Periodontal diseases are chronic inflammatory conditions characterized by loss of connective tissue, alveolar bone resorption and formation of periodontal pockets as a result of the complex interaction between pathogenic bacteria and the host’s immune response. Dental plaque is the primary etiologic factor in periodontal disease [1].
The onset or progression of periodontal disease can be controlled by regular and meticulous plaque control measures. Mechanical plaque control is the most dependable oral hygiene practice to maintain proper oral hygiene [2]. Plaque control measures like daily tooth brushing and flossing are not practiced consistently for adequate amount of time and neither they are completely reliable due to various morphological changes of teeth. Thus, demanding the search for other alternatives [3].
Many, chemical anti-plaque agents in various formulations have been tried to improve oral health. [4]. Anti-plaque agents can be delivered in the form of mouthwashes, dentifrices, chewing gums and gels. Recently Chlorhexidine has been a gold standard chemical plaque control agent for its proven clinical efficacy because of its broad antibacterial activity, very low toxicity and strong affinity for epithelial tissue and mucous membranes. It is substantive, which reduce the levels of microorganisms in saliva to a considerable extent however it has some side effects like staining of teeth, alteration in taste and mucosal erosions that could affect patient compliance [3,5]. So the search for an ideal and safe anti-plaque agent continues.
Now-a-days around the world number of people are seeking the benefits from nature by using the natural herbal products in both prophylaxis and cure of different diseases. Plants/Herbs serve the source for a majority of prescriptions for different ailments and hence the potential of natural agents for oral health should therefore be explored [3]. Ayurveda being an age old tradition of medicine is less explored in management of oral diseases. Arimedadi Taila/Oil is one such ayurvedic medicine useful in the treatment of common periodontal problems like bleeding gums, bad breath, swollen gums, mobility of teeth, etc., [6]. Arimedadi Taila/Oil (Irimedadi Taila) is also indicated for oil pulling or gargling and in many Dantarogas including stomatitis, glossitis, apthous ulcers, dental caries, pyorrhea, gingivitis, stain removal and hyperemia of gums [6].
There are reports of Arimedadi Oil usage in oral ailments but much research has not been done to assess its effectiveness on oral health [6]. Therefore, the present study was conducted to assess the anti-plaque efficacy of Arimedadi (herbal) oil against 0.2% Chlorhexidine gluconate mouthwash.
Materials and Methods
The present study was a randomized, double blinded, three-group parallel study conducted at Department of Public Health Dentistry, ACPM Dental College Dhule, Maharashtra, India, for 21 days among 45 patients aged between 18-21 years dental students who fulfilled the eligibility criteria. Patient diagnosed with mild to moderate type of gingivitis, free from systemic illness, having minimum of 20 functional teeth in the oral cavity, not received any periodontal therapy for the past six months and willing to give informed consent were included in the study. Patients wearing fixed or removable orthodontic appliances or prosthesis, on antibiotics or other medications from last 3-6 months, females who were in menstrual period and those who were pregnant or lactating were excluded from the study.
The research protocol was approved by the institutional ethical review committee. Participants were informed about the purpose and design of the investigation and written informed consent was obtained. A total of 45 patients who fulfilled the selection criteria were randomly divided into three groups (15 in each group) by applying simple random sampling technique by employing lottery method [Table/Fig-1].
