Esthesioneuroblastomas: Reservations and Recommendations
Rajesh Nair1, Bhavna Nayal2, Vinod Kumar3, Padmapriya Jaiprakash4
1 Senior Registrar, Department of Neurosurgery, Kasturba Medical College, Manipal, Karnataka, India.
2 Associate Professor, Department of Pathology, Kasturba Medical College, Manipal, Karnataka, India.
3 Associate Professor, Department of Neurosurgery, Kasturba Medical College, Manipal, Karnataka, India.
4 Associate Professor, Department of Pathology, Kasturba Medical College, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rajesh Nair, Associate Professor, Department of Pathology, Kasturba Medical College, Manipal-576104, Karnataka, India.
E-mail: rajeshnair39@yahoo.com
Neuroectodermal tumour has a wide range of biological activity that ranges from an indolent course to local recurrence and rapid widespread metastasis.
We describe, herewith, 2 patients with Esthesioneuroblastomas (ENB) who had varied atypical clinical presentation. The first case presented with Intracranial Pressure (ICP) headache and acute visual deterioration with radiology revealing an extra axial lesion with extension into the nasal cavity while the second case presented with nasal congestion and progressive headache of long duration. We review the unusual characteristics that may uncommonly occur in ENBs and elaborate regarding which of these must be considered when evaluating patients with this malignancy.
Intracranial tumours, Nasal tumours, Olfactory neuroblastoma
Case Report
Case 1
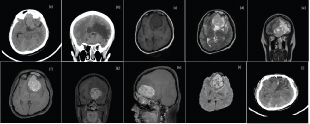
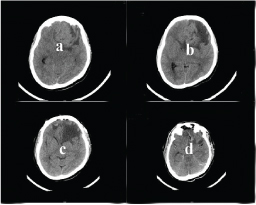
A 30-year-old lady, 5 months post partum, presented with persistent holocranial headache of 15 days duration. The headache was associated with blurring of vision and diplopia since 7 days and vomiting since 3 days. She seemed drowsy on neurological assessment and was disoriented with irrelevant speech. Fundus showed Grade 1 papilloedema bilaterally, with finger counting at 3 feet bilaterally, on confrontation technique. Visual field charting was not possible because of the patient being neurologically obtunded. Plain Computed Tomographic (CT) scan of the brain [Table/Fig-1] showed a well defined, iso to hyperdense lesion in the left basifrontal measuring approximately 4.2x5.4x5.5cm, abutting the roof the ethmoid sinuses and left lesser wing of the sphenoid with significant perilesional oedema and mass effect with midline shift of 8mm. Bone window showed destruction of the cribriform plate bilaterally with involvement of the left sphenoid, ethmoid sinuses and the left nasal cavity. Preoperative Magentic Resonance Imaging (MRI) [Table/Fig-1] revealed a well-circumscribed extra axial lesion, hypointense on T1W, hyperintense on T2W in the left basifrontal region appearing to arise from the olfactory region. On T1W contrast the lesion showed heterogenous enhancement. Mass effect was seen in the form of displacement of the frontal lobe superiorly with abutment of the anterior cerebral arteries to the right. Postero-inferiorly the lesion was seen in close proximity to the C7 segment of left internal carotid artery, M1 segment of left middle cerebral artery with moderate vasogenic oedema causing parafalcine herniation. She was taken up for a bifrontal craniotomy with gross total excision of the tumour with basal repair [Table/Fig-2] and exteriorization of the frontal sinus. Postoperative CT scan showed gross total excision of the tumour with an uneventful postoperative period [Table/Fig-3]. Her vision improved postoperatively and she was discharged on postop day 7 and was asymptomatic on follow-up at 3 weeks.
Preoperative imaging (Case 1) Plain CT brain, axial and coronal: (a,b) showing a 4.2x5.4x5.5cm mass with few cystic areas noted mainly in the left basifrontal region with perilesional oedema and extending into the left nasal cavity, sphenoid and ethmoid sinuses. MRI Brain (preoperative) showing a left basifrontal and midline, extra-axial lesion, axial section, hypo on T1W; (c) hyperintense on T2W; (d) with perilesional oedema on FLAIR, coronal section (e). The lesion had heterogenous enhancement on contrast; (f,g,h – axial, coronal, sagittal) with diffusion restriction; (i) The lesion seemed to arise from the left nasal cavity with invasion into the ethmoid and sphenoid sinus with destruction of the cribriform plate, as seen on the sagittal section of the MRI; (h) The imaging features suggested a possibility of Esthesioneuroblastoma; (j) shows the postop CT scan, axial section, with gross total excision of the tumour with significant residual oedema.
