Symptom Scales (SS) are questionnaires for evaluating and following up of special illnesses. They are used as diagnostic tools. There are simple questions for patients to express his/her illness and these questions help physicians understand the patient’s complaint better. At the same time SS is used to get standardized knowledge for a study. In the past SS often meant long and difficult forms, which are not practical in any thing other than a research environment. However, now-a-days SS have been tried to be designed as easily understood by the physician and patient in minutes [1,2].
SS used for the diagnosis and follow-up of Lower Urinary Tract Dysfunction (LUTD) in children is called LUTD Symptom Scale (LUTDSS) [3,4]. LUTD in children is defined as a field of confusion. The definitions of commonly used terms, such as enuresis, incontinence, OAB, etc. can be used interchangeably to refer general dysfunction or vice versa. This confusion is partly due to advancement in paediatric urology, and it changed our views of these conditions radically [5]. LUTD in children consists of two main groups of diseases: storage disorders and emptying disorders. Overactive bladder, stress incontinence, and giggle incontinence are storage disorders. Staccato voiding, dysfunctional elimination syndrome, lazy bladder, primary bladder neck dysfunction, vaginal reflux, Hynmann Syndrome, and fractional voiding are emptying disorders [6]. The diagnosis of LUTD is made by LUTDSS, Uroflowmetry-Electromyography (Uroflow-EMG)-Postvoid Residual Urine (PVR) test and bladder diaries [7]. Only Uroflow-EMG-PVR or only bladder diary is not enough to diagnose LUTD. LUTDSS must be used to diagnose, evaluate and classify the LUTD.
Present study was conducted with the aim to identify the questions that are more important for the diagnosis of LUTD and create a simpler SS.
Materials and Methods
This cross-sectional study was conducted in Etimesgut Military Hospital and Gulhane Military Medical Academy. This study was approved by the Ethical Committee of our institution and followed the Institution’s Review Board of Human Subject Guidelines.
From January 2005 to March 2015, 631 children between the age 5 and 15 were enrolled in this study. LUTDSS was applied to all children and their families were asked for any family or psychosocial problems. All children underwent a complete physical examination including a neurourologic examination. Two hundred sixty three children from a nursery and secondary school saying that they have no urinary complaints and having LUTDSS <9 were designed as control group [3]. Three hundred fifty seven children attending the hospital with urinary complaints and having LUTDSS score ≥9 were thought as having LUTD. These children were evaluated by urinalysis, urine culture, serum urea and creatinine, lumbosacral spine radiography and urinary ultrasonography. Eleven children with active urinary tract infections were excluded from the study. The diagnoses of LUTD were verified by using 3-day bladder diary and 2-time Uroflow-EMG-PVR tests [3].
The inclusion criteria for LUTD group were firstly being 5-15-year-old, and having LUTDSS ≥9; then having abnormal voiding pattern (staccato, urge, fractioned), EMG activity while urinating (external sphincter), PVR >20 mL and abnormal symptoms in bladder diary [5,8]. Staccato voiding pattern was defined as continuous but fluctuating flow curve and larger than the square root of the maximum flow rate. Urge voiding pattern was defined as a sudden appearing curve like a tower and fractioned voiding pattern was defined as intermittent curves with stops and beginnings [5,8]. The exclusion criteria were family or psychosocial problems and any neurologic or constitutional urologic abnormality detected by physical examination or laboratory tests. The control group did not have further evaluation with 3-day bladder diary and 2-time Uroflow-EMG-PVR tests. LUTSS questions in LUTD and control groups were compared.
Statistical Analysis
Statistical analysis was done using Statistical Package for Social Sciences 20 software (Chicago-USA) (SPSS 20 for MAC). Descriptive statistics were noted with mean, frequency, percentiles, and minimum-maximum. Skewness, Kurtosis and Shapiro Wilk test were used to assess the variables’ normalization. Factor Analyses (FA) and Enter Logistic Regression Analyse (ELR) [9] was done in order to determine the important questions for the diagnosis of LUTD. After forming a statistical model with FA and ELR, ROC curve used to identify the exactness of statistical model [10].
Results
There were 232 girls and 125 boys in LUTD group and 182 girls and 81 boys in control group (p>0.05). The average age was 8.49 ± 2.34 in LUTD group and 9.39 ± 2.73 in control group (p>0.05). There was no demographic difference between LUTD and control groups. None of children had family or psychosocial problems. Two hundred fourteen (60%) of LUTD group had staccato, 22 (6%) had urge, 114 (32%) had normal, 7 (2%) had obstructive voiding pattern. Two hundred seventy five (77%) of patients had EMG activity while urinating. PVRs were greater than 20 ml in 89 (25%) of LUTD group. Maximum flow rate was <10 ml/s for 26 (7%) and ≥10 ml/s for the other 331 (93%) patients.