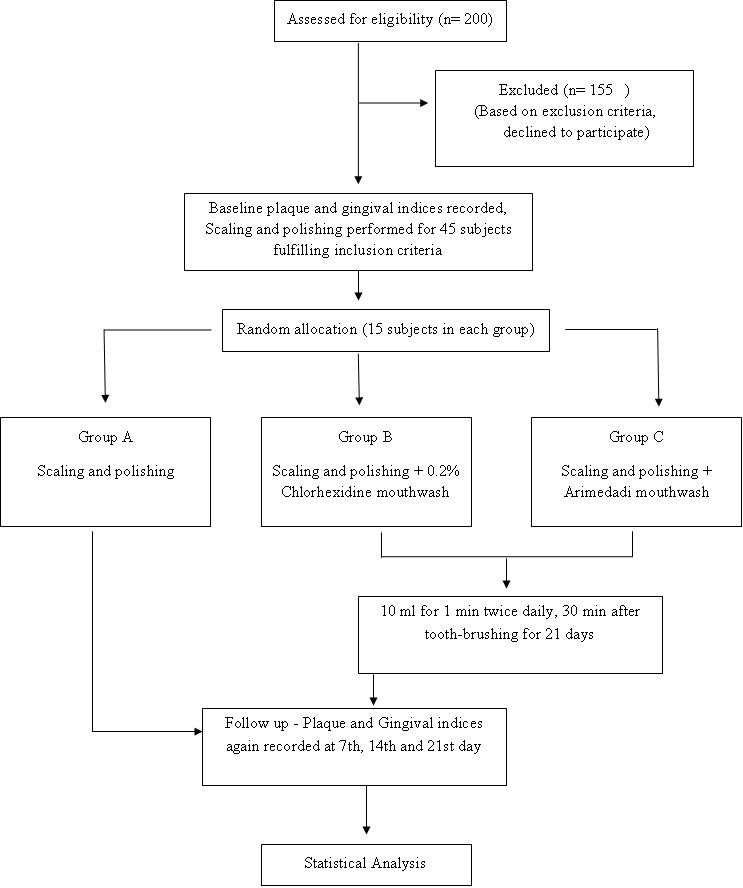
- Group A: Scaling and polishing.
- Group B: Scaling and polishing along with the use of Chlorhexidine mouthwash (0.2%).
- Group C: Scaling and polishing along with the use of Arimedadi mouthwash.
The sample size was determined based on the prevalence of gingivitis/periodontitis in Maharashtra from previous study [7] and by using the Sample Size formula:
n = 4qp/L2
Where q is 95% confidence level, p is prevalence, L is allowable error [7].
Arimedadi Oil
Manufacturer: Ayurveda Sewasangh Panchavati, Nashik.
Composition: Khairchaal, Lavang, Gairic, Agaru, Padmakashtha, Manjishtha, Lodhara, Jeshthamadh, Laksha, Welchi, Wadachi Paane, Nagarmotha, Dalchini, Yashti, Jaiphala, Kapoor, Kankol, Kshudra chandan, Dhayati phoole, Lahan welchi, Nageshar, Til tel [6].
The patients and the examiner who evaluated the effectiveness, were not aware of the type of treatment corresponded to each group. Unicolour (Amber coloured) bottles were used to dispense the mouthwashes and blinding was done while distributing them to the subjects. At baseline, Plaque Index (Silness and Loe, 1964) and Gingival Index (Loe and Silness, 1963) were used to assess the plaque and gingival status. After scaling and polishing of all teeth, oral hygiene instructions were given to all the participants and were distributed with similar toothbrush and toothpaste in an attempt to maintain standardization and improve their oral hygiene. Group A served as control group in which only scaling and polishing was done, Group B were instructed to rinse with 10 ml 0.2% Chlorhexidine mouthwash for 1 min twice daily after 30 min of tooth brushing for 21 days and Group C were instructed to rinse with undiluted 10 ml Arimedadi oil for 1 min twice daily after 30 min of tooth brushing uninterruptedly for 21 days. Subsequent follow up of the patients was done to assess the effect of intervention on gingival health by recording plaque and gingival assessment on 7th day, 14th day and 21st day. Subjects were asked to report immediately if they felt any discomfort in using the mouthwashes during the course of the study.
Statistical Analysis
All statistical procedures were performed using Statistical Package for Social Sciences (SPSS) 20.0 software (IBM, Armonk, NY, United States of America) and the tests applied for data comparison were Paired t- test and ANOVA followed by Post Hoc test.
