An Unusual Case of Extensive Lattice Degeneration and Retinal Detachment
David J. Mathew1, Saurabh Kumar Sarma2, Jennifer V. Basaiawmoit3
1 Consultant Ophthalmologist, Bansara Eye Care Centre, Laitumkhrah, Shillong, India.
2 Senior Consultant Ophthalmologist, Bansara Eye Care Centre, Laitumkhrah, Shillong, India.
3 Medical Director, Bansara Eye Care Centre, Laitumkhrah, Shillong, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. David J. Mathew, Consultant Ophthalmologist, Bansara Eye Care Centre, Lady Veronica Lane, Laitumkhrah, Shillong-793003, Meghalaya, India.
E-mail: davidmathew123@gmail.com
Lattice degeneration of the retina is not infrequently encountered on a dilated retinal examination and many of them do not need any intervention. We report a case of atypical lattice degeneration variant with peripheral retinal detachment. An asymptomatic 35-year-old lady with minimal refractive error was found to have extensive lattice degeneration, peripheral retinal detachment and fibrotic changes peripherally with elevation of retinal vessels on dilated retinal examination. There were also areas of white without pressure, chorioretinal scarring and retinal breaks. All the changes were limited to beyond the equator but were found to span 360 degrees. She was treated with barrage laser all around