Tracheobronchial Injury caused by Blunt Trauma: Case Report and Review of Literature
Vandana Pandey1, Dharam S Meena2, Swati Choraria3, Sushil Guria4
1 Senior Resident, Department of Anaesthesia and Critical Care, AIIMS, Bhopal, India.
2 Professor, Department of Anaesthesia and Critical Care, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India.
3 Senior Resident, Department of Anaesthesia and Critical Care, MAMC, Delhi, India.
4 Assistant Professor, Department of Anaesthesia and Critical Care, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vandana Pandey, B79, Rajved colony, Nayapura, Kolar road, Bhopal- 462042, India.
E-mail: pandeyvandana92@gmail.com
Tracheobronchial injuries are rare cases requiring skillful airway management. We report a challenging case of tracheobronchial injury in a young adult who was run over by a tractor and was referred to us from a peripheral hospital with endotracheal tube in situ. He was severely hypoxaemic on initial presentation. Diagnostic work up showed high suspicion for right bronchial transection along with left lung upper lobe contusion. Due to deteriorating clinical condition of the patient and despite immediate unavailability of fibreoptic bronchoscope, patient was immediately taken up for right posterolateral thoracotomy and double lumen tube was inserted. The position of the tube was confirmed clinically. As soon as the fibreoptic bronchoscope arrived, it was again used to confirm the position of double lumen tube. Patient’s clinical condition improved after repair of the injured right bronchus and he was later extubated the next day.
Blunt trauma chest, Fibreoptic bronchoscope, Thoracotomy
Case Report
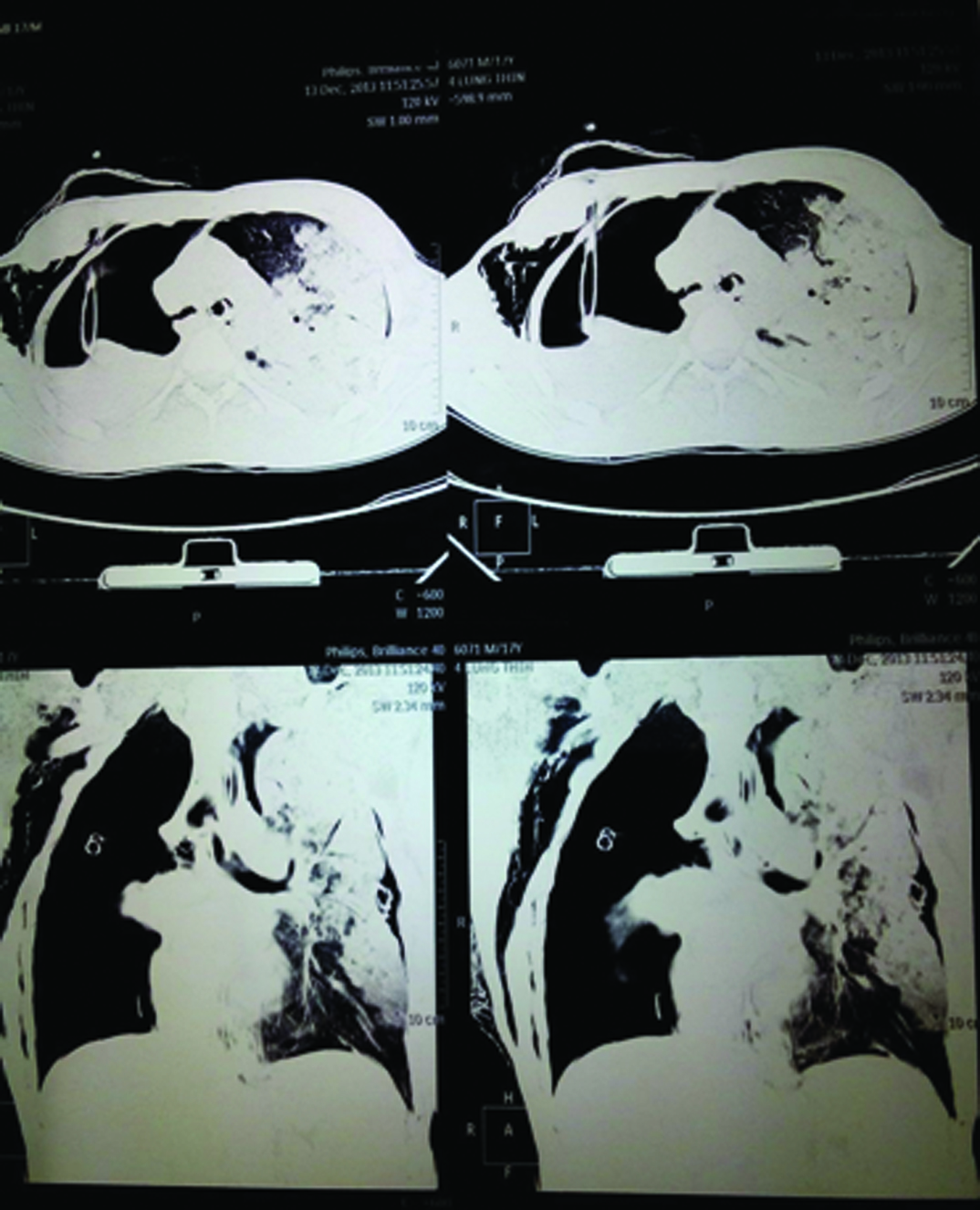
A 17-year-old male patient was admitted to our hospital with history of blunt trauma over chest (run over by a tractor). Patient was first attended at a peripheral hospital where he was intubated with single lumen endotracheal tube 8.0mm oral, cuffed and given assisted mechanical ventilation. Intercostal drain was put on right side of chest. On admission at our hospital, patient was dyspnoeic, with endotracheal tube in situ, tachycardic, hypotensive, and with Glasgow coma score of 10. Chest examination showed poor air entry on the right side despite presence of intercostal drain. Surgical