Intraoperative images: (a) Bifrontal craniotomy and excision of tumour, seen after cutting the falx and superior saggital sinus anteriorly and retracting the frontal lobe. Frontal sinus has been exteriorized; (b) Showing the anterior cranial fossa floor post gross total excision with; (c) exteriorization of the frontal sinus and denuding the mucosa and obliterating the sinus with bone wax.

Post op and preop CT of (Case1) showing the preop axial CT in the upper section (a,b), with a hypo to isodense lesion with perilesional oedema and the lower two sections (cd) showing postop changes and gross total excision of the tumour.
Case 2
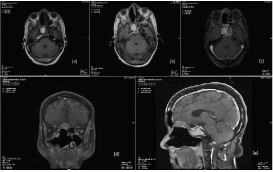
A 67-year-old lady, presented to the ENT outpatient department with a history of nasal congestion and progressive headache since 10 years. On clinical examination she had a pale lobulated mass protruding through the superior aspect of the nasal cavity and seemed to involve the cribriform plate of the right nostril. Preoperative haematological investigations were within normal limits. A biopsy was done which preferred a diagnosis of esthesioneuroblastoma. MRI [Table/Fig-4] of the brain revealed a small well-defined lobulated extra-axial lesion in the right subfrontal region abutting the gyrus rectus superiorly and floor of anterior cranial fossa inferiorly with cortical discontinuity seen with bony destruction of the right cribriform plate. She was referred to neurosurgery for further management.
