The removal of subgingival biofilm in the treatment of periodontitis, and the elimination of mineral irritations on the root surfaces, corresponds with periodontal health and stagnation of tissue loss. The consequent emergence of a healthy subgingival microflora is crucial in terms of the periodontal inflammation status [1,2]. The therapeutic aim is to reduce infection associated, with control of inflammation and to prevent any further tissue destruction. The therapeutic effectiveness of SRP in the treatment of chronic periodontitis has been proven in a variety of longitudinal trials [3,4]. SRP is the most frequent form of periodontal treatment [5]. However, investigations have shown that the elimination of pathogenic periodontal bacteria merely by means of mechanical debridement is unpredictable [6,7].
Over the years, numerous trials have sufficiently documented the benefits of adjuvant administration of antibiotics in combination to SRP [8–10]. The effectiveness of specific antibiotic types has been demonstrated for decades. For instance, an additional administration of amoxicillin and metronidazole has been proven to lead to a significant reduction in Aggregatibacter actinomycetemcomitans [11]. It follows, therefore, that the administration of various antibiotics would certainly be indicated in cases in which SRP alone does not produce the anticipated success due to persistent pockets or inaccessible points (e.g., furcation and concavities).
There are nevertheless justified doubts in respect to antibiotic administration per se [12,13]. The macrolide antibiotic agent Azithromycin (AZM) is an antibiotic which until now has featured less significantly in adjuvant administration as part of periodontitis therapy. It possesses good oral absorption and is characterised by extremely good resilience toward gastric acids. It possesses high effectiveness toward gram-negative bacteria, and Aggregatibacter actinomycetemcomitans in particular [14]. AZM is effective in the treatment of facial infections and intraoral infections [15,16]. One of the noteworthy benefits that AZM provides is its prolonged existence in the respective tissue. Additionally, far fewer resistances have formed in respect to this antibiotic compared with more frequently prescribed antibiotics [17]. The extremely persistent tissue levels that AZM exhibits and consequently shorter period in which the medication is taken, are auspicious properties [18–20].
The purpose of this review study and meta-analysis was to acquire the ability to make a more precise statement on the benefit of AZM as an adjuvant antibiotic in combination with SRP in chronic and aggressive forms of periodontitis.
Materials and Methods
Protocol: A detailed protocol was introduced and adhered to in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) Statement [21,22].
Search Criteria: A search was conducted in the electronic databases (MEDLINE and Cochrane Central Register of Controlled Trials) to locate all publications from the earliest point of record until May 2015. A hand search of key periodontal journals was also conducted to identify full-text articles from the same period. The search was restricted to English- and German-language articles. A typical search strategy, using Boolean operators was employed to identify papers using MesH, keywords and other free terms: (periodontitis OR chronic periodontitis OR periodontal disease) AND (scaling and root planing OR SRP OR non-surgical periodontal therapy OR periodontal treatment OR periodontal therapy) AND (antibiotics OR azithromycin). No restrictions were made in respect to the time of publication.
Study Selection: Titles and abstracts of selected publication were checked by two blinded independent reviewers (J.H. and R.A.). The defined inclusion and exclusion criteria were then applied to select the relevant trials following consultation. Diverging results were discussed and then positively or negatively assessed during the selection process. Eleven trials were selected for the full-text review.
Inclusion Criteria: The first phase of the search process involved research for Randomised Clinical Trials (RCTs) that compared SRP combined with administration of AZM to those that involved SRP on its own, with or without the administration of a placebo. The inclusion criteria were: Published in English; archived in Pubmed; human studies; RCTs; double-blind or blind; published before May 2015; control group SRP on its own or in combination with placebo; follow-up period 1-12 months; chronic and aggressive periodontitis patients; clinical periodontal assessment parameters: PD, CAL, BOP, PI and bacterial load.
Exclusion Criteria: The following criteria were defined as reasons for exclusion: Expert opinion or recommendation; not a human study; case reports; not a clinical trial.
Search Outcome and Evaluation: Primary outcome measures of interest were the changes of the clinical variables in the different groups over the course of three or six months respectively. Due to the fact, that only two studies reported this information, we decided to work with descriptive statistics of the clinical outcome variables at defined time points (baseline, three and six months).
Risk of Bias in Individual Studies: Risk of bias was evaluated through a process of quality analysis performed by reviewers (J.H. and R.A.). Quality analysis of RCT according to the Cochrane Reviewer’s Handbook [23] implied the assessment of six RCT issues: random sequence generation; allocation concealment; blinding of participants; personnel and outcome assessors; handling of incomplete outcome data; selective outcome reporting and other sources of bias. All the six issues were finally qualified as adequate, inadequate or unclear.
Data Items: To be included in this analysis, the means and standard deviations (or statistical values which can be used to calculate the required items e.g., confidence intervals or standard errors) of PD, BOP, CAL, Plaque Index (PI) and total load of bacteria had to be reported for the baseline and for the follow-up measurements at three and / or six months respectively.
Data Analysis: At first all the studies were screened, if they contain the required information. In studies, where only the confidence intervals or standard errors were given, the standard deviations or means were calculated. After the collection of the information the statistical analysis started. It was all done with Microsoft Excel (Calculations, Microsoft Office 2013) and with the statistic software R (R version 3.0.2, 2013).
