Hip fractures are often encountered in the elderly and present special problems to the anaesthesiologist [1]. Surgical repair in these patients usually involves internal fixation of the fracture. Spinal anaesthesia is a commonly used technique to facilitate surgery in these patients. However, positioning of these patients for spinal anaesthesia is troublesome as even a minimal overriding of fracture ends is extremely painful [2]. Adequate pain relief before positioning increases comfort and improve positioning before spinal block [3]. Various analgesics such as NSAIDS (diclofenac, parecoxib) and opioids are commonly used to treat pain in these patients. Analgesics are associated with adverse effects like nausea, vomiting, drowsiness, dry mouth, miosis, orthostatic hypotension, urinary retention and constipation. Systemic opioids are associated with respiratory depression, cough suppression, rigidity and pruritus [4]. An alternative to systemic analgesia is peripheral nerve blockade. Femoral and 3- in-1 nerve block have been used to provide analgesia in patients with hip fractures in prehospital setting and emergency department [5–7].
Femoral nerve block is easy to perform and has been shown to provide excellent analgesia for femoral fractures [5]. This has also been used to provide analgesia during positioning of the patients for spinal anaesthesia [8]. In a study conducted by Tondare and Nadkarni, it was observed that excellent pain relief can be obtained for mid shaft fractures, good relief for lower third fractures, and partial relief for upper third fractures using femoral nerve block [9]. Three-in-one nerve block technique is a variation of femoral nerve block which along with femoral nerve also blocks lateral cutaneous nerve and obturator nerve [7].
Fascia iliaca compartment block is another technique with the intent to block all the three nerves like 3-in-1 nerve block [10]. This was first described by Dalens et al., Iliacus and iliopsoas muscles are covered in a dense fascia known as fascia iliaca [11]. Femoral nerve originates from the L2 to L4 nerve roots and travels under the iliacus fascia along with the lateral femoral cutaneous nerve and the obturator nerve [12]. There is evidence to suggest that the fascia ilica compartment block is easy to perform, and can be accessed via a minimal risk approach. Compared with the 3-in-1 block, fascia iliaca compartment block provides a faster and more consistent simultaneous blockade of the lateral femoral cutaneous and femoral nerves [13]. The fascia iliaca block has traditionally been undertaken by Loss Of Resistance (LOR) using palpable anatomical landmarks. With ultrasound the femoral nerve and fascia iliaca are visualized and local anaesthetic is deposited beneath the fascia, lateral to the femoral nerve [14]. This study was planned to evaluate the analgesic efficacy of ultrasound guided fascia iliaca compartment block to facilitate positioning for spinal block in patients with hip fracture.
Materials and Methods
This prospective study was conducted in the Department of Anaesthesiology and Critical Care, Pt. B. D. Sharma, UHS, Rohtak in 18 month period from April 2013 to September 2014 and ethical clearance was taken from ethical committee. Fifty patients aged between 40-80 years, belonging to American society of Anesthesiologists (ASA) physical status I-III undergoing surgery for hip fracture were included in this study. Patients having haemorrhagic diathesis, peripheral neuropathy, allergy to amide local anaesthetics, mental disorders, and patients who refuse to participate in the study were excluded. All the patients were examined in ward one day before surgery and complete physical as well as systemic examination was done. Routine investigations such as haemoglobin, bleeding time, clotting time and urine examination were carried out in all patients. The purpose and protocol of the study was explained to patients and informed written consent was obtained. Linear Visual Analogue Scale (VAS) on 0-10cm was explained to all 50 patients for the assessment of pain where 0 denotes no pain and 10 denotes worst pain imaginable. Upon arrival in premedication room, usual monitoring including Heart Rate (HR), Non-Invasive Blood Pressure (NIBP), Electrocardiography (ECG) and pulse oximetry (SpO2) were established. Intravenous line was secured with 18G venous cannula.
All the patients received an ultrasound guided fascia iliaca compartment block in the premedication room. Images were obtained using a sonosite M-Turbo ultrasound machine with an HFL38 x 13-16 MHz 40mm broadband linear array probe. The ultrasound probe was placed in transverse orientation on the thigh just inferior to inguinal ligament at one-third of the distance from Anterior Superior Iliac Spine (ASIS) to pubic tubercle. The two fascial planes, the fascia lata and the fascia iliaca were visualized as two hyperechoic lines. The bright band covering the iliacus was the iliacus fascia (or fascia iliacus). After local skin disinfection using topical 10% povidone iodine, a short beveled 23G Quincke’s lumbar puncture needle was introduced through the skin in a lateral to medial orientation and directed in plane to ultrasound probe to allow visualization of the full length of the needle throughout the procedure. The needle tip was visualized penetrating the fascia lata and then the fascia iliaca. After puncturing the fascia iliaca, and negative aspiration, 30 mL of 0.5% ropivacaine was injected over a 2-3 minutes period interrupted by intermittent aspirations. An expanding anechoic collection just below the fascia iliaca was the visual confirmation of correct placement of anaesthetic.
