Broad Ligament Pregnancy – Success Story of a Laparoscopically Managed Case
Jayashree Nayar1, Sobha S. Nair2
1 Professor, Department of Obstetrics and Gynaecology, Amrita Institute of Medical Science and Research Center, Kochi, Kerala, India.
2 Assistant Professor, Department of Obstetrics and Gynaecology, Amrita Institute of Medical Science and Research Center, Kochi, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jayashree Nayar, 22-Neptune Country, Chilavanoor, Kadavanthra, Kochi-682020, Kerala, India.
E-mail: jshr2008@gmail.com
Abdominal pregnancies constitute 1% of ectopic pregnancies, among which broad ligament pregnancy is a rare form. The maternal mortality rate has been reported to be as high as 20%. The diagnosis is seldom established before surgery. Laparoscopic management of broad ligament ectopic pregnancy is the ideal form of treatment in appropriately selected patients.
We present the case report of successful laparoscopic treatment of a 3x3.5cm broad ligament pregnancy. A search of literature shows that ours is the 6th case report of such a rare ectopic pregnancy managed endoscopically successfully.
Abdominal pregnancy, Ectopic pregnancy, Endoscopic surgery, Intra ligamentary pregnancy
Case Report
A 25-year-old woman presented to our out-patient department with history of 6 weeks amenorrhoea and with complaints of 1 episode of spotting per vaginum, mild intermittent abdominal pain, predominantly in the umbilical region and