to prevent extension of the retinal detachment posteriorly. She remained stable till her latest follow-up two years after the barrage laser. This case is reported for its rarity with a discussion of the probable differential diagnoses. To the best of our knowledge, this is the first report of such findings in lattice degeneration.
Barrage laser, Peripheral retinal detachment, Wagner’s disease
Case Report
A 35-year-old Asian Indian housewife presented to the Department of Ophthalmology for a regular eye check-up. She was told elsewhere that she has a retinal problem, the details of which were not known to her. She had been using glasses for the last 10 years. There was no history of flashes or floaters, redness, pain or sudden loss of vision in the past. She did not undergo any laser or surgical treatment in the past. She was born of a non-consanguineous marriage and birth history was reportedly normal. There was no family history of retinal diseases.
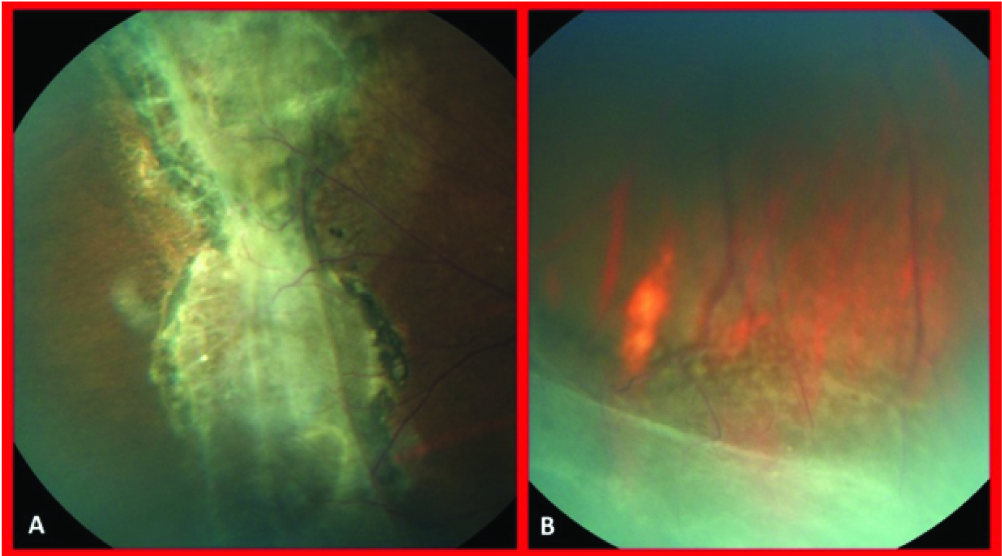
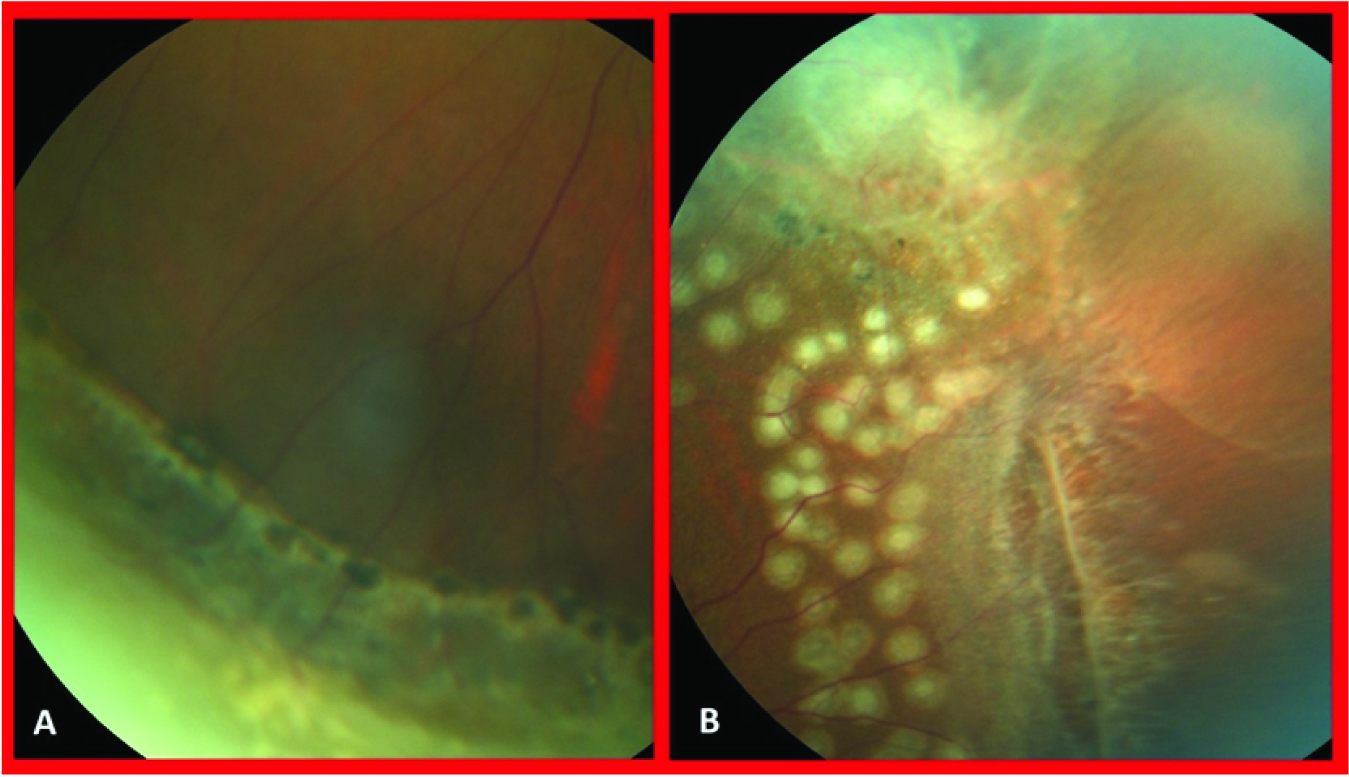
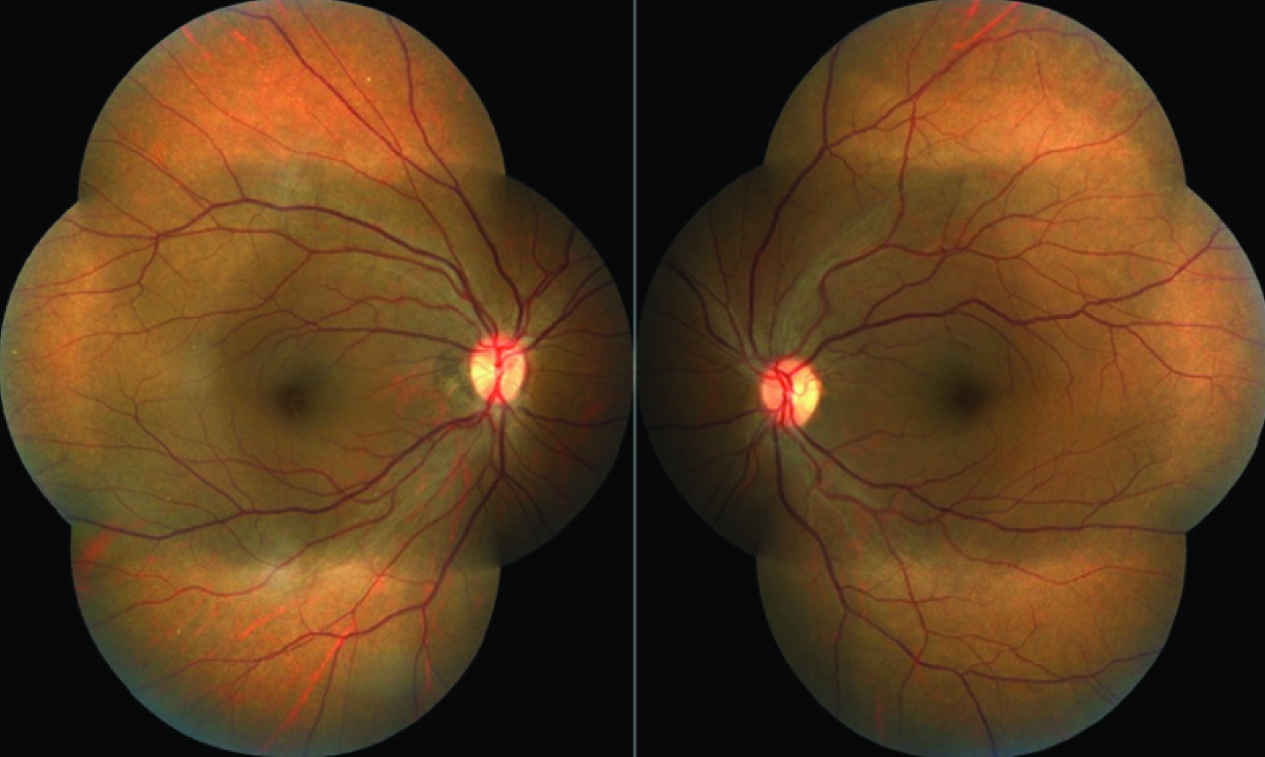
On examination, she had a best corrected visual acuity of 20/20 in both eyes using Snellen’s visual acuity chart with a correction of -0.50DC at 10° and +1.00DS / -1.00DC at 170° in the right and left eyes respectively. Anterior segment examination was within normal limits. There was no cataract. The vitreous was clear. On dilated examination, the retina showed fibrotic changes peripherally with elevation of retinal vessels due to retinal detachment. There were areas of white without pressure and retinal breaks as well [Table/Fig-1,2]. All the changes were limited to beyond the equator but were found to span 360 degrees. Chorioretinal scarring was present in some areas [Table/Fig-1a,2a] but there were other areas devoid of scarring [Table/Fig-1b] which carried the risk of extension of the retinal detachment. The posterior pole was within normal limits [Table/Fig-3]. There were no extra-ocular dysmorphic features, cleft or high arched palate, joint hypermobility or deafness.
(a) Fibrotic changes causing elevation of the retina, chorioretinal scarring and pigmentary changes. (b) Inferior peripheral retinal detachment with some spread posteriorly. Credits: Deepa and Banshanhi.
(a) Peripheral white without pressure with a clear posterior border marked by pigmentary changes. (b) Fibrotic changes (upper half), lattice degeneration with atrophy and retinal tear; fresh barrage laser marks are also seen. Credits: Deepa and Banshanhi.
The posterior pole in both eyes was within normal limits. Credits: Deepa and Banshanhi.