At first for each study and each group the effect size cohens d and its confidence interval was calculated.
Here x̄ stands for the mean, and S2 for the variance. For a better comparison and interpretation, this effect size was transformed to the correlation r. Due to the fact that in both groups and all studies the sample sizes were the same at the baseline and the follow-up measures, we used the following formula.
To interpret the overall effect, the weighted mean r̄ was calculated using

Here, s is the number of studies, ni is the sample size of study i, ri is the effect in study i and n=n1+...ns the total sum over all samples in all studies.
In accordance with Cohen et al., (1988) [24] r = 0.1 can be interpreted as a small, 0.3 as a moderate and 0.5 as a large effect.
Results
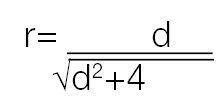
Search Strategy: A total of 88 relevant abstracts were found through the electronic and manual search. After the first screening there were 11 articles remaining and overcame exclusion criteria, based on title and abstract. Of these 11 remaining articles five papers were excluded because they met one or more exclusion criteria [Table/Fig-1a] [25–29]. The agreement between the reviewer was κ=0,90. Finally there were six studies included [Table/Fig-1b] [30–35].
Flowchart of literature search and inclusion.
All considered studies and reasons for inclusion or exclusion.
| Publication | Reference No. | Inclusion/Reason for Exclusion |
|---|
| Emingil et al., 2012 | [30] | Included |
| Gomi et al., 2007 | [31] | Included |
| Haas et al., 2008 | [25] | Only changes of the clinical parameters given |
| Han et al., 2012 | [26] | Only changes of the clinical parameters given |
| Mascarenhas et al., 2005 | [27] | No concrete information about the clinical parameters |
| Oteo et al., 2010 | [32] | Included |
| Pradeep et al., 2013 | [33] | Included |
| Sampaio et al., 2011 | [34] | Included |
| Smith et al., 2002 | [35] | Included |
| Yashima et al., 2009 | [28] | No concrete information about the clinical parameters |
| Haffajee et al., 2007 | [29] | Only baseline-data given |
Study Characteristics: All trials included are RCTs and written in the English language. The publication period extended between 2002 and 2013 [Table/Fig-2]. One trial had a follow-up period of six and 12 months while the remaining five trials included evaluations of three or six months [30–35].
Characteristics of included studies.
| Study (year)Journal | Type | ClinicalParameters | NAge | Treatment | Follow-up(Months) | Outcome |
|---|
| Emingil et al., (2012)[30]Journal of Periodontal Research | RCTDouble-blindPlacebo-controlledParallel-designed | BOPCALPDPI | 3229.16 | Treatment: SRP + Azithromycin (500 mg,3 days)Control: SRP + Placebo (3 days) | 3 and 6 | All clinical parameters improved over 6-month period.Both groups showed similar improvements. |
| Gomi et al., (2007)[31]Journal of Periodontology | RCTParallel-designed | BOPCALPDMB | 3448.20 | Treatment: SRP + Azithromycin (500 mg,3 days)Control: SRP | 3 and 6 | All clinical parameters improved in the treatment-group more than in the placebo groupTotal number of bacteria didn’t change during examination. |
| Oteo et al., (2010)[32]Journal of Clinical Periodontology | RCTDouble-blindPlacebo-controlledParallel-designed | BOPCALPDPIMB | 2846.8 | Treatment: SRP + Azithromycin (500 mg,3 days)Control: SRP + Placebo (3 days) | 3 and 6 | All clinical parameters improved in the treatment-group (PI and BOP improved in the same extend in the placebo-group).Total number of bacteria changed in both groups during examination (no inter-group differences). |
| Pradeep et al., (2013)[33]Australian Dental Journal | RCTDouble-blindPlacebo-controlledParallel-designed | BOPCALPDPI | 54 | Treatment: SRP + Azithromycin gel(0.5 %)Control: SRP + Placebo | 3, 6 and 9 | Significant improvements in the treatment-group compared to the placebo-group for PD, CAL and PI. There was no improvement of BOP. |
| Sampaio et al., (2011)[34]Journal of Clinical Periodontology | RCTDouble-blindPlacebo-controlledParallel-designed | BOPCALPDPI | 4043.96 | Treatment: SRP + Azithromycin (500 mg,5 days)Control: SRP + Placebo (5 days) | 6 and 12 | All clinical parameters improved in both groups (no inter-group difference). |
| Smith et al. (2002)[35]Journal of Clinical Periodontology | RCTDouble-blindPlacebo-controlledParallel-designed | BOPPDPI | 4442.68 | Treatment: SRP + Azithromycin (500 mg,3 days)Control: SRP + Placebo (3 days) | 3 and 6 | PI, BOP improved in both groups to the same extent. The decrease of PD was better in the treatment group compared to placebo group. |
Note: RCT = Randomized Clinical Trial; BOP = Bleeding on Probing; CAL = Clinical Attachment Level; PD = Pocket Depth; PI = Plaque Index; MB = Microbiology; N = Sample Size; SRP = Scaling and Root Planing.
Between 28 and 54 patients (N) were involved in the trials. One trial did not provide an average patient age [33]. All studies included were single centre studies.
