Unusual Presentation of Pigmented Basal Cell Carcinoma of Face: Surgical Challenge
Ravleen Nagi1, Shashikant Sahu2, Nitin Agarwal3
1 Senior Lecturer, Department of Oral Medicine and Radiology, New Horizon Dental College and Research Institute, Bilaspur, Chhattisgarh, India.
2 Consultant, Plastic and Cosmetic Surgeon, Department of Plastic Surgery, Burn and Trauma Centre, Bilaspur, Chhattisgarh, India.
3 Pathologist, Department of General Pathology, Nishkarsh Pathology Clinic, Bilaspur, Chhattisgarh, India
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ravleen Nagi, Senior Lecturer, Department of Oral Medicine and Radiology, New Horizon Dental College and Research Institute, Sakri, Bilaspur, Chhattisgarh, India.
E-mail: ravleennagi@yahoo.in
Clinical variants, Melanoma, Treatment
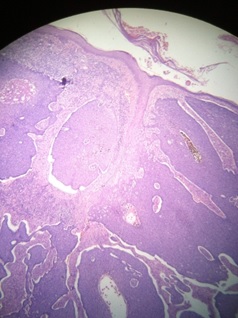
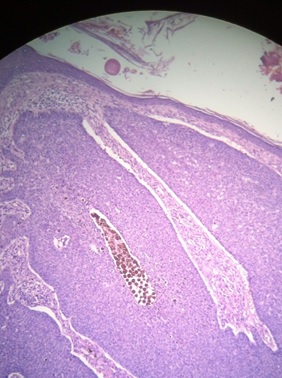
A 55-year-old man reported with the chief complaint of black pigmented mass on right side of the face. The patient initially noticed the lesion two years back, gradually increasing in size. Patient’s family and medical history was non-contributory. Personal history revealed that he smoked one packet of bidi per day since 20 years. Patient was a farmer by occupation. On extra oral examination, irregular rectangular dark brown mass was present on right side of the face extending medially up to the lateral wall of nose and superiorly up to the infra-orbital region 5mm below the lower eyelid, and medially the mass was extending up to the medial canthus of right eye measuring around 5 X 4cm in size with well defined borders [Table/Fig-1]. On palpation, it was non-tender, non-fixed, non indurated and firm in consistency. Adjacent skin was normal with no lymphadenopathy. Based on history and clinical examination, provisional diagnosis of Basal Cell Carcinoma (BCC) was given. An incisional biopsy was done, and specimen was sent for Histopathological Examination (HPE) [Table/Fig-2]. The lesion was excised with wide local resection with 4-5 mm lateral and deep margins under general anesthesia and the raw area created was covered by Limberg Flap [Table/Fig-3,4]. Patient was followed up after 10 days and the flap was found healthy [Table/Fig-5]. Specimen was sent for HPE which revealed Pigmented BCC (PBCC) [Table/Fig-6].
The black pigmented lesion on the right side of the cheek which was well defined, non-tender, non-fixed, and firm on palpation.

Pigmented basal cell carcinoma showing nodular sheets with retraction artifacts H&E (X40).
Wide local surgical resection of pigmented basal cell carcinoma.

Raw area was covered with Limberg flap.

Postoperative follow up photograph of patient showed well healed flap.