A 360° barrage laser using double frequency Neodynium: Yttrium Aluminium Garnet (Nd:YAG) laser (spot size 300μm, exposure duration 200 milliseconds, power 120-150mW) was done all around, in both eyes. Areas of retinal breaks were lasered adequately with three rows of laser spots [Table/Fig-2b]. On the latest follow-up at 2 years, there was no deterioration of vision, macular oedema, macular puckering or progression of retinal detachment.
Discussion
Lattice degeneration of the retina, also synonymous as circumferential, equatorial or palisade retinal degeneration is present in 6-8% of the general population. It is present in 30% of retinal detachments in phakic patients [1]. Lattice degeneration often takes the appearance of an elongated area of inner retinal thinning, its long axis tending to lie parallel to the ora serrata. Lattice may also be seen on either side of a major retinal vessel, following a perivascular pattern in Wagner or Stickler syndrome. Lesions that are located at or posterior to the equator tend to be larger. The base of the lesion has a moth-eaten uneven appearance and the overlying thin degenerating retina is often jagged [2,3]. White lines in a criss-crossing or fish-bone pattern may or may not be seen within the lesion, which renders the name “lattice” degeneration to this lesion. These white lines are in fact glial or hyaline sheathed vessels which may be occluded. These white lines are seen in 11.9 to 42.9% of patients with lattice degeneration [2]. Normal appearing retina exists between the lesion and the ora serrata as in this case. This may be confirmed in appropriate cases by scleral depression to differentiate lattice from a pigmented prominent vitreous base [3].
Retinal tears are present in upto 2.4% cases of lattice degeneration. They usually develop along the posterior and lateral edges of the lesion. In many such tears, an incomplete posterior vitreous detachment is present with its edge attached to the posterior margin of the lesion [4,5]. However, it was not observed in this case. Retinal detachment is seen in less than 1% of patients with lattice degeneration if the fellow eye did not have a retinal detachment [5,6]. However, with a history of retinal detachment in one eye, the risk of retinal detachment in the fellow eye over seven years is between 2-5% [7].
The lattice degeneration variant in this case resembled that of Wagner’s disease which does not usually have any systemic features in contrast to Stickler’s syndrome [8]. The common features that this case shared with Wagner’s disease were lattice degeneration, peripheral tractional detachment, chorioretinal atrophy and white without pressure. However, this case differs from Wagner’s disease in the fact that there was no family history, optic atrophy, avascular membranes, glaucoma, and cataract or perivascular pattern of lattice degeneration.
It was first described by Wagner in 1938 in a Swiss family. An empty vitreous cavity was noted in most patients. Peripheral tractional detachment was seen in 55% of older patients. The incidence of cataract and chorioretinal atrophic areas was found to increase with age [8,9].
Other differentials include erosive vitreoretinopathy, Goldmann-Favre vitreoretinal dystrophy, familial exudative vitreoretinopathy, autosomal dominant neovascular inflammatory vitreoretinopathy and autosomal dominant vitreoretinochoroidopathy.
Erosive vitreoretinopathy is an autosomal dominant inherited disorder characterized by “erosion” of the retinal pigment epithelium causing visualization of the choroidal vessels and progressive drop in vision, scotomas, sheathing of vessels and bone-spicule pigmentation. This entity has a higher rate of retinal detachment than Wagner’s disease but resembles it in the fact that there are no extra-ocular features [10].
Goldmann-Favre disease is autosomal recessively inherited and is marked by drop in vision in the first two decades of life due to macular retinoschisis. Other features include chorioretinal atrophy, peripheral retinoschisis, vitreous veils and retinitis pigmentosa-like pigmentation [11].
Familial exudative vitreoretinopathy shares many features with retinopathy of prematurity but there is no history of prematurity and family members are usually affected. It is known to present asymmetrically in both eyes and is characterized by a peripheral avascular zone, lipid exudation, temporal dragging of the fovea, falciform fold attached to the disc and retinal detachment [12].
Autosomal dominant neovascular inflammatory vitreoretinopathy and autosomal dominant vitreoretinochoroidopathy are characterized by vitritis and cystoid macular oedema [13]. These were not seen in this case.