Risk of Bias across the Studies: Four of the included studies declared no conflicts of interests by self-supported financing of their research. One study was supporting by Pfitzer Ltd. and another one did not specify [24,35]. The majority of studies included the sample size calculation whereas two studies gave no information about the calculation of the sample size at all [31,34]. Consequently, all studies included in this meta-analysis were considered with low and a minimum of four unclear risks of bias [Table/Fig-3].
Risk of bias summary. L=Low risk bias; U=Unclear risk of bias; H=High risk of bias.
| Emingil et al., 2012 [30] | Gomi et al., 2007 [31] | Oteo et al., 2010 [32] | Pradeep et al., 2013 [33] | Sampaio et al., 2011 [34] | Smith et al., 2002 [35] |
|---|
| Random sequence generation (selection bias) | L | L | L | L | L | L |
| Allocation concealment (selection bias) | L | L | L | L | L | L |
| Blinding of participants and personnel (performance bias) | L | U | L | L | L | L |
| Blinding of outcome assesment (detection bias) | L | U | L | L | L | L |
| Incomplete outcome data (attrition bias) | L | L | L | L | L | L |
| Selective reporting (reporting bias) | L | L | L | U | L | U |
| Other bias | L | L | L | L | L | L |
Study Results: There were no significant differences ascertained if one compares all trials as per the start of the trial. One trial examined patients with aggressive periodontitis [30], while the remaining trials only included patients with chronic periodontitis. One trial involved local application of AZM in a 0.5% solution [32]. Five trials used AZM by a dose of 500mg/3days. Only one study altered this dosage protocol, administering AZM (500mg/5days). The results of one study indicate that both therapies (SRP + LDD of placebo in Group 1 and SRP + LDD of 0.5% AZM in Group 2) resulted in significant improvements [33]. All trials involved six probe points per tooth in order to assess the periodontal condition, and SRP was conducted using handheld instruments.