Sensory blockade was evaluated 5, 10 and 20 minutes after ropivacaine administration using loss of perception to cold in the lateral, anterior and medial part of the thigh (corresponding to Lateral Femoral Cutaneous (LFC), Femoral (F) and Obturator (O) nerve sensory distributions, respectively). Sensory Block was assessed as follows: Complete Block- Block in all the three thigh regions; Partial Block- Block in one or two thigh regions and Block failure- Block in no thigh region at 20 minutes after the local anaesthetic injection. After the evaluation of cold perception loss by the FIC block at 20 min, patient was moved to operating room where spinal anaesthesia was administered in sitting position.
Visual analogue scale scores were noted before the block, 20 min after block and during positioning for spinal anaesthesia (approx. 30 min after block). If patient reports a VAS score ≥ 4 during positioning, procedure was stopped, and 30mg of IV ketorolac was given. Positioning was reattempted after reduction of VAS to less than 4. Patient positioning was evaluated as 0=unsatisfactory, 1=satisfactory, 2=good or 3=excellent. The VAS score during patient positioning and the quality of position was recorded by the anaesthesiologist administering the spinal anaesthesia. Patient’s acceptance for FIC block was evaluated 24 hour after arriving back to the orthopaedics ward using a two-point score: 1=good (if necessary, I would have the block again) and 2=bad (I would never have the block).
Monitoring of HR, ECG, NIBP and SpO2 was performed at 0, 5, 10 and 20 minutes after the block and then continuously in operating room. Any episode of hypotension (decrease in MAP more than 10% of the baseline value) or bradycardia (Heart rate less than 60/min) was noted and managed accordingly.
Results
Out of total 50 patients 19 patients (38%) were less than 60 years and 31 patients (62%) were above 60 years. Mean age of patients included in this study was 61.5 years. Out of 50 patients 31 (62%) were males while 19 (38%) were females. In this study 18 patients (36%) had weight less than 65 kg and 32 patients (64%) had more than 65 kg. In our study #NOF (n=9) and #Tr (n=41) were taken as hip fracture cases. Out of total 9 patients with #NOF, 3 patients (6.66%) had # in left side, and 6 patients (13.33%) on right side. Out of 41 cases of #Tr., 20 patients (40%) had #Tr on right side and remaining 21 patients (42%) on left side. Duration of surgery in these hip # patients was between 60 to 120 minutes in 43 cases (86%) and more than 120 minutes in 7 cases (14%). In these patients no surgery was completed in less than 60 minutes. Mean time for duration of surgery was 99.94 min ± 19.12 minute In our study patients were classified on the basis of ASA physical status I-III.
Out of total 50 patients, distribution of cases was as follow: 27 (54%) patients (grade I), 18 (36%) patients (grade II) and 5 (10%) patients (grade III). Mean haemoglobin level was 11.90±1.25. Mean blood sugar level was 97.26±17.42. Mean blood urea level was 21.02±7.09.
In present study sensory blockade after FIC block was assessed at different time intervals (5, 10, 20 minutes) in lateral, anterior and medial thigh. In lateral part of thigh, at 5 minutes sensory blockade was present in 33 patients (66%) and at 10 minutes sensory blockade was present in 45 patients (90%). Sensory blockade was same at 20 minutes in lateral part of thigh as that present at 10 minutes interval. These difference of sensory blockade was statistically insignificant (p=0.413). In anterior part of thigh and medial part of thigh also the statistical relation was not significant (p=0.226) [Table/Fig-1].