Preoperative MRI Scan of the brain, post transnasal excision of the nasal tumour (Case 2) showing a small well defined lobulated extra-axial lesion (hyperintense on T1: (a) hyperintense on FLAIR; (b) and intense post contrast enhancement; (c) axial sections measuring ~ 1.7 x 1.5 x 2.6cm is seen with a broad base to the dura in the right subfrontal region abutting the right gyrus rectus superiorly and floor of anterior cranial fossa inferiorly.
Cortical discontinuity with evidence of bony destruction of the right cribriform plate was noted. The contrast series shows intense enhancement on coronal; (d) and sagittal; (e) sections which show and involvement of the right half of the anterior cranial fossa floor with posterior extension into the sella.
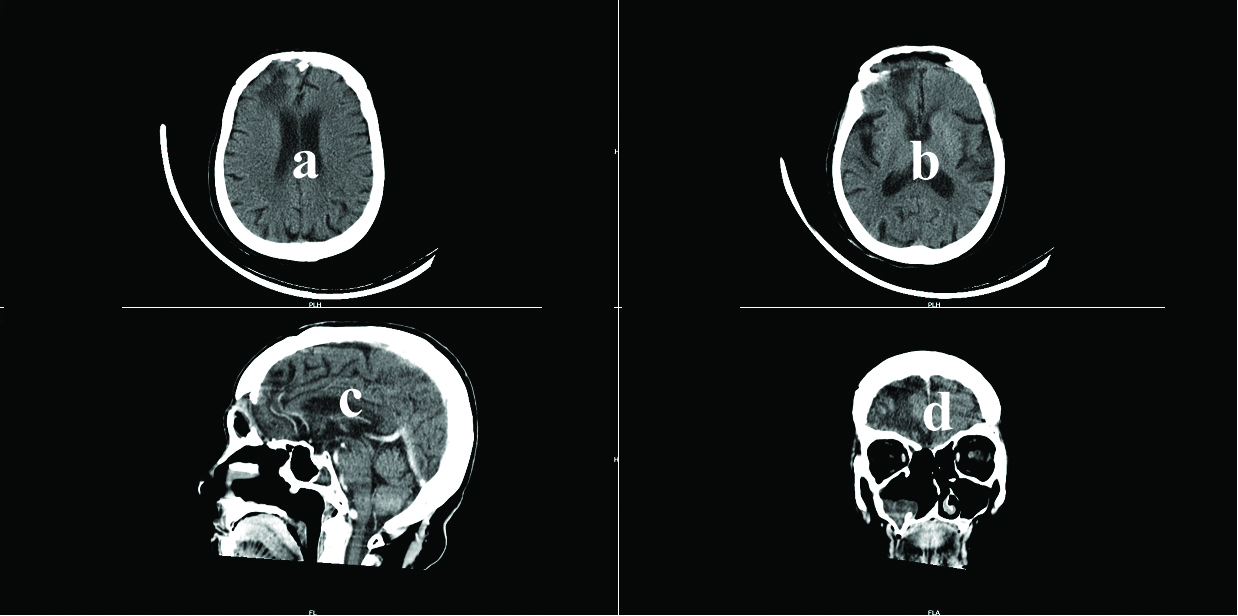
A neurological examination was unremarkable except for anosmia. She was planned for a two-staged procedure for excision of the tumour. The first stage was an endoscopic transnasal approach and the tumour was excised upto the cribriform plate. Once satisfactory recovery had occurred, the patient was subjected to a bifrontal craniotomy and gross total resection of the tumour along with the olfactory bulbs. A thorough anterior cranial fossa carpeting with pericranial graft was done [Table/Fig-5]. The patient had a small transient CSF leak, postoperatively, which settled after a week of conservative management. She also developed transient abulia, due to frontal lobe retraction during surgery, which resolved after two weeks of conservative inpatient care. On discharge, she was symptom free, however she had anosmia and loss of taste, which persisted at three and six weeks follow up.
Postoperative Plain CT scan of the brain (Case 2) {Axial, (a,b) contrast sagittal (b) and contrast coronal (c)} sections showing total excision of the tumour, the inner table of the frontal sinus has been removed for exteriorization of the sinus and anterior cranial fossa carpeting as seen on section b and c.