nausea since 1 day. She was a primigravida and a known case of hypothyroidism, on hormone replacement since 2 years. She was haemodynamically stable. On per abdominal examination there was minimal tenderness and no mass was palpable. Per speculum examination revealed minimal blood stained discharge through the os. There was no mass palpable in both fornices or cervical motion tenderness, with the uterus being of normal size and anteverted on vaginal examination. Laboratory investigations showed urine pregnancy test was positive and Serum BHCG measured 24,719mIU/ml. Her haemogram was normal.
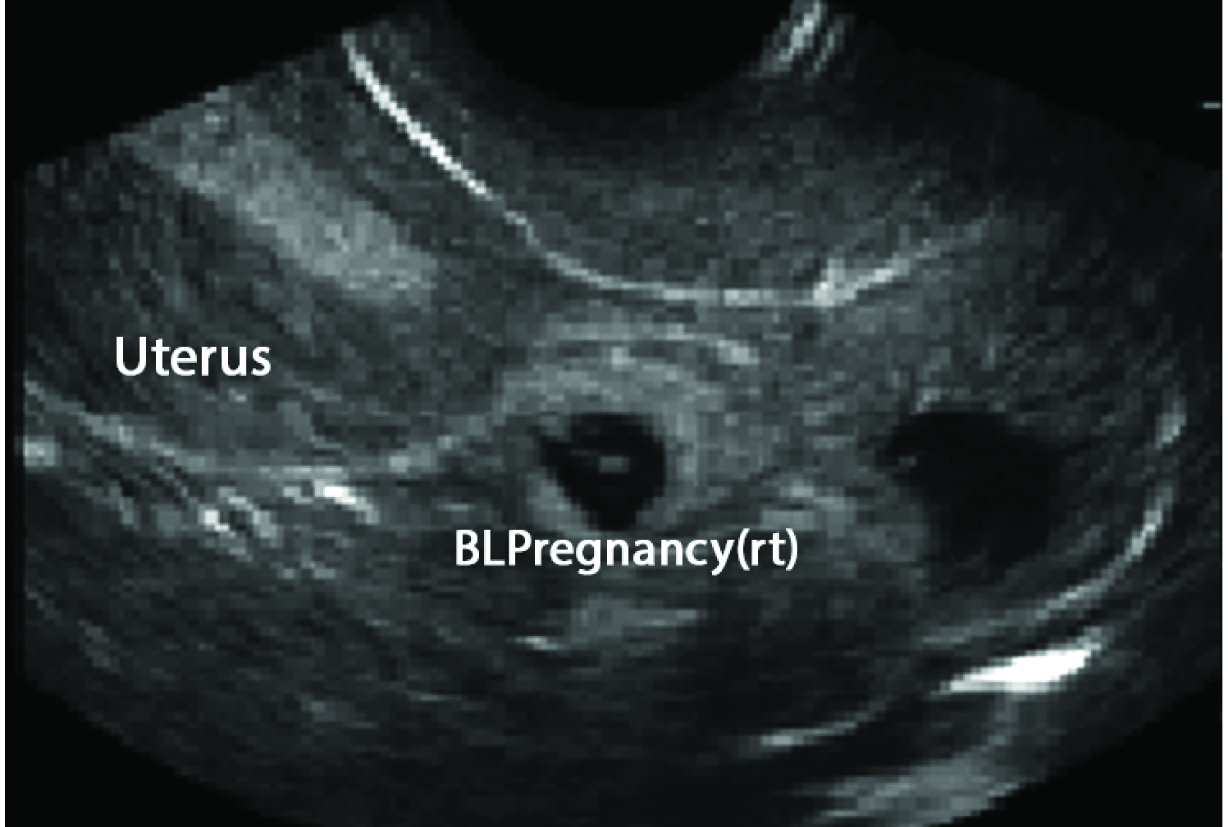
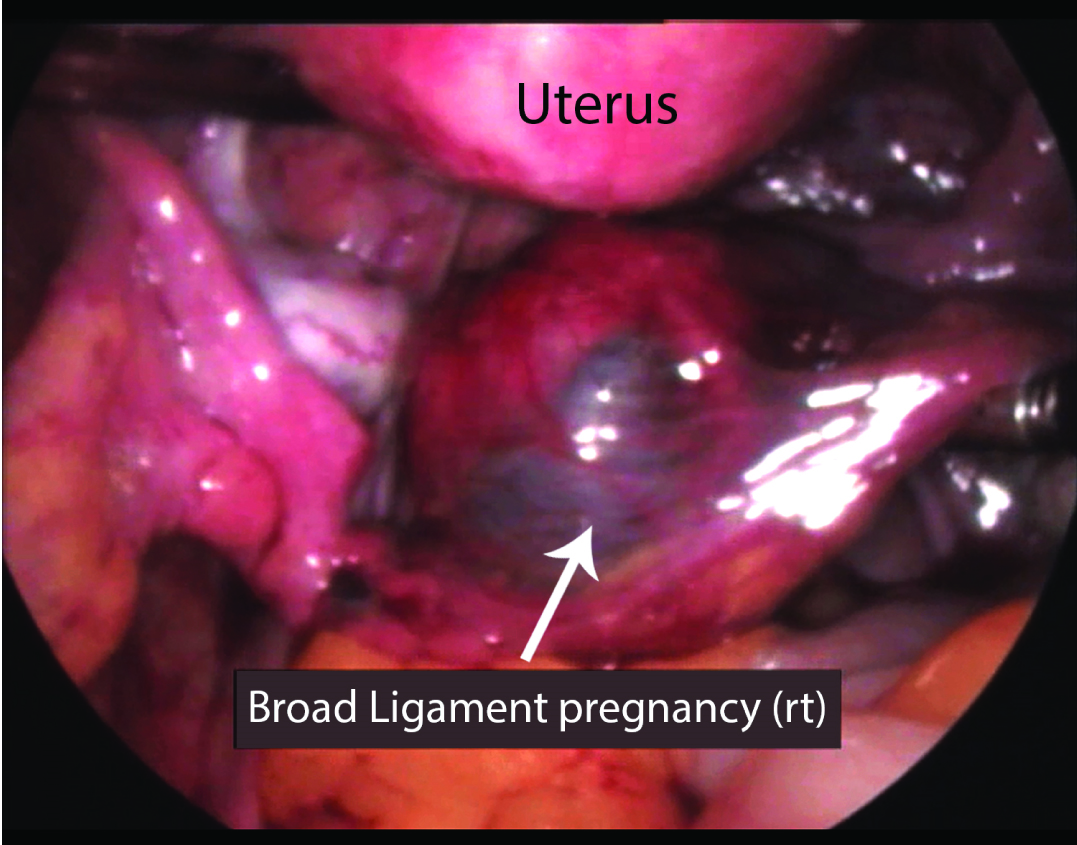
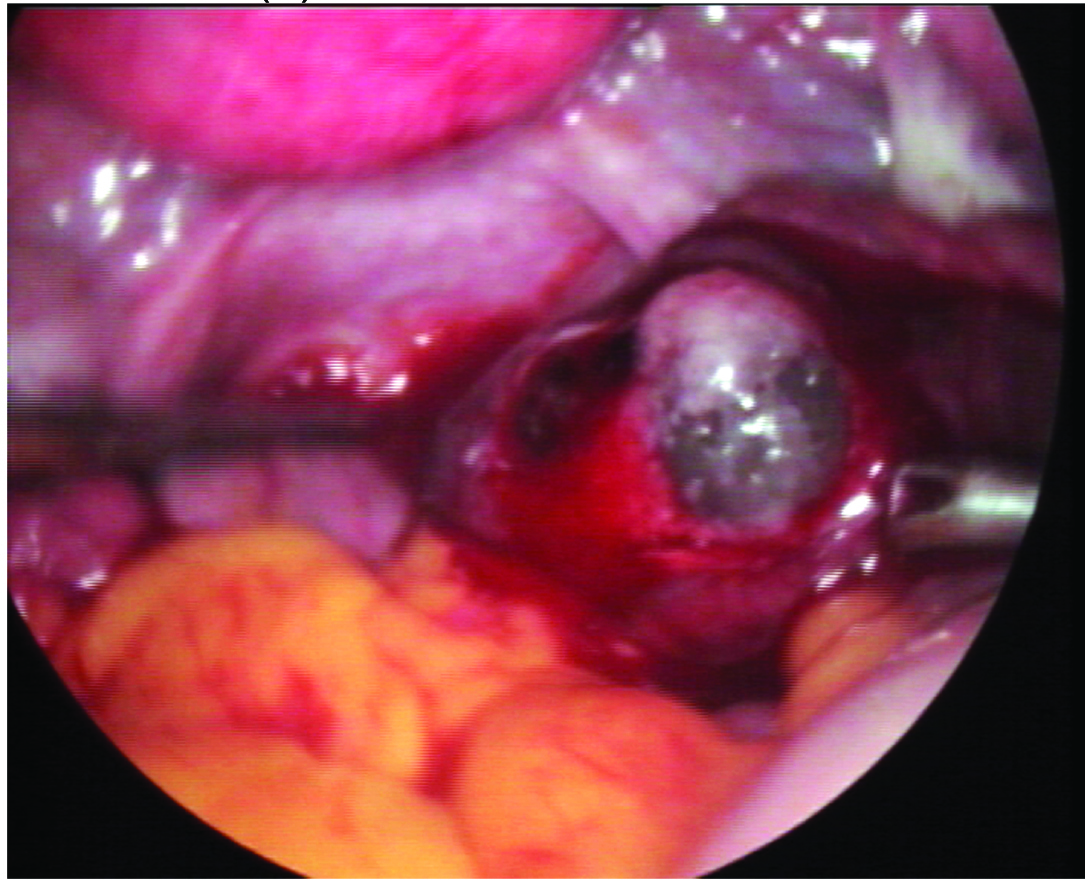
Trans vaginal ultrasonography revealed an empty uterus with a 3x3.5cm right adnexal mass containing a foetal pole of 7 weeks gestation [Table/Fig-1]. Foetal cardiac activity was noted and there was no free fluid in the cul de sac. Since the patient was stable and the findings suggested unruptured tubal pregnancy. Laparoscopy was undertaken after relevant preparation. A 3x3.5cm abdominal pregnancy [Table/Fig-2,3] was found in the right broad ligament with minimal blood in the cul de sac. The right tube, uterus, left adnexa appeared normal. The rest of the viscera were normal. The right broad ligament was opened and the sac was excised, products of conception extruded. There was excess bleeding from the site, which could not be controlled by cauterisation of the vessels and ultimately resulted in right salpingectomy.