Sensory blockade after FIC block at different time intervals.
| Present (%) | Absent (%) | p-value |
|---|
| Lateral thigh5 minutes10 minutes20 minutes | 33 (66%)45 (90%)45 (90%) | 17 (34%)5 (10%)5 (10%) | 0.413 |
| Anterior thigh5 minutes10 minutes20 minutes | 34 (68%)48 (96%)48 (96%) | 16 (32%)2 (4%)2 (4%) | 0.226 |
| Medial thigh5 minutes10 minutes20 minutes | 28 (56%)43 (86%)43 (86%) | 22 (44%)7 (14%)7 (14%) | 0.226 |
After assessing sensory blockade in three different parts of thigh, sensory block was assessed as complete block, partial block and block failure at 5, 10 and 20 minutes time interval after block. At 5 minute 18 (36%) patients had complete block (sensory blockade in anterior, lateral and medial part of thigh). At 10 minute time interval, a total of 40 (80%) had complete block. Total number of patients having complete block was same at 20 minutes as that at 10 minutes time interval. We found statistically significant relation between partial blockade at 5 minute Vs complete block at 10 minutes (p<0.01). Partial block was present in 28 (56%) patients at 5 minute which progressed to complete block in 19 out of 28 patients at 10 minute and 20 minutes. Only in 9 patients, block remained partial at the end of 20 minutes. This progression of partial block into complete block with increase time interval was statistically significant (p<0.01). There was only 1 block failure at 20 minutes out of total 50 cases [Table/Fig-2].
Characteristic of block at different time intervals.
| Present (%) | Absent (%) | p-value |
|---|
| Complete block5 minutes10 minutes20 minutes | 18 (36%)40 (80%)40 (80%) | 32 (64%)10 (20%)10 (20%) | <0.01 |
| Partial block5 minutes10 minutes20 minutes | 28 (56%)9 (18%)9 (18%) | 22 (44%)41 (82%)41 (82%) | <0.01 |
| Block failure5 minutes10 minutes20 minutes | 3 (6%)1 (2%)1 (2%) | 47 (94%)49 (98%)49 (98%) | <0.01 |
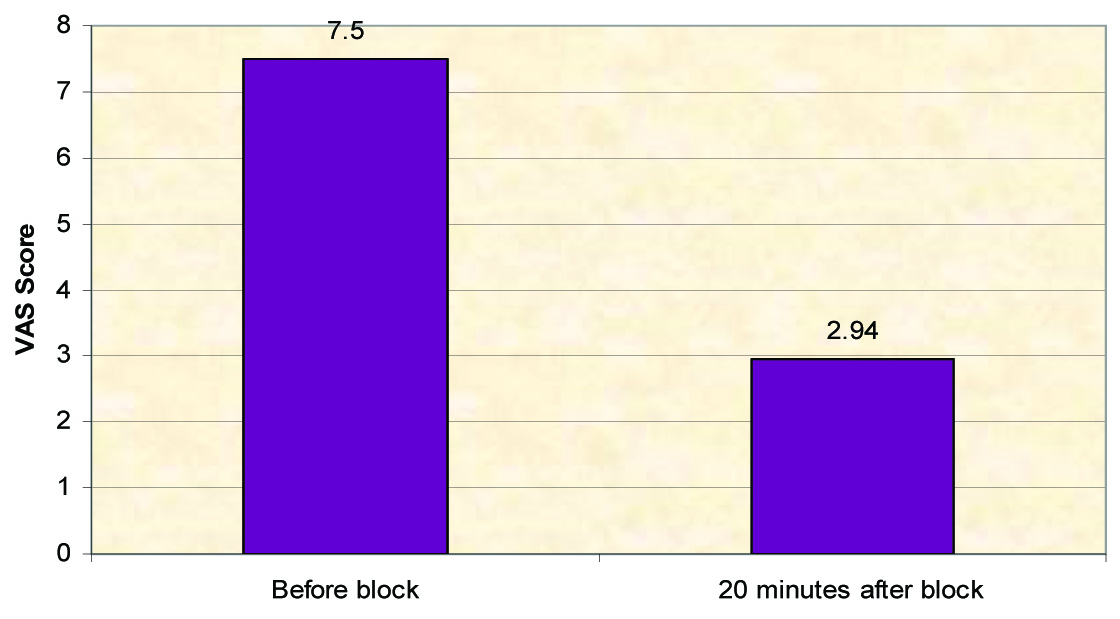
In this study we assessed VAS before block and after 20 minutes of block between 0 to 10 scales. Before FIC block average VAS was 7.5 which was decreased to average of 2.94 at 20 minutes after block which was statistically significant (p<0.01). During positioning for spinal anaesthesia, 46 patients had VAS less than 4 [Table/Fig-3].
VAS score before and after block.