Histopathology
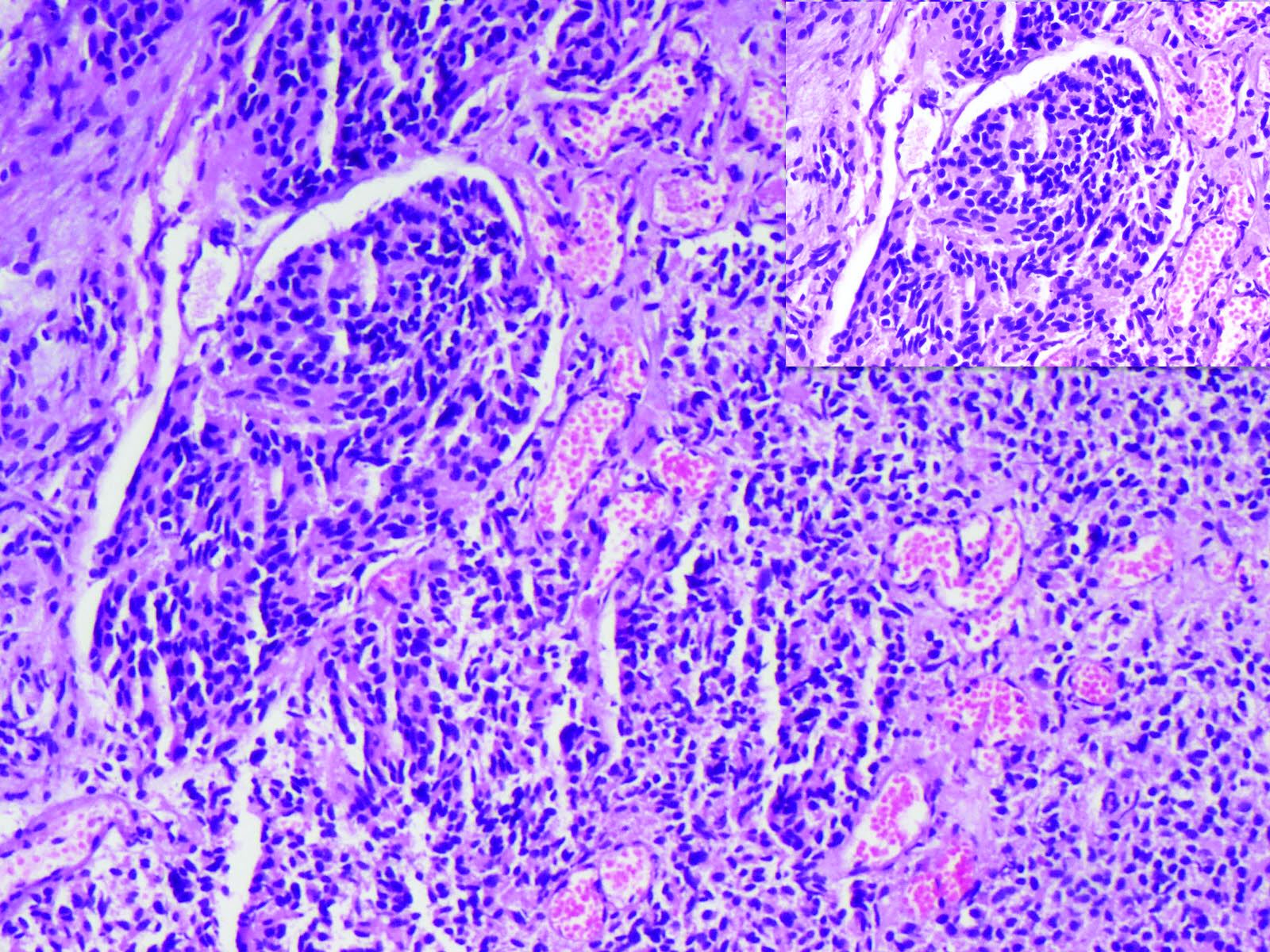
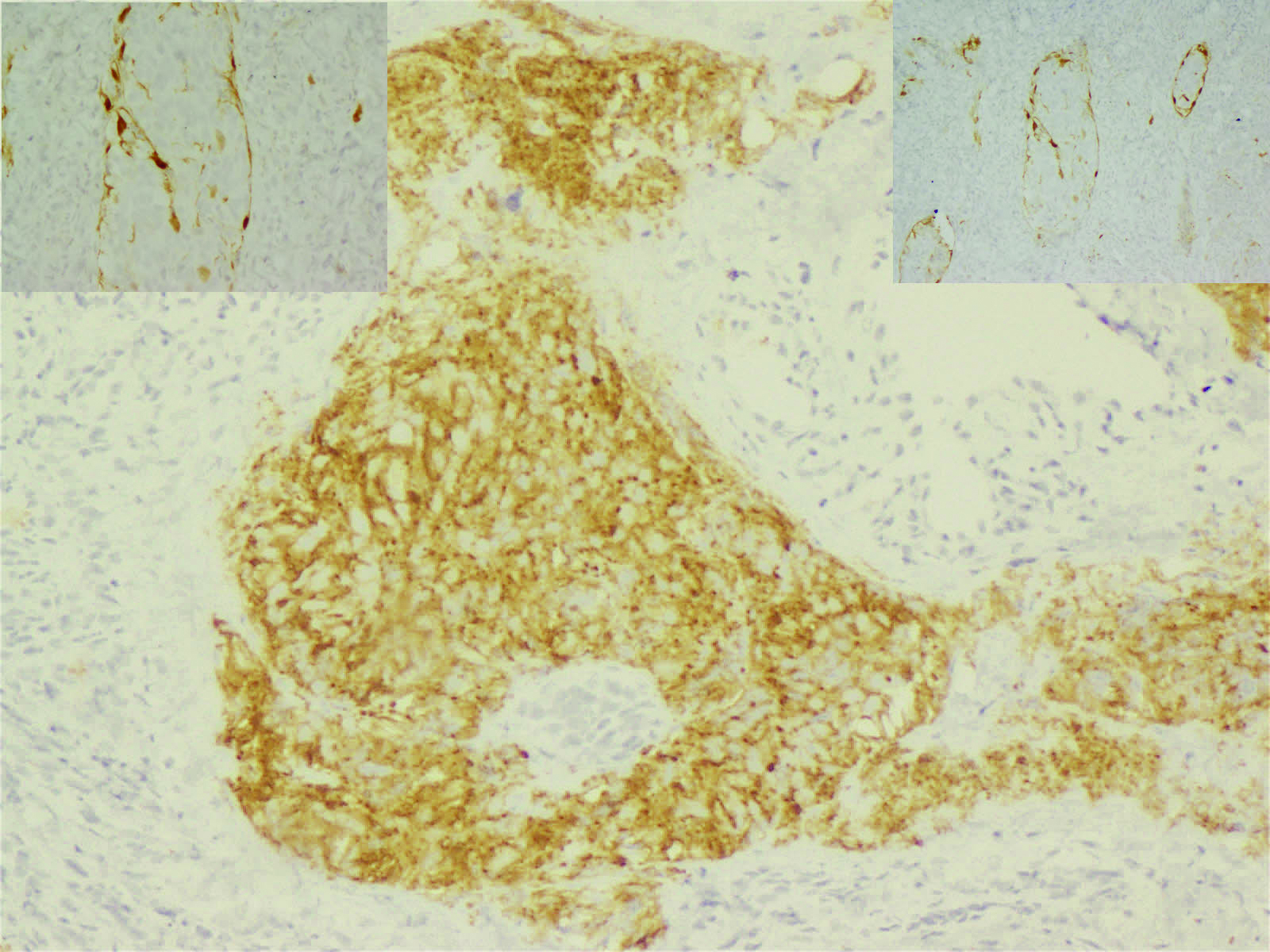
Sections showed hypercellular tumour composed of poorly retained lobular architecture with interconnecting fibrovascular stromal cells showing round to oval pleomorphic nuclei with granular chromatin [Table/Fig-6]. Focal necrosis was present with small focus of neurofibrillary material. Flexner Wintersteiner pseudorosettes and Homer Wright pseudorosettes were seen with gliosis. IHC showed synaptophysin and chromogranin positivity with S-100 positivity in the peripheral sustentacular cells [Table/Fig-7]. A final pathological diagnosis of Hyam’s Grade 3 esthesioneuroblastoma was rendered.
H&E Section shows nests and sheets of uniform cells with scant to moderate cytoplasm, round nuclei with stippled chromatin, indistinct nucleoli, mild nuclear pleomorphism, surrounded by delicate stroma with congested capillaries 100x; Left upper inset showing same section magnified - 200x.
IHC stained tumour cells showing strong cytoplasmic positivity for synaptophysin (100x) Left upper inset showing the IHC stained sustentacular cells showing cytoplasmic positivity for S-100 protein (100x) and right upper inset (200x).
Discussion
Esthesioneuroblastoma (ENB), also known as olfactory neuroblastoma, is a rare nasal malignancy that accounts for 3% of all intranasal tumours [1]. ENBs have an indolent clinical course and are poorly understood and under reported malignant neoplasm. A review of the world literature revealed up to 1000 published cases and suggested that the true incidence may be underestimated [2]. Consequently, no large series