Angioleiomyoma of the Plantar-Medial Arch: A Case Report
Omar Baarini1, Mark Gilheany2
1 Senior Registrar, Australasian College of Podiatric Surgeons, Australia.
2 Fellow, Australasian College of Podiatric Surgeons, Australia.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Omar Baarini, Senior Registrar, Australasian College of Podiatric Surgeons, PO BOX 248, Collins Street West Melbourne, VIC 8007, Australia.
E-mail: obaarini@hotmail.com
An angioleiomyoma is a benign soft tissue tumour that arises from smooth muscle layer of blood vessels. The true aetiology of these masses is largely unknown and quite often may not be associated with pain. This paper illustrates the occurrence of an angioleiomyoma in the medial arch of the foot, a previously unreported location. Significant delay occurred in the patient being referred for specialist consultation, after attending numerous general practitioners for management. This highlighted the need for ongoing publication for case reports of this nature. The patient underwent excision with no recurrence of the lesion reported at 12 months. Often masses of this type may be left alone. However, when symptomatic simple excision will suffice where no other surrounding complication exists and where the mass is well encapsulated in the sub cutaneous area.
Leiomyomas, Subcutaneous/soft tissue tumour, Vascular leiomyomas
Case Report
A 51-year-old fast food store owner presented with a 2-year-old asymptomatic and slowly growing mass in the right mid foot in the region of the medial arch. The mass was initially described as a painless subcutaneous soft tissue tumour about 20mm in diameter. The general practitioner did not advise surgery initially as the mass was well encapsulated and not causing any pain [Table/Fig-1].
Encapsulated mass on mid foot.

The patient presented for Podiatric consultation for a second opinion. Of particular concern to the patient was the cosmetic appearance of the mass and the ongoing irritation in footwear. After clinical and radiographic assessment of the mass a decision to excise was made. Based on the imaging results full excisional biopsy was discussed with the patient and identified as suitable alternative to fine needle biopsy.
Clinical considerations in assessing the patient’s suitability for surgery in this case included a medical history of long standing well controlled non-insulin dependent diabetes mellitus and hypertension. Recent HbA1c results, as well as neurological and vascular assessment indicated the patient’s suitability for surgical excision of the tumour.
There was no history of previous trauma to the area. The patient was sent for X-ray and ultrasound. X-ray examination was insignificant, with no signs of any bone erosion secondary to mass pressure. Ultrasound examination reported a soft tissue tumour which was hypo echoic and hyper vascular in a well defined capsule. Reported diagnosis was fibroma or lipoma.
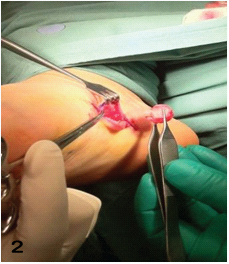
The mass was excised under mild sedation and a local anaesthetic block (10ml of 0.5% Bupivacaine); and was approached via a curvi-linear incision proximal to the lateral border. Sub cutaneous blunt dissection with a small curved artery forcep was utilised, exposing a well circumscribed solid mass [Table/Fig-2]. This allowed for sharp dissection and clean extraction of the tumour. The wound was closed with 3/0 Monocryl.
Excision of tumour for biopsy.
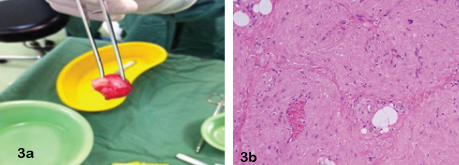
The mass was sent for histopathology testing of which two transverse slices were processed. The results reported an encapsulated mass (23x15x15 mm) with margins marked. A section showed a nodular lesion with the periphery of the nodule surrounded by a thin rim of mildly compressed fibrotic tissue. Proliferating within the nodule were numerous thick walled blood vessels and smooth muscle bundles. Scanty collections of adipocytes were also noted in neoplasm. The histopathology findings were consistent with Angioleiomyoma [Table/Fig-3a,b]. Healing proceeded without complication, and at 12 month review there was no evidence of regrowth.
(a) Mass identified as Angioleiomyoma. (b) Histopathology slide (Stain Haematoxylin & Eosilin with magnification X40)showing numerous thick walled blood vessels and smooth muscle bundles.
Discussion
Angioleiomyoma is a one of the three different forms of a leiomyoma, which may otherwise be known as vascular leiomyoma. These are uncommon and are categorized as a benign neoplasm that arise from smooth muscle layer of blood vessels [1,2]. They have been categorized histopathologically by a well-circumscribed dermal nodule surrounded by a compressed connective tissue and separated from it by clefts. Variable sized veins with muscular walls are present within the nodule and smooth muscle bundles extend tangentially from the periphery of the vessels. The lumina of the veins is rounded or slit like and as a rule angioleiomyoma only contain a small amount of collagen [3]. They frequently occur in extra-skeletal sites which include the ovaries, uterus, bladder, lung, and the gastrointestinal tract [4]. Other forms of leiomyoma include piloleiomyoma which arise from arrector pili muscles; and genital leiomyoma which arise from smooth muscles of the scrotum, vulva, or nipple [5]. Angioleiomyoma are twice as prevalent in women as men and effect middle aged population mainly; however they can be found throughout the body in male and female adults of all ages [4]. Approximately 50-70% of all the Angioleiomyoma found are within the lower limbs [6]. These masses account for approximately 4.4% of all benign soft tissue tumours [7]. The aetiology of the formation of this tumour is unknown, however factors such as trauma, infection, hormones and arteriovenous malformations have been discussed [5].