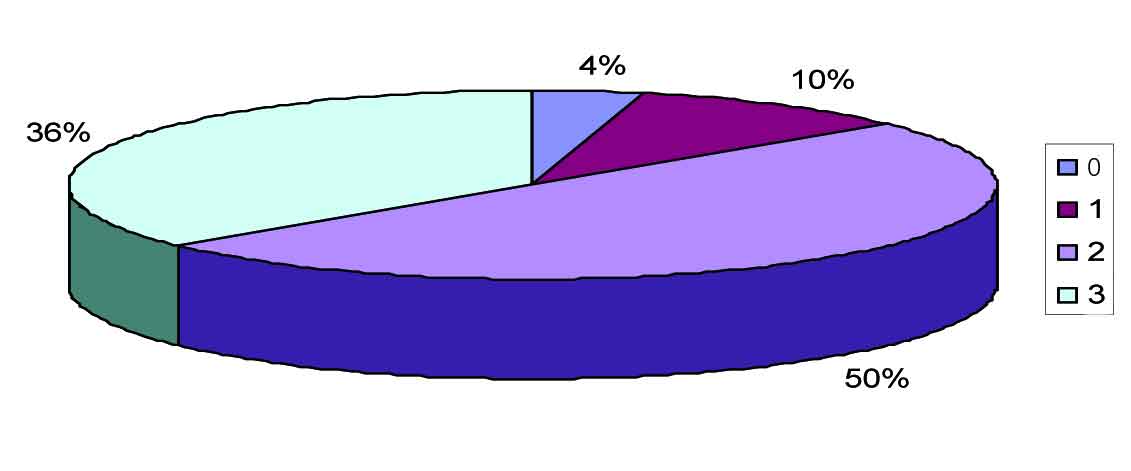
In our study, only 4 patients required supplementary analgesia for positioning before spinal. Positioning during spinal anaesthesia was assessed unsatisfactory (0) in 2 cases (4%), satisfactory (1) in 5 cases (10%), good (2) in 25 cases (50%) and excellent (3) in 18 cases (36%) [Table/Fig-4].
In our study preoperative monitoring of heart rate, NIBP and oxygen saturation was done at 0,5,10,20,30,45,60,90 minutes. Only 7 patients presented with hypotension after the block. All cases of hypotension were presented after spinal anaesthesia at 30 to 60 minutes after FIC block. Out of all these 50 cases only 3 patients suffered bradycardia. No other complication was seen after block in our study group. Satisfaction of patients about block was assessed on 2nd day after 24 hrs and 45 patients (90%) were satisfied with the block
Discussion
In our study lateral cutaneous nerve of thigh (supllies lateral part) was blocked in 90% of cases at 20 minutes of time interval after block. Anterior part which was supplied by femoral nerve was blocked in 96% of cases. In 86% of patients in present study, lowest blockade was in medial part which is supplied either by femoral nerve or invariably by obturater nerve. At 5 minute 18 (36%) patients had complete block and at 20 minute time interval, a total of 40 (80%) had complete block. We found statistically significant relation of complete block (p<0.01). Yun et al., studied 20 patients in which 40% of patients had a complete blockade and the remaining 60% of the patients had a partial blockade. They also found less sensory blockade in medial part [2]. Pandya et al., compared FIC block and 3-in-1 nerve block with assessment of blockade of femoral, obturator and genitofemoral nerves. Sensory blockade of lateral part (93.33%) was significantly higher in FIC group in their study. This result was comparable with our study [15]. Wallace et al., noted that sensory block for LFC was higher in FIC block group at all point of time compared with 3-in-1 group but this did not achieve statistical significance. The LFC was the only nerve that was noted to have achieved a higher degree of blockade in FIC group. However when the percentage of subjects who achieved complete blockade of all three nerves at 30 minutes was only 67%, in their study [16]. This result was low as compared to our study even though we measured blockade at 20 minutes. These differences in results may be due to use of ultrasound guidance in our study.
Dolan et al., found statistically significant increase in the incidence of sensory loss in the medial aspect of the thigh 95% as compared to loss of resistance technique 60% (p=0.001) [14]. Complete loss of sensation was observed in 82% of patients using ultrasound as compared to loss of resistance technique 47% patients (p=0.001). Ultrasound guided fascia iliaca block resulted in a statistically significant increase in the incidence of femoral (p=0.006) and obturator (p=0.033) nerve motor block [15]. We did not compare our result with loss of resistance technique, but complete blockade was comparable to their study which was almost equal. Degree of blockade in medial compartment was lower but was same in relation to anterior and lateral compartment.