Treatment is indicated in symptomatic patients, positive family history of retinal detachment, retinal detachment in the fellow eye, trauma related retinal breaks, myopia and clinical progression of detachment [1,3]. In this case, the lattice was extensive with retinal detachment at presentation. The chorioretinal scars that were seen at the posterior edges of the lattice in some areas might have acted as a barrier preventing further posterior extension. However, there were other areas which were devoid of such a “barrier”. Since the lesion was present continuously all around, the laser spots could not be connected to the ora or placed enclosing the areas devoid of chorioretinal scarring. Hence, a 360° barrage was carried out. It should be kept in mind that prophylactic laser treatment may lead to formation of premacular fibrosis, giant retinal tear, macular hole and even increase the risk of retinal detachment in some cases [14].
Conclusion
Lattice degeneration though commonly encountered, can vary in its appearance. Though most cases can be observed without intervention, some present a real risk of retinal detachment. These cases require barrage laser or cryotherapy to seal off the affected areas. In this case, there was already a peripheral retinal detachment which required laser treatment. This case report illustrates a rare variant of atypical extensive lattice degeneration. To the best of our knowledge, this is the first report of such findings in lattice degeneration. Association with syndromes like Stickler’s syndrome and Wagner’s disease must be kept in mind when one encounters such atypical lattice degeneration.
[1]. Wilkinson CP, Interventions for asymptomatic retinal breaks and lattice degeneration for preventing retinal detachmentCochrane Database Syst Rev 2014 9:CD003170 [Google Scholar]
[2]. Byer NE, Lattice degeneration of the retinaSurv Ophthalmol 1979 23(4):213-48. [Google Scholar]
[3]. Jones W, Lattice degenerationIn: Peripheral Ocular Fundus 2007 3rd edMissouriButterworth-Heinemann, Elsevier:88-99. [Google Scholar]
[4]. Straatsma BR, Zeegen PD, Foos RY, Feman SS, Shabo AL, XXX Edward Jackson Memorial Lecture. Lattice degeneration of the retinaTrans Am Acad Ophthalmol Otolaryngol 1974 78(2):OP87-113. [Google Scholar]
[5]. Byer NE, Changes in and prognosis of lattice degeneration of the retinaTrans Am Acad Ophthalmol Otolaryngol 1974 78(2):OP114-25. [Google Scholar]
[6]. Byer NE, Long-term natural history of lattice degeneration of the retinaOphthalmology 1989 96(9):1396-1401-02 [Google Scholar]
[7]. Folk JC, Arrindell EL, Klugman MR, The fellow eye of patients with phakic lattice retinal detachmentOphthalmology 1989 96(1):72-79. [Google Scholar]
[8]. Maumenee IH, Stoll HU, Mets MB, The Wagner syndrome versus hereditary arthroophthalmopathyTrans Am Ophthalmol Soc 1982 80:349-65. [Google Scholar]
[9]. Graemiger RA, Niemeyer G, Schneeberger SA, Messmer EP, Wagner vitreoretinal degeneration. Follow-up of the original pedigreeOphthalmology 1995 102(12):1830-39. [Google Scholar]
[10]. Brown DM, Kimura AE, Weingeist TA, Stone EM, Erosive vitreoretinopathy. A new clinical entityOphthalmology 1994 101(4):694-704. [Google Scholar]
[11]. Batioğlu F, Goldmann-Favre vitreoretinal degenerationEur J Ophthalmol 2003 13(3):307-10. [Google Scholar]
[12]. Shukla D, Singh J, Sudheer G, Soman M, John RK, Ramasamy K, Familial exudative vitreoretinopathy (fevr). Clinical profile and managementIndian Journal of Ophthalmology 2003 51(4):323 [Google Scholar]
[13]. Kyung SE, Chang MH, Ji JY, A case of erosive vitreoretinopathyKorean Journal of Ophthalmology 2002 16(1):47 [Google Scholar]
[14]. Byer N, Rethinking prophylactic treatment of retinal detachmentIn: Advances in Vitreoretinal Surgery 1991 New YorkOphthalmic Communications Society:399-411. [Google Scholar]