Answered questions of LUTDSS in LUTD and control groups are depicted at [Table/Fig-1].
Answered questions of LUTDSS in LUTD and control groups.
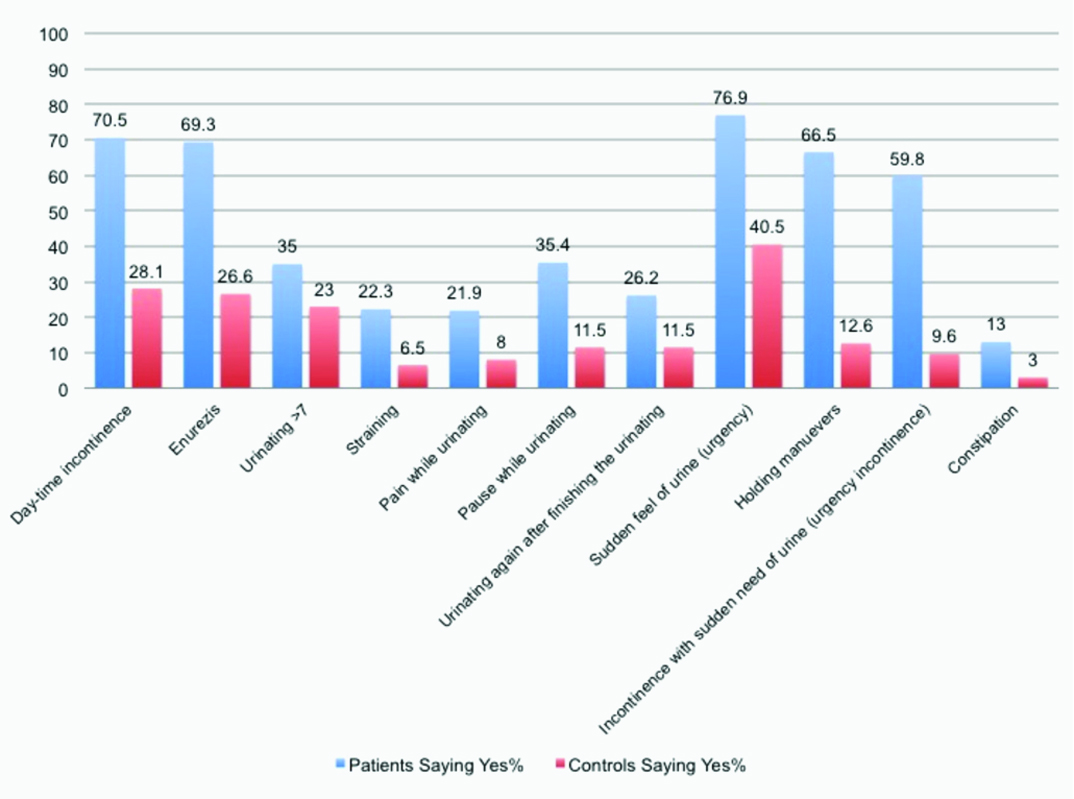
Once the answered questions of LUTDSS in LUTD group were evaluated by factor analyses, Kesier Meyer Olkin score and p score was detected 0.60 and p=0.001, respectively. This meant that factor analysis was a good evaluation tool for detection of important questions in LUTDSS in LUTD group. First, 3rd., 8th. and 10th questions were detected as the most answered questions in LUTD group by factor analyse. Then the answered LUTDSS questions of LUTD and control groups were evaluated by ELR, and the same questions were detected statistically significant for the detection of LUTD. According to ELR, children with daytime incontinence (first question) were 47.7 (4.8-510) times (p=0.01), children with enuresis (third question) were 59.53 (6.2-961) times (p=0.001), children with pause while urinating (eighth question) were 28.7 (4.4-2090) times (p=0.001), children with urgency (tenth question) were 54.7 (29.3-604) times (p=0.039) more likely to have LUTD than the children not having these complaints. When using the parameters detected by ELR created the ROC curve, area under curve was calculated 86.4% [Table/Fig-2a]. On the other hand comparing the LUTDSS questions of LUTD group with control group having LUTDSS=0, 1., 3., 8., and 10 questions were detected statistically significant for the detection of LUTD again. Children with daytime incontinence (first question) were 88.64 (44-103) times (p=0.001), children with enuresis (third question) were 32.94 (34-52) times (p=0.001), children with pause while urinating (eighth question) were 47.54 (106-38) times (p=0.001), children with urgency (tenth question) were 14.38 (36-12) times (p=0.001) more likely to have LUTD than the children not having these complaints. Creating a ROC curve using the parameters detected by ELR again, and area under curve was calculated 96.3% [Table/Fig-2b]. The sensitivity and specifity of each question in LUTDSS are also yielded in [Table/Fig-3]. First, 3., and 10. questions have higher sensitivity, and 8. question has higher specifity than other questions. These findings mean that using only 1.,3.,8., and 10. questions can make diagnosis of LUTD in children and form a simpler SS with 4 questions [Table/Fig-4].