Lopez et al., observed blockade of medial compartment of thigh without ultrasound guidance in 92.6% of the cases at 10 minutes after the block and in 96.3% at 40 minutes. The lateral part of the thigh was blocked in 37% of cases at 10 minutes and in 51.9% at 40 minutes. The internal part of the thigh was blocked in 22.2% of the cases at 10 minutes and in 37% at 40 minutes. There was 1 block failure in their case series. Seven patients had a complete block and 19 had a partial block [10]. Our result showed increase in percentage of blockade (lateral part) with ultrasound guidance. However, Lopez et al., observed more blockade in medial part even without ultrasound guidance [10].
In this study, we assessed VAS before block and after 20 minutes of block between 0 to 10 scales. Before FIC block average VAS was 7.5 which was decreased to average of 2.94 at 20 minutes after block which was statistically significant (p<0.01). During positioning for spinal anaesthesia, 46 patients had VAS less than 4. Yun et al., calculated the VAS scores (mean and range) during positioning before spinal anaesthesia which was 2.1±0.9. This VAS scores was 2.0±0.6 at 20 minutes of blockade [2]. These both VAS scores at 20 minutes and before spinal anaesthesia were almost equal to our results. Haines et al., reported a statistically significant lower mean pain scores compared to time 0. The lowest mean pain score of 1.3/10 was achieved at time 120 min, which represents a 76% drop in pain from just before the placement of the block in their case series. They found mean pain scores 2.55 at 20 minutes after blockade which was 2.95 in our case series which was statistically significant (p=0.0001) [4]. Hogh et al., found decreased verbal pain scores to a median of 1.5 (SD±0.78) at 15 minutes of post-block (p=0.001) and 1.3 (SD±0.71) at 60 minutes of post-block (p=0.021). They had median of 2.5 (SD±0.92) before the block [17]. These data show significant decrease in pain score which was decreased to 2.94 from 7.5 (p<0.01) in our study as seen just in their study. Pandya et al., observed VAS scores 4.27±0.74 before block which was decreased to 3.43 ± 2.36 in FIC group at 12 hours which was statistically significant (p=.036). They did not calculate VAS scores at 20 minutes. But this study supported our results [15]. Lopez et al., measured Simplified Verbal Scale (SVS) instead of VAS scores from 0 (no pain) to 4 (extreme pain). The SVS was noted before the block was performed, 10 minutes later, and then at 40 minutes on admission to the trauma care center. The SVS mean (range) was 3 (3-4) before the block, 1 (0-2) 10 minutes after the block, and 0 (0-1) when arriving at the trauma care center (p<0 .05) [10]. These result also supported our finding about statistically significant decrease in pain scores however we used VAS scores. In our study, only 4 patients required supplemantary analgesia for positioning before spinal. Yun et al., observed additional analgesic requirement in 12 of 20 patients of partial block but only 2 patients required out of 7 in our study [2]. These results were more superior than their study. Positioning during spinal anaesthesia was assessed unsatisfactory (0) in 2 cases (4%), satisfactory (1) in 5 cases (10%), good (2) in 25 cases (50%) and excellent (3) in 18 cases (36%). In our study preoperative heart rate monitoring was done at 0, 5, 10, 20, 30, 45, 60, 90 minutes after block. Preoperative NIBP monitoring was also done at same 0, 5, 10, 20, 30, 45, 60, 90 minutes. Preoperative monitoring of patients oxygen saturation was also done at same time interval.
Only 7 patients presented with hypotension after the block. All cases of hypotension were presented after spinal anaesthesia at 30 to 60 minutes after FIC block. Out of all these 50 cases only 3 patients suffered bradycardia. All cases of bradycardia were presented between 30 to 60 minutes after block and all are after spinal anaesthesia. No other complication was seen after block in our study group.
Satisfaction of patients about block was assessed on 2nd day after 24 hours and 45 patients (90%) were satisfied with the block. Acceptance of FIC block was found in 19 out of 20 cases in Yun et al., [2].
Limitation
This study was done to study the role of FICB but did not compare the effect of other commonly used lower limb block. The comfort level of positioning before SA may vary from person to person as per their experience.
Conclusion
Ultrasound guided FICB can be performed safely without complications in controlling pain for patients with hip fracture. Analgesic property of FICB is useful as pre-operative medication and adjuvant to spinal anesthesia to control surgical stress response in case of hip fracture surgeries. The FICB before positioning for SA provides good pain relief and improve spinal performance with good patient acceptance, hence improving overall quality and efficiency of patient care. FIC block is efficacious in terms of facilitating the sitting position for spinal anaesthesia in patients undergoing hip fracture surgery.