Ultra sound picture right ectopic pregnancy.
Intra operative findings at laproscopy.
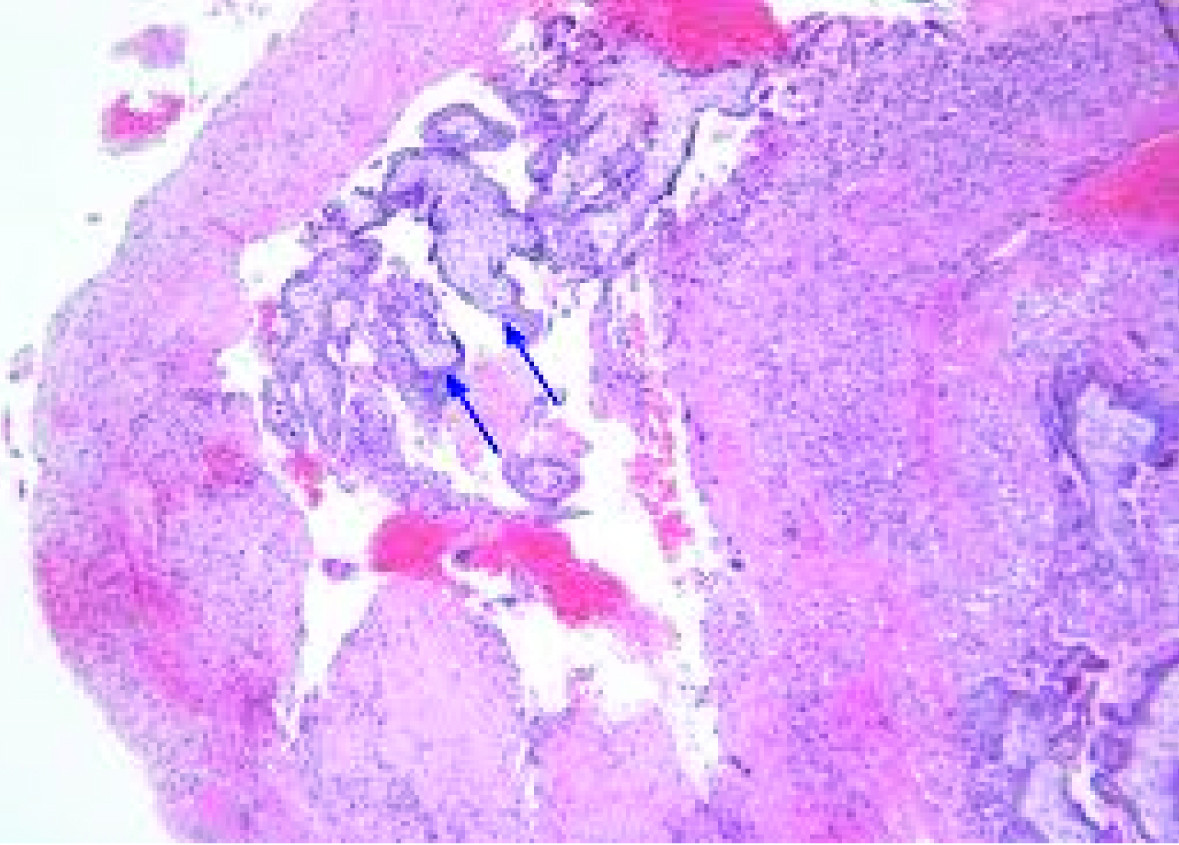
Histopathological report showed the presence of chorionic villi interspersed with blood vessels within the sac space, which confirmed this as an ectopic pregnancy from the broad ligament [Table/Fig-4].
Histo pathology slide confirming diagnosis.
She had no postoperative complications but was lost to follow-up after the initial postoperative checkup at 6 weeks.
Discussion
Abdominal pregnancy is one, that is implanted in the peritoneal cavity, outside the uterine cavity and the fallopian tubes. It is estimated to be 1% of ectopic pregnancies [1,2] and the incidence is about 1 in 10,000 births. Rarely abdominal pregnancy occurs after hysterectomy [3,4].
Broad ligament, omentum, pelvic sidewall, posterior cul-de-sac, abdominal organs (e.g., spleen, bowel, liver), large pelvic vessels, diaphragm, and the uterine serosa are potential sites [2,4].
Today it is possible for us to arrive at a confirmed diagnosis of Ectopic pregnancy with the help of high resolution transvaginal sonography combined with serum Beta HCG, resulting in a sensitivity of 93% and a specificity of 99%. However, a preoperative diagnosis of broad ligament pregnancy is very rare.