of this tumour has been accumulated and the treatment protocols have not yet been defined [3]. They have a bimodal age of onset in the second and sixth decades of life. The common manifestations include nasal congestion, rhinorrhea, epistaxis and rarely anosmia. The usual site includes the nasal cavity and ectopics, though reported, are a rare presentation [4]. These tumours involve the olfactory epithelium in the superior nasal cavity in the area of the cribriform plate, along the superior septum, and the superior turbinate [5,6]. Pathologic features include pseudorosettes, nuclear stippling and neurofibrillary stroma [7]. ENBs primarily cause invasion and destruction of surrounding structures and have a potential for metastasis.
ENB are most frequently staged using a system proposed by Kadish et al., in 1976 [3]. This classifies patients into three groups. Group A – tumour is limited to the nasal cavity, Group B – tumour is limited to the nasal cavity and paranasal sinuses and Group C – tumour extends beyond the nasal cavity and paranasal sinuses into: (i) base of skull; (ii) orbit; (iii) distant metastases; (iv) intracranial compartment. Chao et al., added and additional group in 2001, Group D – cervical nodal metastases [8]. In our case, both patients belonged to Kadish Group C. As described originally by Kadish et al., Group C FNB were considered inoperable and the standard of care dictated the patient to be subjected to high dose of radiation therapy of 6000 to 6500 rads in 7 weeks followed by surgical resection of residual disease, if operable. Group D is a very rare occurrence and as such irradiation of the neck or elective neck dissection does not appear to be indicated.