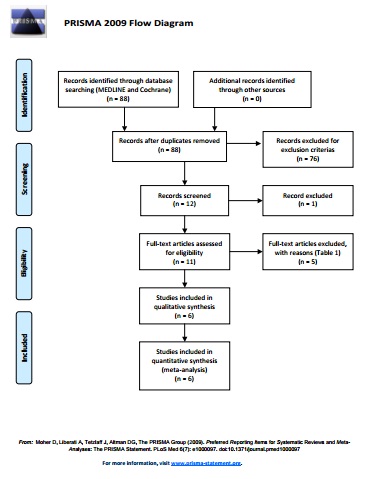
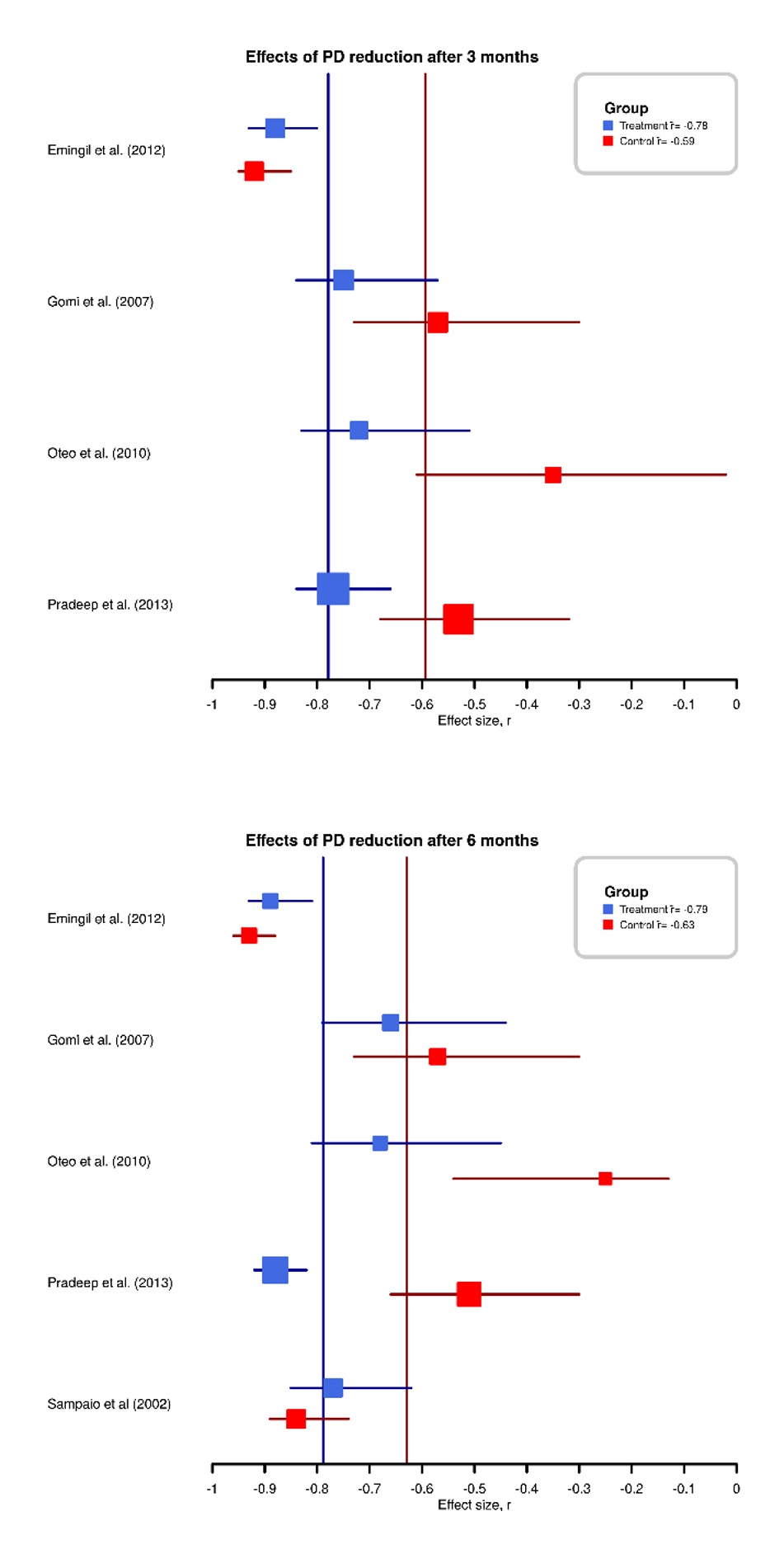
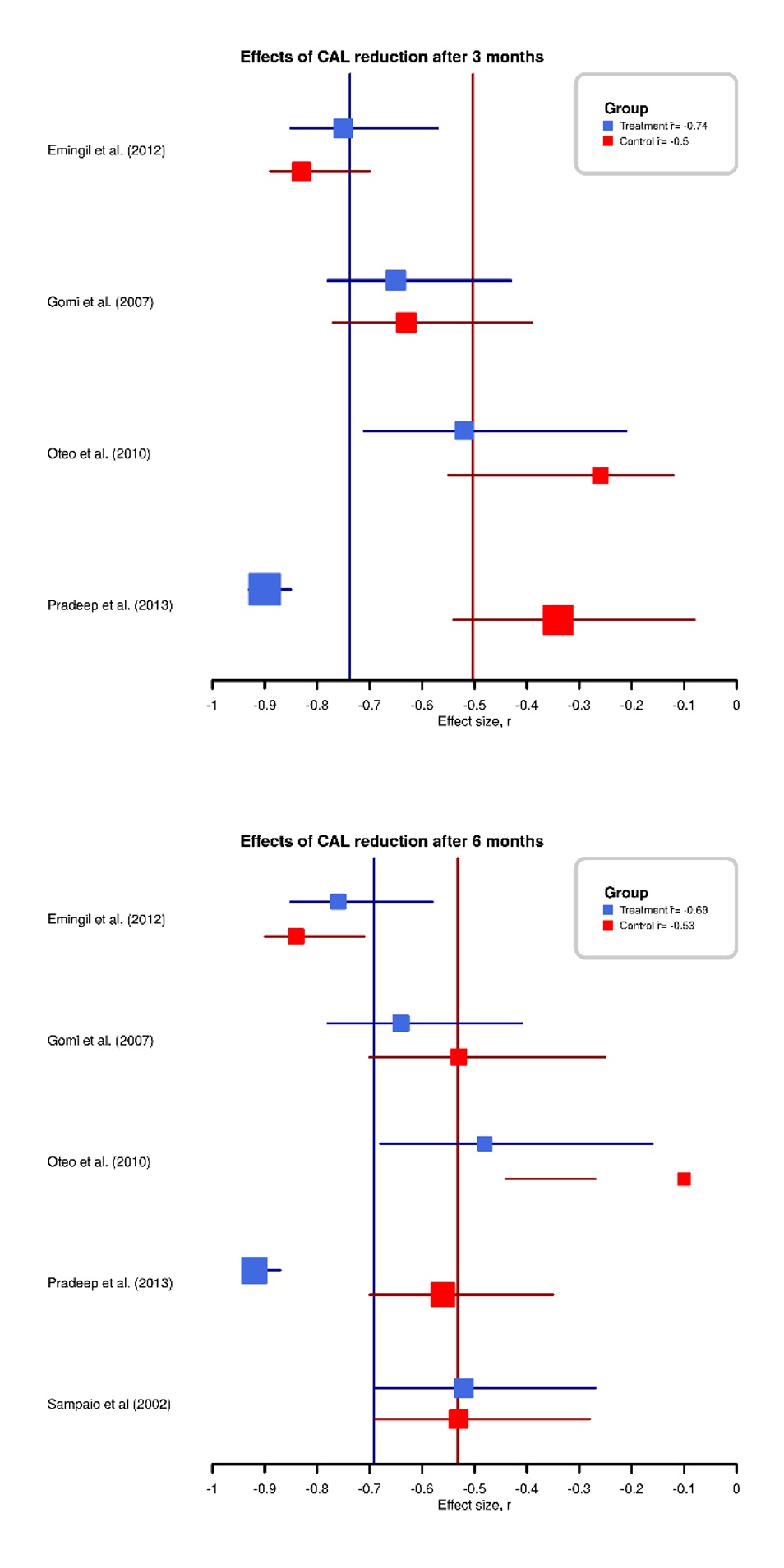
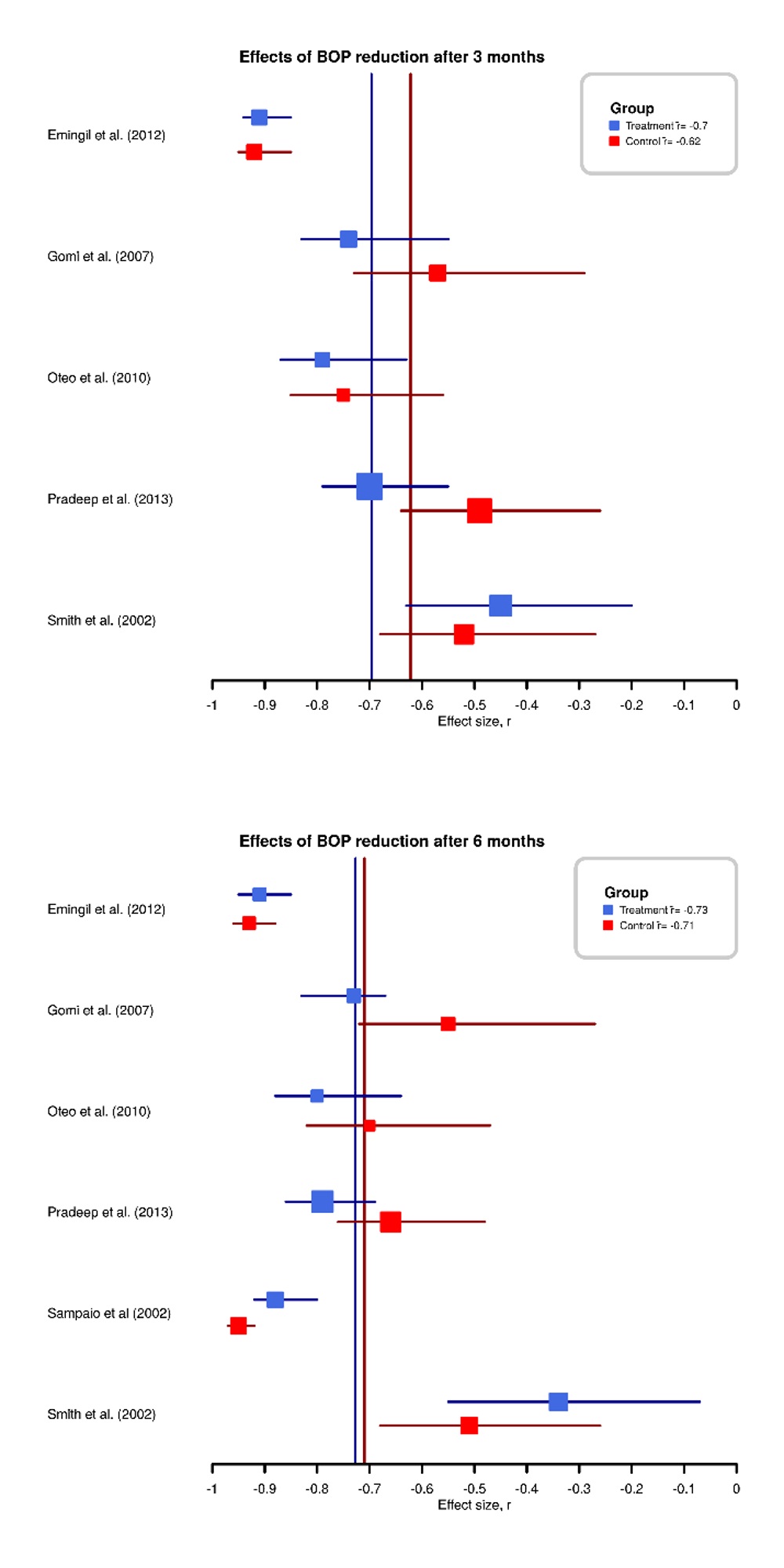
Results for PD, CAL and BOP [Table/Fig-4,5 and 6]: The treatment Group (TG, SRP+AZM) and the Control Group (CG, SRP) both exhibited significant improvements in the values recorded. Total two trials reported a greater therapeutic success within the TG in comparison with the CG. The results of CAL and BOP in three studies demonstrated a greater clinical improvement in the TG compared with the CG [31–33]. Both groups showed an improvement in values in all of the reviewed trials by larger effects for the TG [Table/Fig-7,8].
Forest plot of PD reduction after 3 and 6 months.
Forest plot of CAL reduction after 3 and 6 months.
Forest plot of BOP reduction after 3 and 6 months.
