, ATC: Anaplastic Carcinoma, PTC: Papillary Carcinoma
p63 revealed distinct crisp nuclear staining present focally in the tumour cells, in 6 cases (18.18%); interestingly, all were papillary carcinomas (6/13; 46.1%) with the mean p63 expression 21.08 ± 10.10 (percentage of cells p63 +ve). In another case p63 staining was seen in cytoplasm of the tumour cells (not considered as positive) and not in the nuclei or surrounding thyroid. p63 expression was absent in MTC, FTC and ATC. Correlation between p63 immunostaining in FNA smears and histopathologic sections (83.3%) was observed in all cases of papillary carcinoma apart from one which showed only very few cells positive on cytology.
Tg was positive in all cases (100%) of well differentiated tumours with follicular differentiation (FTC, PTC) with variable expression (SI range 73–291; mean SI 231.64 ± 67.06; median SI 261.75), with good cytohistological correlation (94.12%). Anaplastic carcinomas showed Tg expression with a lower SI in 2/5 cases (40%). Overall, Tg expression was significantly downregulated (Fisher-Exact test, p-value = 0.016) in anaplastic carcinoma than in FTC, PTC subgroup; where median SI (261.75) was taken as cut-off value for Tg downregulation.
Cytoplasmic Cal and CEA expression with variable SI was observed in all 6 cases (100%) of medullary thyroid carcinoma where IC was performed; Cal SI range 77–260.5, with mean SI 179.58 ± 71.95 and median SI was 182.75 and; CEA SI score range 67–288, with mean SI 178.17 ±72.33 and median SI 174.25. HPE was available in 4 cases with 100% cytohistological correlation for Cal and 75% for CEA. 95.45% of well differentiated thyroid carcinomas with follicular differentiation (FTC, PTC) were positive for both Tg and Bcl-2; and none of the anaplastic carcinomas showed expression for both markers together. Overall a weak positive correlation (ρ = 0.65) was noted between Tg and Bcl-2 expression in FTC, PTC and ATC. All medullary thyroid carcinoma cases were positive for both Cal and CEA (100%) and 83.33% of cases showed Bcl-2 expression, with strong positive correlation between Bcl-2 and Cal (ρ = 0.93) and Bcl-2 and CEA expression (ρ = 0.89).
Discussion
Thyroid cancer is the most common endocrine cancer accounting for 1% of all cancers [11]. FNAC is currently the first line tool in evaluation of thyroid nodules [12,13], that helps in diagnosis and deciding the management. It has good accuracy in diagnosing PTC and MTC, but has limitations regarding Follicular Thyroid Carcinoma (FTC) and morphological variants including FV-PTC [14–16]. In this study FNAC showed good sensitivity (90%), positive predictive value (100%) and cyto-histologic correlation for typing of thyroid carcinomas (85%). Immunocytochemistry can be applied on smears, cell block and tissue sections. It can help in diagnosis, particularly in cases with morphological overlap on cytomorphology. MTC may show varied cytomorphological patterns and immunostaining for Cal, and CEA may prove to be diagnostic [17]. ATC is usually negative for Tg and Cal [17,18].
Bcl-2 is a unique antiapoptotic proto-oncogene [1], discovered in follicular B cell lymphoma [19]. It is expressed in long lived progenitor cells and tissues with increased turn over, including breast epithelia, prostate, thyroid follicles, basal layers of skin and colonic crypts. Physiologically, it may prevent apoptosis in thyroid epithelia [20]. Overexpression of Bcl-2 has been observed in the cytoplasm of main cells of solid cell nests [21]. Bcl-2 family of proteins may play an important role in the pathophysiology of thyroid tumours derived from follicular epithelium, by disturbing the equilibrium between proapoptotic and antiapoptotic events [22]. It is expressed in thyroid tumours including PTC [2,7], FN and MTC, while only a small proportion of undifferentiated thyroid tumours show Bcl-2 expression [2]. A recent study has shown Bcl-2 expression in thyroid carcinoma showing thymus like elements [23]. We observed Bcl-2 expression in 88.9% of FTC and 40% of ATC cases; the ATC group showed significant downregulation (Fisher-Exact test, p-value=0.001), as compared to well differentiated thyroid carcinoma (FTC, PTC, MTC) group.
Bcl-2 and Tg are co-expressed in majority of well differentiated thyroid carcinomas with follicular differentiation, and are downregulated in poorly differentiated and undifferentiated carcinomas [24], and in coexisting adjacent ATC [25]. Tg is a marker of thyroid follicular epithelial origin, expressed in FTC and PTC and is reduced or absent in ATC [11,17,18,25,26].