Treatment options include surgical resection followed by radiation therapy for primary lesions. Advanced, recurrent, or metastatic lesions (Group C & D) require adjuvant chemotherapy. Current recommendation supports craniofacial resection followed by radiotherapy for primary low to moderate grade lesions with addition of chemotherapy for patients with recurrent or metastatic disease [9]. The rarity in our presentation was the presence of intracranial extension of the tumour (Group C), wherein the lesion was primarily in the nasal cavity or sinuses. The other point that has been highlighted is the age variation and typical bimodal presentation of these tumours. In our series, one patient was a post partum young lady with a large intracranial extension with ICP features and the other patient was an elderly lady with a small intracranial component. This varied manifestation forms the crux of our report and highlights the need to consider ENBs as differentials in patients presenting with such symptomatology.
The present standard of care dictates an endoscopic approach for the intranasal component followed by a transcranial approach for the intracranial component. These tumours are more expansive than infiltrative and usually after gross total resection of the tumour show a small area of intranasal infiltration [10,11]. This has also made us rethink enbloc-craniofacial resection for all ENBs, thereby sacrificing healthy tissue in the process. Such staged procedures, also helps us to downgrade the Kadish staging of the tumour and thereby improving the prognosis and response to adjuvant therapy.
In our patients, we were able to achieve a complete resection, as a direct transcranial approach in one case and as a two-staged procedure in the other. Both patients were referred for adjuvant radiotherapy.
Long Term Follow-up
Case 1: The patient underwent adjuvant radiotherapy after gross total excision. She presented again, after 4 months, with recurrence of tumor, both in the intracranial and nasal cavity. We counselled them for re-surgery and tumor decompression and adjuvant radiotherapy for local control of tumor. In view of poor prognosis the patient deferred all further treatment. She was lost to follow-up and presented 2 months later with advanced disease and succumbed to raised intracranial tension (ICT) and herniation.
Case 2: The second patient has been on follow-up since the past one and a half years with no new symptoms and no radiological evidence of tumour recurrence or residual. She has been symptom free since surgery and adjuvant radiation.
Conclusion
Esthesioneuroblastomas are uncommon, under reported, intranasal malignant tumours and the presented cases reinstate the bimodal presentation of these tumours with the varied symptoms and the good results following surgical decompression in both two staged and a single trans-cranial approach in patients with smaller intranasal components.
[1]. O’Connor TA, Mclean P, Juillard GJK, Parker RG, Olfactory neuroblastomaCancer 1989 63:2426-28. [Google Scholar]
[2]. Broich G, Pagliari A, Ottaviani F, Esthesioneuroblastoma: a general review of the cases published since the discovery of the tumour in 1924Anticancer Research 1997 17(4):2683-706. [Google Scholar]
[3]. Kadish S, Goodman M, Wang CC, Olfactory neuroblastoma. A clinical analysis of 17 casesCancer 1976 37:1571-76. [Google Scholar]
[4]. Lund VJ, Howard D, Wei W, Spittle M, Olfactory neuroblastoma: past, present, and future?Laryngoscope 2003 113(3):502-07. [Google Scholar]
[5]. Diaz EM, Johnigan RH, Pero C, Olfactory neuroblastoma: the 22-year experience at one comprehensive cancer centerHead and Neck 2005 27(2):138-49. [Google Scholar]
[6]. Cho KS, Lee DG, Choi KU, Roh HJ, Primary olfactory neuroblastoma originating from the posterior nasal septumOtolaryngology 2010 142(5):776-77. [Google Scholar]
[7]. Faragalla H, Weinreb I, Olfactory neuroblastoma: a review and updateAdvances in Anatomic Pathology 2009 16(5):322-31. [Google Scholar]
[8]. Chao KS, Kaplan C, Simpson JR, Esthesioneuroblastoma: the impact of treatment modalityHead Neck 2001 23(9):749-57. [Google Scholar]
[9]. Bradley PJ, Jones NS, Robertson I, Diagnosis and management of esthesioneuroblastomaCurr Opin Otolaryngol Head Neck Surg 2003 11:112-18. [Google Scholar]
[10]. Rossi Monteiro EM, Lopes MG, Santos ER, Diniz CV, Endosocpic treatment of esthesioneuroblastomaBraz J Otorhinolaryngol 2011 77(2):171-77. [Google Scholar]
[11]. Sampath P, Park MC, Huang D, Deville C, Cortez S, Esthesioneuroblastoma with haemorrhage – An unusual presentationSkull Base – an interdisciplinary approach 2006 16(3):169-73. [Google Scholar]