Effect sizes (r) of the changes of the clinical variables between the baseline and the follow-up measurements (3 and 6 months) for the treatment-groups.
| Study | BOP | PD | CAL | PI | MB |
|---|
| 3 months | 6 months | 3 months | 6 months | 3 months | 6 months | 3 months | 6 months | 3 months | 6 months |
|---|
| Emingil et al., (2012)[30] (n = 16) | -0.91 | -4.49 | -0.88 | -0.89 | -0.75 | -0.76 | -0.98 | -0.99 | - | - |
| Gomi et al., (2007)[31] (n = 17) | -0.74 | -2.12 | -0.75 | -0.66 | -0.65 | -0.64 | - | - | -0.11 | - |
| Oteo et al., (2010)[32] (n = 15) | -0.79 | -2.64 | -0.72 | -0.68 | -0.52 | -0.48 | -0.80 | -0.82 | -0.30 | - |
| Pradeep et al., (2013)[33] (n = 28) | -0.70 | -2.61 | -0.77 | -0.88 | -0.90 | -0.92 | -0.72 | -0.90 | - | - |
| Sampaio et al., (2011)[34] (n = 20) | - | -3.65 | - | -0.77 | - | -0.52 | - | -0.80 | - | - |
| Smith et al., (2002)[35] (n = 23) | -0.45 | -0.73 | - | - | - | - | -0.69 | -0.68 | - | - |
Note: N = sample size; BOP = Bleeding on Probing; CAL = Clinical Attachment Level; PD = Pocket Depth; PI = Plaque Index; MB = Microbiology.
Effect sizes (r) of the changes of the clinical variables between the baseline and the follow-up measurements (3 and 6 months) for the control groups.
| Study | BOP | PD | CAL | PI | MB |
|---|
| 3 months | 6 months | 3 months | 6 months | 3 months | 6 months | 3 months | 6 months | 3 months | 6 months |
|---|
| Emingil et al., (2012)[30] (n = 16) | -0.92 | -0.93 | -0.92 | -0.93 | -0.83 | -0.84 | -0.95 | -0.97 | - | - |
| Gomi et al., (2007)[31] (n = 17) | -0.57 | -0.55 | -0.57 | -0.57 | -0.63 | -0.53 | - | - | -0.16 | - |
| Oteo et al., (2010)[32] (n = 15) | -0.75 | -0.70 | -0.35 | -0.25 | -0.26 | -0.10 | -0.70 | -0.71 | 0.09 | - |
| Pradeep et al., (2013)[33] (n = 28) | -0.49 | -0.66 | -0.53 | -0.51 | -0.34 | -0.56 | -0.55 | -0.70 | - | - |
| Sampaio et al., (2011)[34] (n = 20) | - | -0.95 | - | -0.84 | - | -0.53 | - | -0.82 | - | - |
| Smith et al., (2002)[35] (n = 23) | -0.52 | -0.51 | - | - | - | - | -0.61 | -0.72 | - | - |
Note: N = sample size; BOP = Bleeding on Probing; CAL = Clinical Attachment Level; PD = Pocket Depth; PI = Plaque Index; MB = Microbiology.
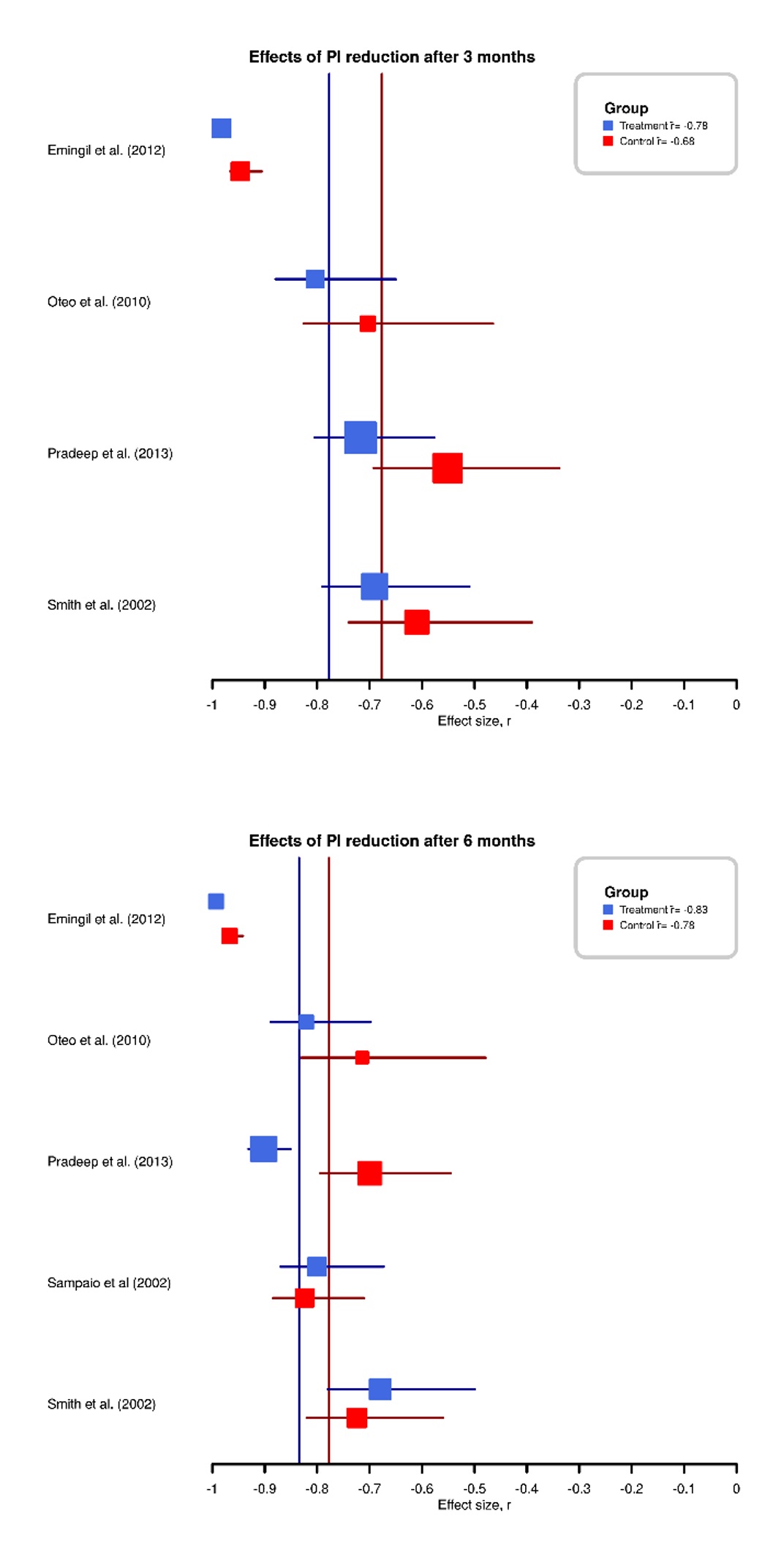
Consideration of the PI [Table/Fig-9]: One trial did not succeed in extracting any plaque values [31]. The remaining five trials did not permit a homogenous interpretation. The PI values improved in all studies up to the six-month follow-up, but in two studies the CG achieved better values, and in three studies TG recorded better values [Table/Fig-7,8].