ROC curve with 1st., 3rd., 8th., and 10th. questions (a. ROC curve for patients with LUTDSS <9, b. ROC curve for patients with LUTDSS =0).

Predictive values of LUTDSS questions.
| Questions of LUTHSS | Sensitivity (%) | Specificity (%) |
|---|
| 1. Does your child have daytime wetting? | 70.5 | 69.3 |
| 3. Does your child have night wetting | 74 | 68.9 |
| 5. How many times does your child urinate | 35 | 54 |
| 6. Does your child strain while urinating | 22.3 | 93.5 |
| 7. Does your chıld have pain while urinating | 21.9 | 91.6 |
| 8. Does your child urinate with pauses | 35.4 | 88.5 |
| 9. Does your child go to urinate again after finishing urinating | 26.2 | 88.5 |
| 10. Does your child say a sudden need of urinating? | 76.9 | 59.2 |
| 11. Does your child try to hold urinating with abnormal maneuvers | 66.5 | 87.4 |
| 12. Does your child get wet after sudden need of urinating | 59.8 | 90.4 |
| 13. Does your child have constipation | 13 | 90 |
* LUTDSS: Lower Urinary Tract Dysfunction Symptom Score
| Yes | No |
|---|
| 1. Does your child have daytime wetting? | | |
| 3. Does your child have night wetting | | |
| 8. Does your child urinate with pauses | | |
| 10. Does your child say a sudden need of urinating? | | |
Discussion
SSs capture patient’s own perceptions of their health and ability to function of life. Some studies show that physicians typically underestimate the symptoms that patients experience [2]. Sometimes patients do not want to tell their problems by speaking and sometimes they do not know how to grade their symptoms. Some studies suggest that physicians overestimate the impact of disease and it’s treatment results. So, using a SS is a timesaving and easy way of learning of patient’s feelings.
There are many SSs in Urology. Sickness Impact Profile (SIP), Melzac Pain Questionnaire (MPQ), Expanded Prostate Cancer Index Composite (EPCIC), Prostate Cancer Treatment Outcome Questionnaire (PCTOQ), Incontinence Impact Questionnaire (IIQ) is some examples of SSs, but mostly used ones are International Prostate Symptom Index (IPSS), International Index Of Erectile Function (IIEF), Overactive Bladder Questionnaire (OVQ) and Incontinence Impact Questionnaire-Short Form (IIQ-SF). When looking at the most used ones and classical ones, one can easily see the difference. Classical ones have lots of questions, which are difficult for patient and the physician to read, understand and answer. On the other hand, mostly used ones have a few easily understood questions. This shows the need for simple SSs in urology.
LUTDSS for children had been named as dysfunctional voiding symptom score (DVSS) for long time. Farhat et al., described a DVSS and mentioned that it could help to identify patients easily and direct treatment and investigation, and stratify treatment intensity [11]. Akbal et al., designed a DVSS by modifying the form from the one used by van Gool et al. for the International Reflux Study in Children [3,4,12]. Akbal et al., compared the forms of children with dysfunctional voiding and forms of healthy children [4]. Then they scored each questions by using their odds ratios and created a new one. At the end they concluded that the score 8.5 or greater (not including quality of life score) had voiding abnormalities with a sensitivity of 90% and a specificity of 90%. In our study, we used the same form created by Akbal et al., and named it as LUTDSS. Scores of our patient group were greater than 9.
The form of Farhat et al., was designed like IPSS. It has 10 questions, and 5 answers for first 9 questions [11]. The last question was in yes or no format. The form of Akbal et al., was mostly in yes or no format, but first 4 of 13 questions had multiple choices [3,4,12]. In our clinical practice, most parents report that they had difficulty for answering the first 4 questions. So, in our opinion, LUTDSS in yes or no format will be more applicable in clinical practice. Our new LUTDSS consists of 4 questions in yes or no format. These questions were detected by FA, ELR, ROC curve, and sensitivity and specificity tests.
Limitation
The main limitation in this study is that we did not compare our new SS with standard LUTDSS in patients. Comparing these SSs will be our future investigation.
Conclusion
The new SS is shorter and seems to be as accurate as the LUTDSS. It seems to ease the diagnosis and follow-up of children with LUTD.
* LUTDSS: Lower Urinary Tract Dysfunction Symptom Score