Pigmented basal cell carcinoma showing pigmentation H&E (X100).
Discussion
BCC is the most common type of skin cancer with high incidence rates in whites as compared to Indians. It is more common in men than women and is more common in middle aged people or elderly [1]. It is most commonly seen on middle third of the face, but lesions could be seen anywhere on the sun exposed parts of the skin [2]. Prolonged exposure to ultraviolet radiation is the main cause of development of BCC. Our patient belonged to fifth decade and presented with pigmented dark brown mass on middle third of the face. There was no local destruction or jaw involvement associated with the lesion. He was farmer by occupation and routine exposure to sunlight may be the cause of development of BCC. Occurrence of BCC at an early age is a feature of Xeroderma Pigmentosum and Nevoid BCC Syndrome [1].
There are several variants of BCC based on clinical appearance and aggressiveness: nodular, pigmented, sclerosing, superficial and basosquamous. Pigmented BCC (PBCC) is a rare variant (6%) consists of dark brown or black melanin pigmentation. Clinically it presents as a well defined papule or nodule over sun exposed parts of skin and is slow growing, locally invasive, rarely metastasizes. Differential diagnosis of PBCC mainly includes malignant melanoma and seborrhic keratosis [3]. They can be differentiated by histopathological examination. In our patient, incisional biopsy was done from the lower aspect of the lesion and histopatholgical examination revealed nodular sheets of cells, basal palisading pattern of cells with abundance of melanin and increased mitotic activity. Histopathlogically, seborrheic keratosis has a wide variety of histologic appearances such as acanthotic, hyperkeratotic, clonal, reticulated, irritated, and pigmented. Pigmented type can be confused with PBCC, in which pigment is present in basal keratinocytes with marked increase in melanocytes. In contrast, malignant cells of malignant melanoma histopathologically reveals wide range of shapes such as spindle cell, plasmacytoid, clear cell, and epitheloid ones with considerable pleomorphism, nuclear hyperchromatism and abnormal mitotic activity [3].
Although BCC is not a lethal malignancy, if left untreated, it can result in severe destruction and disfigurement. It is necessary to treat it as early as possible to prevent complications due to its aggressive behavior [4]. There are many treatment options available for PBCC such as surgical excision, electric cauterization and curettage, cryotherapy, radiotherapy, laser therapy, chemical destruction of the tumor with 5 fluorouracil, interferon-α, topical imiqimod and photodynamic therapy. Surgical excision is the treatment of choice and widely employed therapeutic method [3]. Tumors with diameter above 2cm or with unclear borders or with aggressive histological signs (infiltrative, morphologic and peri-neural infiltration) are indicated for Mohs microscopic surgery [5]. In our patient local wide surgical resection with 4-5mm margins was done and raw area was covered by Limberg flap. We preferred surgical excision as the primary line of treatment in our case which was compatible to the study by Sebastian et al., [6]. Periodic evaluation of such patients is necessary to prevent recurrences. Properly excised BCC has fewer chances of recurrences. PBCC shows lesser subclinical infiltration than nonpigmented one, and thus have a better prognosis [2]. In the present case after initial 10 days follow-up, flap was found healthy and no recurrence of the tumor was reported. Patient was on regular follow-up for evaluation of tumor site.
In conclusion, timely diagnosis and early treatment of BCC leads to better prognosis of patients. PBCC is rare variety which is a diagnostic challenge to clinicians as it mimics other black pigmented lesions especially malignant melanoma. Knowledge of histopathological and cytological features of PBCC and its differentials will help in exact diagnosis and treatment of this condition.
[1]. Mozaffary PM, Delavarian Z, Amirchaghmaghi M, Dalirsani Z, Mostaan LV, Khadem SS, Secondary involvement of the mandible due to basal cell carcinoma: a case reportIran J Med Sci 2015 40:277-81. [Google Scholar]
[2]. Janjua OS, Qureshi SM, Basal cell carcinoma of head and neck region: an analysis of 171 casesJ Skin Cancer 2012 :1-4. [Google Scholar]
[3]. Dourmishev LA, Rusinova D, Botev I, Clinical variants, stages, and management of basal cell carcinomaIndian Dermatol Online J 2013 4:12-17. [Google Scholar]
[4]. Rishiraj B, Epstein JB, Basal cell carcinoma: what dentists need to know?J Am Dent Assoc 1999 130:375-80. [Google Scholar]
[5]. Silverman MK, Kopf AW, Bart RS, Grin CM, Levenstein MS, Recurrence rates of treated basal cell carcinomas. Part 3: Surgical excisionJ Dermatol Surg Oncol 1992 18:471-76. [Google Scholar]
[6]. Sebastian Villalon-Lopez J, Arturo Valle-Mejia C, Patino-Lara A, Moreno-Perez Bertha A, Alejo Munoz-Lopez J, Alcantar-Andrade A, Supraestructure maxillectomy and orbital exenteration for treatment of basal cell carcinoma of inferior eyelid: case report and reviewJ Cancer Res Ther 2005 1:132-35. [Google Scholar]