emphysema was present over the right side of chest. Chest X-ray revealed collapsed right lung [Table/Fig-1]. An urgent computerized tomography scan was done that showed large pneumothorax on right side causing complete collapse of right lung parenchyma and communication with right main bronchus contusion of the left upper lobe was also seen [Table/Fig-2]. Patient was planned for immediate thoracotomy with an informed high risk consent and cardiopulmonary bypass kept on standby. Patient was shifted to the operation theatre with endotracheal tube in situ after thorough endotracheal suctioning. Preoperative vitals were severely compromised with a pulse rate of 144/min, blood pressure 63/48mmHg, oxygen saturation 50% on 100% inspired oxygen, respiratory rate 40/min. Patient was given 1 litre of crystalloids and vasopressor was started (dopamine@3-5 microgram/kg/min). The blood pressure increased to 94/49mmHg. Pre-operative arterial blood gas analysis showed-pH—7.20, PaO2-30.7, PaCo2-85.6, HCO3-32.6, base excess-2.4mmol/l, SaO2-45%. Patient was premedicated with fentanyl and then induced with etomidate and succinylcholine. Endotracheal tube was removed and left sided #39F double lumen tube was inserted. Left endobronchial intubation was confirmed clinically by auscultation as paediatric fibreoptic bronchoscope was immediately unavailable and left lung ventilation was achieved. Subsequently saturation improved to 60%. By that time fibrescope arrived and tube position was confirmed. For maintenance of anaesthesia, 100% O2 with isoflurane and vecuronium was used. Patient was placed in left lateral position for thoracotomy. After primary closure of the bronchial stump was done, two lung ventilation was resumed. There was no air leakage through the anastomosis site at positive pressure of 30cm H2O. Arterial blood gases after bronchial repair showed markedly improved oxygenation with PaO2-200, SaO2-99.6%, PaCO2-65.9 and pH-7.23. At the end of surgery, double lumen tube was removed and a conventional endotracheal tube 8.5 mm cuffed was inserted orally. Patient was shifted to intensive care unit for elective postoperative ventilation and was successfully extubated the next day. Postoperative chest x-ray showed complete inflation of right lung. Rest of the recovery was uneventful.