Broad ligament ectopic pregnancy was first described in 1816 by Loschge [5]. Champion and Tessitore [6] summarised the largest series of 62 cases and reported the incidence as one in 183,900 pregnancies. They also stated the required anatomical relationships to diagnose a broad ligament ectopic pregnancy, namely: location of the uterus medially, the pelvic side walls laterally, the pelvic floor inferiorly and the fallopian tube superiorly. These were exactly the boundaries of the ectopic pregnancy in our case.
In most cases of abdominal pregnancies, the choice of surgical management is via laparotomy because of the high risk of massive intraoperative haemorrhage. Laparoscopic management of abdominal pregnancies at unusual sites, such as the uterovesical fold and caesarean section scar, has been described with the advantages of less blood loss and lower surgical morbidity/mortality and faster recovery.
On a thorough search using Medline and Keywords–broad ligament pregnancy/laparoscopy/successful management, we could find only 5 other cases of a broad ligament pregnancy successfully managed laparoscopically of varying sac size ranging from 1cm to 6.5cm [7–12].
To our knowledge, this is the 6th successful laparoscopic management of such an abdominal pregnancy in the broad ligament. In some of the cases mentioned in literature, laparoscopy was abandoned and laparotomy or even hysterectomy resorted to.
The tabular description of the six successful cases of broad ligament pregnancy [including this case] managed successfully by laparoscopy [Table/Fig-5].