Results
Intra-group and Inter-group comparison of mean PI, mean GI, mean percentage reduction of PI and GI was done using ANOVA and Bonferroni Post Hoc test. There was an improvement in plaque and gingival health in all the groups from baseline to 7th day (p<0.001) but the improvement was more pronounced in Group B and Group C as compared to Group A. From 7th day till 14th day there was further improvement seen in Group B and Group C as that of Group A (p<0.001). However from 14th day till 21st day there was no difference in gingival health status in between Group B and Group C (p>0.001) moreover the plaque and gingival status further deteriorated in Group A, thus proving the efficacy of Chlorhexidine gluconate and Arimedadi oil as mouthwash in reducing plaque accumulation and improving gingival health as compared to only scaling and polishing [Table/Fig-2,3]. The percentage reduction of PI and GI in Group B and Group C was more from baseline till 21st day as compared to Group A (p<0.001) [Table/Fig-4,5].
Intragroup comparison of plaque index at different interval (baseline, 7days, 14 days & 21 days).
| PI | Group A | Group B | Group C |
|---|
| Baseline | 1.77±0.18 | 1.77±0.18 | 1.76±0.18 |
| 7th day | 1.13±0.14 | 0.89±0.06 | 0.94±0.11 |
| 14th day | 1.24±0.17 | 0.71±0.06 | 0.73±0.09 |
| 21st day | 1.47±0.16 | 0.69±0.06 | 0.71±0.05 |
| ANOVA F-value | 44.746*** | 355.515*** | 273.119*** |
| p-value | p<0.001 | p<0.001 | p<0.001 |
| Baseline Vs 7 days (Paired t-test) | p<0.001 | p<0.001 | p<0.001 |
| Baseline Vs 14 days (Paired t-test) | p<0.001 | p<0.001 | p<0.001 |
| Baseline Vs 21 days (Paired t-test) | p<0.001 | p<0.001 | p<0.001 |
| 7 days Vs 14 days (Paired t-test) | p<0.05 | p<0.001 | p<0.001 |
| 7 days Vs 21 days (Paired t-test) | p<0.001 | p<0.001 | p<0.001 |
| 14days Vs 21 days (Paired t-test) | p<0.001 | p>0.05 | p>0.05 |
p value <0.05 considered statistically significant.
*** The mean difference is very highly significant at the .001 level.
Intragroup comparison of gingival index at different interval (baseline, 7days, 14 days & 21 days).
| GI | Group A | Group B | Group C |
|---|
| Baseline | 1.80±0.15 | 1.82±0.22 | 1.81±0.23 |
| 7th day | 1.22±0.17 | 0.94±0.14 | 0.98±0.11 |
| 14th day | 1.34±0.17 | 0.67±0.07 | 0.67±0.08 |
| 21st day | 1.50±0.09 | 0.66±0.08 | 0.66±0.07 |
| ANOVA F-value | 42.753*** | 231.429*** | 222.060*** |
| p-value | p<0.001 | p<0.001 | p<0.001 |
| Baseline Vs 7 days (Paired t-test) | p<0.001 | p<0.001 | p<0.001 |
| Baseline Vs 14 days (Paired t-test) | p<0.001 | p<0.001 | p<0.001 |
| Baseline Vs 21 days (Paired t-test) | p<0.001 | p<0.001 | p<0.001 |
| 7 days Vs 14 days (Paired t-test) | p<0.05 | p<0.001 | p<0.001 |
| 7 days Vs 21 days (Paired t-test) | p<0.001 | p<0.001 | p<0.001 |
| 14 days Vs 21 days (Paired t-test) | p<0.001 | p>0.05 | p>0.05 |
p-value <0.05 considered statistically significant.