Chest X ray showing collapse of right lung.

CT scan showing right sided pneumothorax with complete collapse of right lung parenchyma.
Discussion
Tracheobronchial Injuries (TBI) occurring after blunt chest trauma is a rare scenario which requires skilful handling of airway. The reported incidence in literature is less than 1% [1]. Most of the patients die at the site of injury due to major airway trauma. It is associated with a high mortality rate of 30% and early intervention is the key to survival [2]. We report a case of TBI with severe hypoxaemia referred to a tertiary care hospital and its successful anaesthetic management with use of double lumen tube despite immediate unavailability of Fibreoptic Bronchoscope (FOB).
An injury occurring between the cricoid cartilage and the division of lobar bronchi into their segmental branches is classified as a TBI [3]. It may occur due to trauma (blunt or penetrating), iatrogenically, due to inhalation of toxic fumes or due to aspiration. Lack of a skin wound in blunt trauma makes the recognition and diagnosis of TBI difficult. The severity of injury due to major airway involvement and rapid progression to life threatening hypoxaemia presents a challenging scenario to the anaesthesiologist [4].
The mechanism of TBI due to blunt trauma can be classified into three types-explosive rupture of tissues due to reflex closure of glottis, due to development of shearing forces at the cricoid cartilage and carina and thirdly, due to chest compression along antero-posterior axis leading to tensile force development causing laceration at the level of carina [5].
In the present case, the patient had right bronchus injury probably due to chest compression. The right bronchus injuries are more common because it is shorter, supports the heavier right lung and there are less supporting structures than the left bronchus which is fixed to major blood vessels [6].
The clinical features are non-specific and can vary from dyspnoea, cough, cyanosis, surgical emphysema to stridor, haemoptysis, mediastinal emphysema or pneumothorax [7]. A massive air leak and the inability to re-expand the lung after tube thoracotomy are highly indicative of a TBI which was also seen in our patient [3]. Hypoxaemia is shown not to be a poor prognostic factor for TBI [8]. Our patient was severely hypoxaemic at initial presentation but recovered after prompt surgical intervention.
The initial investigation of choice is chest X-ray which can show nonspecific findings of pneumothorax, pneumomediastinum and surgical emphysema. Computed tomography is done in haemodynamically stable patients and has 85% sensitivity of detecting airway lesions [9]. It may show mediastinal air, separation in the tracheobronchial air column, respiratory tract deviation or specific location of the separation [10]. The simultaneous presence of pneumomediastinum and cervical emphysema appears to be the most frequent association [9]. Definitive diagnosis is made by bronchoscopy which shows site, nature and extent of injury. Bronchoscopy requires expertise and is not always and readily available in emergency situations. As our patient was referred from a peripheral centre with endotracheal tube in situ, rigid bronchoscopy could not be done. Flexible bronchoscopy is the fastest diagnostic technique in the hands of an expert anaesthesiologist.
The management of TBI can be operative or non- operative. Patients with stable haemodynamics, small lacerations <4cm, not involving all layers, with cuff positioned below the level of injury and with no other major associated injuries are managed conservatively [10]. Our patient was severely hypoxaemic despite being mechanically ventilated and so was taken up for surgery.