Showing time of report and significant features of each case
| Study (Year) | Age,y | Parity | Risk Factors | Gestational Age (wk) | Presentation | hCG (IU/L) | Imaging Findings (USG if Not Specified) | Outcome |
|---|
| 1 | Olsen (1997) [8] | 26 | 1+1 | Not known | 7 | Vaginal spotting | 22,140 | Right adnexal mass | Laparoscopy; right intraligamentary pregnancy <1 cm peritoneal separation; managed with bipolar scissors and scissors and electrocautery. |
| 2 | Siow et al., (2004) [9] | 25 | Unknown | Not known | 10 | Asymptomatic | 55.8 | 5.5-cm right adnexal mass with CRL 8 wk | Laparoscopy; 6.5cm right broad ligament ectopic pregnancy, vasopressin injection and excision. |
| 3 | Apantaku et al., (2006) [10] | 33 | 1+2 | Previous laparotomy and bilateral salpingectomy, IVF pregnancy | 8 | Not mentioned | NA | Empty uterus, right adnexal mass with CRL 6 wk | Laparoscopy; 2cm broad ligament pregnancy below remnant of right tube. |
| 4 | Cormio et al., (2006) [11] | 28 | 0 | Ipsilateral salpingooophrectomy | 10 | Abdominal pain, vaginal bleeding | 35,760 | 5-cm round mass over left adnexal region | Laparoscopy; left broad ligament opened, ectopic pregnancy removed enbloc with part of myometrium. |
| 5 | Cheung CS-y, Cheung VYT 2014 [12] | 30 | 0+1 | Ipsilateral salpingectomy | 6 | Vaginal bleeding | 15,665 | Suspected stump pregnancy, CRL 5 wk 5 d with slow fetal pulsation | Laparoscopy; 3cm unruptured right broad ligament pregnancy; excision and laparoscopic suture to obliterate the space and hemostasis. |
| 6 | Our Case | 25 | 0 | Not known | 6 | Spotting, Intermittent abdominal pain | 24,719 | Empty uterus, rt adnexal mass, 7 weeks fetal pole with cardiac activity | Laparoscopic excision of sac and right salpingectomy. |
Conclusion
Thus with this set up- comprising an efficient team of laparoscopic surgeons and anaesthetists, operative laparoscopy is a safe alternative for the management of appropriately selected patients with early broad ligament pregnancy.
[1]. Atrash HK, Friede A, Hogue CJ, Abdominal pregnancy in the United States: frequency and maternal mortalityObstet Gynecol 1987 69:333 [Google Scholar]
[2]. Fisch B, Peled Y, Kaplan B, Abdominal pregnancy following in vitro fertilization in a patient with previous bilateral salpingectomyObstet Gynecol 1996 88:642 [Google Scholar]
[3]. Binder DS, Thirteen-week abdominal pregnancy after hysterectomyJ Emerg Med 2003 25:159 [Google Scholar]
[4]. Fader AN, Mansuria S, Guido RS, Wiesenfeld HC, A 14-week abdominal pregnancy after total abdominal hysterectomyObstet Gynecol 2007 109:519 [Google Scholar]
[5]. Loschge Arch F Med Erfahr 1818 2:218 [Google Scholar]
[6]. Champion PK, Tessitore NJ, Intraligamentary pregnancy: A survey of all published cases of over 7 calendar months, with the discussion of an additional caseAm J Obstet Gynecol 1938 36:281-93. [Google Scholar]
[7]. Tsudo T, Harada T, Yoshioka H, Terakawa N, Laparoscopic management of early primary abdominal pregnancyObstet Gynecol 1997 90:687-88. [Google Scholar]
[8]. Olsen ME, Laparoscopic treatment of intraligamentous pregnancyObstet Gynecol 1997 89:862 [Google Scholar]
[9]. Siow A, Chern B, Soong Y, Successful laparoscopic treatment of an abdominal pregnancy in the broad ligamentSingapore Med J 2004 45(2):88-89. [Google Scholar]
[10]. Apantaku O, Rana P, Inglis T, Broad ligament ectopic pregnancy following in-vitro fertilisation in a patient with previous bilateral salpingectomyJ Obstet Gynaecol 2006 26(5):474 [Google Scholar]
[11]. Cormio G, Ceci O, Loverro G, Bettocchi S, Spontaneous left broad ligament pregnancy after ipsilateral salpingo-oophorectomyJ Minim Invasive Gynecol 2006 13(2):84-85. [Google Scholar]
[12]. Cheung CS-y, Cheung VYT, Broad ligament ectopic pregnancyCRSLSe 2014 :00102DOI 10 .4293/CRSLS 2014,00102 [Google Scholar]