In our study, Tg expression was downregulated in ATC as compared to FTC, PTC subgroup (p-value=0.016). We feel that Tg may be expressed in differentiated areas of thyroid tumours of follicular origin and its expression is gradually reduced with de-differentiation; resulting in variable intensity, and further loss of antigen in ATC. Furthermore, we observed that Bcl-2 and Tg were co-expressed in 95.45% of well differentiated thyroid tumours of follicular origin (FTC, PTC) and none of the ATC, although each of these markers was expressed separately in some of ATC cases. Thus, ATC showed significant downregulation of Tg and Bcl-2. Expression of Bcl-2 is related inversely to loss of differentiation as well as neoplastic progression [24], and its loss may be associated with reduced survival and worse prognosis [3,27].
Bcl-2 was observed in 83.33% of MTC cases. These results are similar to Vialle et al., [27]. The dysregulation of apoptosis may be an important step during oncogenesis of MTC. Also, the indolent growth pattern of MTC may be brought about by Bcl-2 [28]. In the present study, all cases of MTC were positive for both CEA and Cal, with variable intensity, as reported previously [17,18]. MTC can show varied morphology and a panel of markers including Cal and CEA is useful for diagnosis. We noted a positive correlation between Bcl-2 and Cal expression (correlation co-efficient = 0.93) and Bcl-2 and CEA expression (correlation co-efficient = 0.89) in medullary carcinoma.
We feel that Bcl-2 plays an important role in thyroid carcinogenesis. Loss of Bcl-2 was associated with loss of differentiation in thyroid tumours. That may explain its correlation with differentiation associated tumour antigens, namely Tg in follicular derived lesions and Cal and CEA in MTC. ATC as such is associated with worse prognosis and loss of Bcl-2 may be partly responsible. However, more evidence is required to know its exact prognostic value.
p63 a p53-homologue, has been demonstrated in the basal cells of epidermis, ectocervix, urothelium and prostate acini and ducts. The p63 gene encodes transcriptionally active TAp63 isoforms and N-terminally truncated dominant negative isoforms; both may play a role in thyroid tumour progression [9]. It is expressed in a proportion PTC [5–7], including areas of squamous differentiation and scattered tumour cells near the basement membrane [5]. It is specific but less sensitive for PTC. p63 is negative in normal follicular epithelium and follicular neplasms [29]. p63 expression has also been recently observed in thyroid carcinoma with thymus like elements [23]. p63 is expressed in a large proportion of hashimoto’s thyroiditis, which may possibly share a pathobiological relationship with PTC [8]. The p63 expression has been observed in main cells of solid cell nests [9]. The p63 positive pluripotent embryonal remnants may mature, remain undifferentiated, transform to papillary carcinoma or lead to immune reaction and lymphocytic infiltration leading to Hashimoto’s thyroiditis [30].
There was nuclear expression of p63 in 46.15% of our PTC cases and none of the other tumour subtypes, with average percentage of cells staining positive 21.08 ± 10.10. Interestingly in one case, p63 was expressed in the cytoplasm of tumour cells (not taken as positive); the adjacent normal thyroid did not show any staining. This could possibly be due to leakage of nuclear antigens in the cytoplasm. We found p63 to be a specific but less sensitive marker for PTC.
Limitations
The main limitations encountered in our study were cystic aspirate and low cellularity in cytology smears which led to false negative diagnosis. Follicular lesions and Follicular variant of papillary carcinoma were also difficult to subtype on FNAC.
Conclusion
FNAC is fairly accurate for diagnosing thyroid malignancy, and immunocytochemistry adds to the diagnostic value. Loss of Bcl-2 expression is associated with loss of differentiation in thyroid tumours and it may have a role in thyroid carcinogenesis. Bcl-2 is significantly downregulated in anaplastic carcinoma as compared to well differentiated thyroid carcinoma, and shows correlation with differentiation associated tumour antigens, including Tg, Cal and CEA. Loss of Bcl-2 may be partly responsible for poor prognosis associated with ATC. p63 is a specific but less sensitive marker for PTC. Further, studies are required to determine the role of Bcl-2 and p63 in thyroid tumours.
CPTC: Classical Papillary Thyroid Carcinoma, FTC: Follicular Thyroid Carcinoma, FV-PTC: Follicular Variant of Papillary Carcinoma Thyroid, MTC: Medullary Carcinoma, ATC: Anaplastic Carcinoma
SI: Staining Intensity, WDTC: Well Differentiated Thyroid Carcinomas, FTC: Follicular Thyroid Carcinoma, MTC: Medullary Carcinoma, ATC: Anaplastic Carcinoma, PTC: Papillary Carcinoma