*** The mean difference is very highly significant at the 0.001 level.
Intergroup comparison of percentage reduction of plaque index at different intervals.
| Percent Reduction PI | 7th day | 14th day | 21st day |
|---|
| Group A | 35.15±13.12 | 29.22±13.30 | 16.51±10.24 |
| Group B | 49.18±7.05 | 59.58±5.06 | 60.65±4.14 |
| Group C | 46.21±6.74 | 58.37±5.91 | 59.16±4.52 |
| ANOVA |
| F-value | 9.198 | 56.040 | 198.569 |
| p-value | <0.001 | <0.001 | <0.001 |
p-value <0.05 considered statistically significant.
Intergroup comparison of percentage reduction of gingival index at different intervals (7days, 14 days, 21 days).
| Percent Reduction GI | 7th day | 14th day | 21st day |
|---|
| Group A | 31.72±11.02 | 25.24±11.46 | 16.36±7.00 |
| Group B | 47.73±8.23 | 62.56±7.68 | 63.40±6.50 |
| Group C | 45.38±7.96 | 62.41±6.37 | 63.22±5.30 |
| ANOVA |
| F value | 13.314 | 90.160 | 276.938 |
| P value | <0.001 | <0.001 | <0.001 |
p value <0.05 considered statistically significant.
Discussion
The present study shows that ayurvedic mouthwash (Arimedadi) was equally effective as conventional chlorhexidine mouthwash in reduction of plaque and gingival scores over a period of 21 days usage.
Chemical plaque control is considered to be an adjunct to mechanical oral hygiene practices. Mouth rinses/mouth washes have exhibited their analgesic, anti-inflammatory, and antimicrobial activity when used as an adjunct to mechanical oral hygiene [8]. Chlorhexidine has been regarded as a “gold” standard for the prevention of plaque and gingivitis. Numerous studies have reported the efficacy of Chlorhexidine in reducing plaque accumulation and gingival inflammation [3, 8–10]. However chlorhexidine usage has its own limitations such as brown discoloration of dentition and restorative material, dorsum of the tongue, taste perturbation, oral mucosal ulceration, unilateral/bilateral parotid swelling and enhanced supragingival calculus formation on its long term use [11].
Ayurveda is practiced in India from ancient periods and there are numerous natural plants found which have a great significance in dentistry. Various studies have been conducted exhibiting favorable results of herbal/natural product for management of dental ailments. Different natural plants are used for preparation of mouthwashes such as green tea, turmeric, neem, cranberry, aloe vera, pot marigold; triphala etc., and studies conducted have proved to be effective in reducing plaque accumulation and gingival inflammation [8,10–16]. Ayurvedic medicine, Arimedadi Taila /Oil is less explored to assess its dental health benefits. So the present study assessed and compared the efficacy of Arimedadi oil as mouthwash with that of conventional 2% Chlorhexidine mouthwash.
Performing oral prophylaxis after recording baseline data was done to assess the effect of scaling alone in control group and to assess effect of the mouthwashes on gingival health in other two groups on subsequent follow-up at 7th, 14th and 21st day. The present study showed improved plaque and gingival health status in all the groups on 7th day. From 7th day till 14th day the reduction in plaque and gingival scores was seen in Group B and Group C as compared to Group A (p<0.001). There was not much difference in reduction of plaque and gingival scores from 14th day onwards in Group B and Group C (p>0.05). The probable reason for not much difference in plaque and gingival conditions at 14th and 21st day in Group B and Group C could be that both the mouthwashes revealed to have maximum benefit from 14th day onward and after that it remains constant confirming the benefits of mouthwashes on long term use in maintaining proper gingival health. On the other hand the gingival health deteriorated in Group A from 14th day to 21st day, thus proving the adjuvant effect of mouthwashes in other two groups. This shows the useful effect of scaling on gingival health for transient period. The results of the present study were similar to the study conducted by Aspalli et al., and Parwani et al., where herbal mouthwash was equally effective to Chlorhexidine mouthwash [12,17]. Also the study conducted by Rao et al., have shown Arimedadi oil to be effective in improving periodontal status in more than 80% subjects while in the present study there was improvement in periodontal status in all 100% (15) subjects in Group C [6].