Differential diagnosis includes lipoma, fibroma, ganglions, schwannomas, cutaneous angiomyolipomas, glomus tumours and others [5]. Arteriogram, or a Doppler study may be used to determine arterial and venous anatomy adjacent to the mass. The tumour is rarely diagnosed until it is excised and histopathological examination conducted [8,9]. Pre operative planning is aided and often depends on the multiple imaging modalities, especially ultrasound, and MRI [3–5]. Although such imaging as ultrasound and MRI allow for visualisation of the mass for excision, and are helpful with assessing for the hypervascular characteristics of the mass; they are not specific, and the final diagnosis depends on histopathological examination [8–11].
Pain is not always associated with the presence of an Angioleiomyoma. However, about 60% of patients do report some kind of pain, which includes pressure pain, sharpness or pinching, which may be affected by temperature [2]. It has been hypothesised that the pain may be associated with local tissue anoxia, or due to the compression of local neural structures [6,12].
Complications such as secondary calcification, myxoid degeneration, hyalinization and malignant transformation have been reported [4].
Simple excision and biopsy is often all that is needed [2,8–10]. The decision to proceed to surgery often depends on the size of the lesion and the severity of the symptoms [4]. Once excised, malignant recurrence of the mass is noted to be extremely rare [13]. In cases of recurrence, it has been discussed that the new lesion should be removed widely and treated like other low grade malignancies [7,12].
Conclusion
Angioleiomyoma is a relatively uncommon benign subcutaneous soft tissue mass that most often occurs in the extremities. Simple excision and histopathology is recommended, especially in cases where patients report pain or other difficulties associated with the protruding mass. Imaging can be of assistance in visualizing the mass and its surrounding structures prior to surgical excision. This report presented a case where this was evident with a successful outcome and no recurrence of the tumour.
[1]. Heffernan MP, Smoller BR, Kohler S, Cutaneous epitheliod angioleiomyomaAmerican Journal of Dermatopathology 1998 20:213-17. [Google Scholar]
[2]. Requena L, Baran R, Digital Angioleiomyoma: an uncommon neoplasmJournal American Academy Dermatol 1993 29:1043-44. [Google Scholar]
[3]. Requena L, Sangueza OP, Cutaneous vascular proliferations. Part IIIJournal American Academy Dermatol 1998 38:159-60. [Google Scholar]
[4]. Gajanthodi S, Rai R, Chaudhry RK, Vascular Leiomyoma of FootJournal of Clinical and Diagnostic Research 2013 7(3):571-72. [Google Scholar]
[5]. Dominguez-Cherit J, Brandariz A, Distal digital angioleiomyoma: a case report and review of the literatureThe International Society of Dermatology 2003 42:141-43. [Google Scholar]
[6]. Hanft JR, Carbonell JA, Hao DQ, Angioleiomyoma of the lower extremityJAPMA 1997 87(8):388-91. [Google Scholar]
[7]. Murata H, Matsui T, Naoyuki H, Tomoya S, Eiichi K, Toshikazu K, Angioleiomyoma with Calcification of the Heel: Report of Two CasesFoot Ankle Int 2007 28:1021-25. [Google Scholar]
[8]. Woo KS, Kim SH, Kim HS, Cho PD, Clinical Experience with Treatment of AngioleiomyomaArchives of Plastic Surgery 2014 41:374-78. [Google Scholar]
[9]. Park HJ, Kim SS, Lee SY, Choi YJ, Chung EC, Rho MH, Sonographic Appearances of Soft Tissue Angioleiomyomas: Differences From Other Circumscribed Soft Tissue Hypervascular TumoursJournal of Ultrasound Medicine 2012 31:1589-95. [Google Scholar]
[10]. Yoo HJ, Choi AJ, Chung JH, Oh JH, Lee GK, Choi JY, Angioleiomyoma in Soft tissue of extremities: MRI FindingsAmerican Journal of Roentgenology 2009 :W291-94. [Google Scholar]
[11]. Nicolai P, Redaelli de Zinis LO, Facchetti F, Craniofacial resection of vascular leiomyoma of the nasal cavityAmerican Journal Otolaryngal 1996 17:370-77. [Google Scholar]
[12]. Yates B, Angioleiomyoma: clinical presentation and surgical managementFoot Ankle Int 2001 22:670-73. [Google Scholar]
[13]. Herren DB, Zimmermann A, Buchler U, Vascular leimyoma in an index finger undergoing malignant transformationJournal of Hand Surgery 1995 20:484-87. [Google Scholar]