Forest plot of PI reduction after 3 and 6 months.
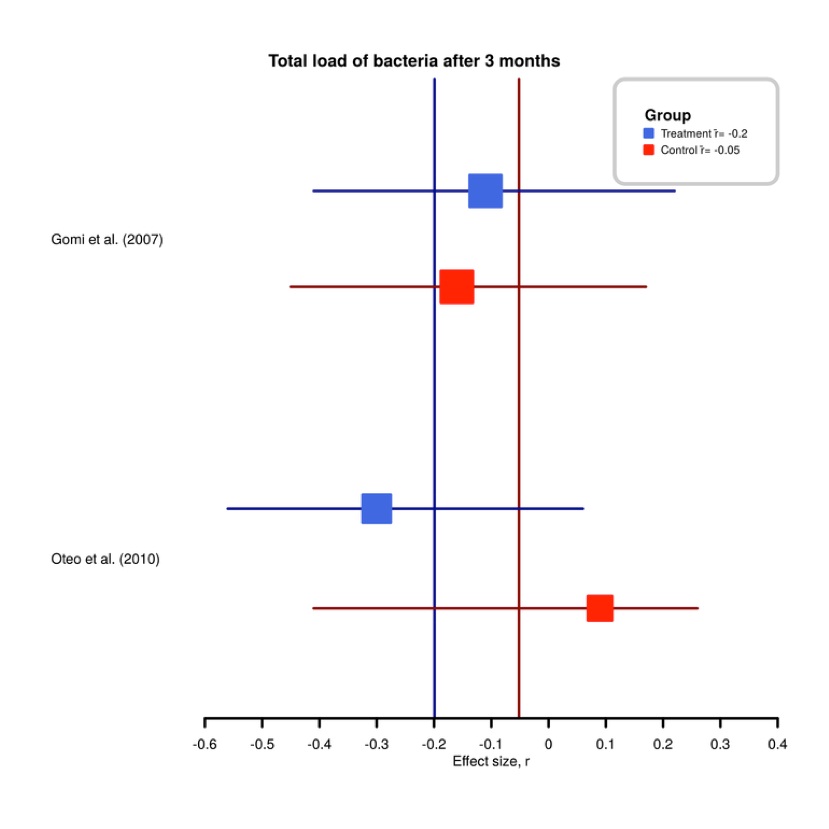
Total bacterial load [Table/Fig-10]: Microbiological examinations were conducted in two trials [31,32]. In this respect, it was demonstrated in one trial that a significant reduction in P. gingivalis took place (p≤0.01) [32]. The frequency of detection of P. gingivalis was reduced noticeable (p≤0.01) in the TG after one, three and six months. In contrast, the bacterial burden remained approximately constant throughout the examination period in the second trial [32].
Forest plot of total bacterial load reduction after 3 months.
Discussion
This systematic review and meta-analysis dealt with the question as to a positive effect ensuing from the systemic administration and local drug delivery of the antibiotic AZM in the nonsurgical treatment of periodontitis, compared with SRP on its own [33]. Following review of the trials, six trials continued to satisfy the inclusion criteria. A meta-analysis was possible due to the satisfactory homogeneity of the trials. Moreover, the result of this meta-analysis and review corresponds with a previously conducted review paper [36]. The data situation in the trials included, reveals substantial differences. The six included studies exhibit differences in the following aspects: Study size; population composition; statistical methods of evaluation; risk of bias; AZM dosage; time of AZM administration; time of SRP; and administration of a placebo. It is nevertheless possible to recognise a trend if one considers the effect magnitudes, and divides the effect magnitudes into minor effect (r value from 0.1), moderate effect (r value from 0.3) and major effect (r value from 0.5) in respect to the relevant clinical parameters [24].