A large number of microorganisms including gram positive and gram negative organisms, fungi, yeasts, and viruses are inhibited by Chlorhexidine gluconate mouthwash as it exhibits both anti-plaque and antibacterial properties. Its superior anti-plaque activity is attributed to its substantivity and pin-cushion effect [11].
On the other hand Arimedadi oil contains, Manjishtha (Rubia cordifolia), Khadira (Acacia catechu), Til oil (Sesamum inidicum), Clove (Syzygium aromaticum) and many other ingredients. Khadira has been proven for its astringent and bactericidal properties, khadira as an analgesic and anticaries agent, manjishtha as an astringent, analgesic, anti-inflammatory blood purifier, clove as an analgesic, anti caries and antimicrobial agent, til oil as anti-plaque and anti gingivitis agent [18–21]. The improvement in gingival health in Group C might have been due to these ingredients present in the Arimedadi mouthwash. However, the exact mechanism of action of the Arimedadi ingredients on gingival health needs to be explored.
It has been reported that in females, hormonal changes during menstrual period have significant effect on gingival health [22]. So in this study during recruitment of females it was kept in mind to exclude those females who were in menstrual period to overcome the effect of hormonal changes on gingival health. This proves that whatever changes in gingival health could be attributed to the intervention carried out in present study than hormonal changes. Thus confirms the role of mouthwash on gingival health.
The present study was carried out over a period of 21 days in order to assess the long term effect of mouthwashes. According to Naitkari et al., Chlorhexidine should never be used for more than two weeks to avoid its local side effects such as teeth staining and taste alteration. No adverse effect was seen during the course of this study as oral prophylaxis performed at baseline and routine oral hygiene practices reduced the chances of staining of teeth during the study period [16, 23]. Arimedadi oil mouthwash was unpalatable when tested for its taste by principal investigator so noncompliance was foreseen. To overcome the non compliance, during the study period dental students were recruited in this study. However, Arimedadi oil mouthwash did not show any side effects after its usage.
Studies conducted on plaque and gingival diseases are subject based. Successful management of these requires more research into factors such as poor oral hygiene, diet, lifestyle, salivary flow/content, and other customs [24–27]. Correcting the factors, which have led to gingivitis in the first place alone, can prevent recurrence.
The Ayurvedic mouthwash used in the study was equally effective like chlorhexidine mouthwash in improving gingival health; however, the compliance with Arimedadi is questionable due to its taste. So efforts should be made to make it more compliant and palatable by adding sweeteners and flavoring agents without compromising on its chemical properties and effectiveness on oral health care. Further studies need to be conducted among general public in order to explore the efficacy and safety of the mouthwash on other forms of periodontal diseases.
Limitation
Arimedadi oil proved to be effective in reduction of gingival inflammation and plaque accumulation when it was used over the period of this study, however in order to see its long term effects longitudinal studies need to be conducted. Though it did not show any side-effects of its usage during the course of the study further clinical trials are required to check for its substantivity, minimum inhibitory concentration and its effects on systemic health also. Keeping this in mind, this herbal product can have clinical implication of being an effective alternative to Chlorhexidine with least or negligible side-effects and it could be advocated and recommended by dental professionals in gingivitis and periodontitis cases.
Conclusion
The effectiveness of Arimedadi oil as a mouthwash was same compared to 0.2% Chlorhexidine Gluconate mouthwash. It should be explored for its cost-effectiveness and safety on long term usage. This could well prove to be an effective and safe alternative for chlorexidine mouthwash.
p value <0.05 considered statistically significant.
*** The mean difference is very highly significant at the .001 level.
p-value <0.05 considered statistically significant.
*** The mean difference is very highly significant at the 0.001 level.
p-value <0.05 considered statistically significant.
p value <0.05 considered statistically significant.