The American Society of Anaesthesiologists modified algorithm for airway disruption emphasizes on awake fibreoptic intubation, or rapid sequence intubation using video assisted laryngoscope in uncooperative patients, lung separation using double lumen tube or bronchial blocker and avoidance of positive pressure ventilation [11]. Maintenance of spontaneous ventilation is a key point in the algorithm. Since our patient was already intubated but on spontaneous respiration and was haemodynamically unstable with severe hypoxaemia, a decision to shift him to the operation theatre was made. Thereafter, patient was induced with cardiostable etomidate and succinylcholine was used as it is a short acting muscle relaxant. The in situ single lumen endotracheal tube was carefully removed after deflating the cuff. Left sided double lumen tube was used for lung separation and position of the tube was checked twice by two senior anaesthesiologist clinically as paediatric fibrescope was not available immediately. This also emphasizes on thorough clinical knowledge about double lumen tubes. By that time, the fibreoptic bronchoscope arrived and it was used to check the position of the double lumen tube. Oxygen saturation after double lumen tube placement improved only upto 60% as the left lung was also contused, but improved dramatically to 99% once repair was done. Cardiopulmonary bypass was kept on standby but unless associated with any major vessel injury, the need to put patient on bypass rarely arises [10].
The surgical approach depends on the site of injury. Right posterolateral thoracotomy is the best approach to access the carina, lower part of intrathoracic trachea, right mainstem bronchus and proximal 2 cm of the left bronchus [3]. Our patient underwent right posterolateral thoracotomy through fourth intercostal space and end to end anastomosis of devitalized tissue was done after which two lung ventilation was resumed.
Conclusion
To conclude our case report stresses on prompt recognition of TBI and its quick and successful management despite severe hypoxaemia at presentation. Through this case report we also wish to increase awareness about these life threatening injuries and stress on provision of fibreoptic bronchoscope in all sizes in emergency department as an indispensable aid to diagnosis of TBI. Even if fibreoptic bronchoscope is not immediately available, thorough clinical knowledge and decision in close collaboration with the surgeon can go a long way in saving patients with TBI.
[1]. Devitt JH, Boulanger BR, Lower airway injuries and anaesthesiaCan J anesth 1996 43:148-59. [Google Scholar]
[2]. Nishiumi N, Inokuchi S, Oiwa K, Masuda R, Iwazaki M, Inoue H, Diagnosis and treatment of deep pulmonary laceration with intrathoracic haemorrhage from blunt traumaAnn Thorac Surg 2010 89:232-38. [Google Scholar]
[3]. Gabor S, Renner H, Pinter H, Sankin O, Maier A, Tomaselli F, Indications for surgery in tracheobronchial rupturesEur J Cardiothorac Surg 2001 20:399-404. [Google Scholar]
[4]. Dong Ye, Zhisen Shen, Yuyuan Zhang, Shijie Qiu, Cheng Kang, Clinical features and management of closed injury of the cervical trachea due to blunt traumaScand J Trauma Resusc Emerg Med 2013 21:60 [Google Scholar]
[5]. Kiser AC, O’Brien SM, Detterbeck FC, Blunt tracheobronchial injuries:treatment and outcomesAnn Thorac Surg 2001 71:2059-65. [Google Scholar]
[6]. Kirsh MM, Orringer MB, Behrendt DM, Management of tracheobronchial disruption secondary to nonpenetrating traumaAnn Thorac Surg 1976 22:93-101. [Google Scholar]
[7]. Sengupta S, Saikia A, Ramasubban S, Gupta S, Maitra S, Rudra A, Anaesthetic management of a patient with complete tracheal rupture following blunt chest traumaAnn Card Anaesth 2008 11:123-26. [Google Scholar]
[8]. Nishiumi N, Maitani F, Tsurumi T, Kaga K, Iwasaki M, Inoue H, Blunt chest trauma with deep pulmonary lacerationAnn Thorac Surg 2001 71:314-18. [Google Scholar]
[9]. Chen JD, Shanmuganathan K, Mirvis SE, Killeen KL, Dutton RP, Using CT to diagnose tracheal ruptureAJR Am J Roentgenol 2001 176:1273-80. [Google Scholar]
[10]. Altinok T, Can A, Management of tracheobronchial injuryEurasian J Med 2014 46:209-15. [Google Scholar]
[11]. American Society of AnesthesiologistsASA difficult airway algorithm modified for traumaASA Newsllet 2005 69:9-16. [Google Scholar]