In order to maintain a measure of comparability of the improvements of the clinical parameters of both groups in the course of time, it is important to avoid a difference of these parameters (e.g., BOP, PD etc.) at baseline. If one group starts with higher scores, they have a greater chance to show better improvements. For this reason comparable groups are vital. Almost all authors considered this issue. Only one study dealt with statistical significant differences of BOP and PI between the groups at baseline (other parameters showed no difference at baseline) [32]. This drawback should be taken in account when interpreting the effects.
The criteria for including studies in this meta-analysis were presented in previous section. Due to the fact that most authors reported means and standard deviations at the different dates, we used these parameters for calculating effect sizes [Table/Fig-7,8]. As we dealt with a within-subject design, it should be noted that this isn’t the ideal approach. The better alternative would have been using the means of the differences between the investigated dates and its standard deviations. Alternatively t-values could be used. Unfortunately only two authors reported this information. Because the two approaches lead to different effect sizes, only the presented back-up method was used. As we used the means and standard deviations for all calculations, the comparability of the effect sizes in this meta-analysis is guaranteed. Nevertheless this limitation should be kept in mind when comparing the presented results with other studies or meta-analyses.
The reduction in PDs after six months revealed a moderate to major effect in the TG and also the CG. The TG recorded better values than the CG in three of the trials. The most significant difference was ascertained in the trial involving local application of AZM.
The meta-analysis also ascertained a major difference between the groups in respect to the CAL. Hence, it is possible that the local application of 0.5% AZM gel has a more positive effect compared with the systemic administration. The PD and CAL improved in 75% of the trials after three months. This applies in equal measure to aggressive and chronic periodontitis. In one study the results were more pronounced in respect to pockets greater than 3mm [30]. Earlier review papers have indicated a positive effect of adjuvant AZM administration in the nonsurgical treatment of periodontitis [9,10]. The low volume of data obtained in respect to aggressive periodontitis patients does not permit any precise assessment of the results.
Certain variations in the study design become apparent if one considers the manner in which SRP is performed. The variations refer to the number of treatment sessions (1-6 sessions) and also the intervals between the individual appointments (1-4 weeks). This necessitates critical questioning of the baseline data. The possible benefits resulting from systemic and adjuvant administration of AZM must be defined more precisely in respect to the treatment protocol.
In terms of the length of antibiotic administration, only one trial documented a five-day antibiotic administration [34]. This trial used 500mg of antibiotics over five days. The SRP was administered in four up to six sessions, and antibiotic treatment started after the final SRP session. This study did not reveal any statistically significant benefits of the AZM administration. One could assume in this respect that the long duration of treatment may already have led to significant improvement during the phase of SRP. Moreover, this trial involved more frequent complications such as diarrhoea, headaches, metallic taste or insomnia due to the longer period of antibiotic treatment. Half of the six trials described side-effects [31,32,34]. The earlier trials described comparatively fewer side-effects when compared with the antibiotic gold standard (amoxicillin & metronidazole) [37]. In respect to the times of AZM administration, one trial commenced administration of adjuvant AZM at the start of treatment [31]. The antibiotic administration in the other trials took place after the final SRP session. Two of the six trials [30,34] did not record any greater improvement in the clinical parameters of the TG compared with the CG. The late time of antibiotic administration may be a reason for this. The absorption process in the defence cells and the slow released were confirmed in these results [38,39].
AZM concentration in the inflamed periodontal tissue verifiably falls from 50% to 20% between one week post-SRP and two weeks post-SRP [31]. Based on this information, it is sensible to terminate mechanical debridement at the earliest opportunity in order to preserve a high concentration of antibiotic in the relevant tissue during the process of biofilm elimination. Trial results indicate that application over three days is superior to application over five days in respect of the bacterial healing rates [40].
Limitation
On the other hand there exist clear limitations regarding different study designs and composition of the investigated population betweens the studies. Moreover it has to be mentioned that there is no generally accepted definition of periodontal disease and examination. For future growing resistance of present used antibiotics and contraindications, AZM may be possible as alternative administered antibiotic drug in combination with SRP in patients with chronic periodontitis.
Conclusion
Our review and meta-analysis suggest substantial benefit of administration of AZM in therapy of patients with adult periodontitis. The use of AZM as an adjuvant to SRP for generalized chronic periodontitis improves clinical and microbiological findings compared to SRP therapy alone. Further studies regarding the adjunctive use of AZM in patients with aggressive periodontitis are needed.
Contribution
The First and the Second (AR & JH) author equally contributed in preparation of the manuscript, literature research, translation, internal communication, proof reading and publication process. Third author(AS) contributed in statistical analysis and creation of tables. Fourth Author (FS) was the head for statistical analysis and correction. Fifth Author (HJ) was the head for clinical research and allocation of the subjects.
Note: RCT = Randomized Clinical Trial; BOP = Bleeding on Probing; CAL = Clinical Attachment Level; PD = Pocket Depth; PI = Plaque Index; MB = Microbiology; N = Sample Size; SRP = Scaling and Root Planing.
Note: N = sample size; BOP = Bleeding on Probing; CAL = Clinical Attachment Level; PD = Pocket Depth; PI = Plaque Index; MB = Microbiology.
Note: N = sample size; BOP = Bleeding on Probing; CAL = Clinical Attachment Level; PD = Pocket Depth; PI = Plaque Index; MB = Microbiology.