Dacrycystitis or inflammation of lacrimal sac has two modes of presentation namely acute and chronic [1]. Chronic dacryocystitis is more common than the acute form and it is usually associated with obstruction of the nasolacrimal duct. The cause of Nasolacrimal Duct Obstruction (NLDO) may be idiopathic or secondary to various infections, inflammations, traumatic injuries or neoplasms. Whatever be the cause of NLDO, it ultimately leads to stagnation of tears and accumulation of mucoid secretions and desquamated cells, thereby providing a suitable environment for bacterial infections and genesis of dacryocystits [2].
Chronic dacryocystitis usually affects adults above 30 years of age and the disease has a predilection for females [3]. It is diagnosed when there is persistent epiphora or regurgitation of mucoid or mucopurulent secretions on application of pressure over lacrimal sac area or on syringing of lacrimal drainage system [2].
Routine lacrimal sac wall biopsies during Dacryocystorhinostomy (DCR) have been recommended for elucidation and better understanding of the various pathologic processes that affect lacrimal drainage system and lead to dacryocystitis. Even though the most common finding is non-specific inflammation, specific pathologies may also be encountered while evaluating these biopsy specimens. Moreover, the histomorphology even in cases of non-specific inflammatory lesions may provide clues regarding prognosis of the patients [4].
The aim of the present study was to undertake histopathological examinations of specimens obtained after DCR operation from patients of chronic dacryocystitis and to interpret various morphologic patterns, to score the degree of chronic inflammation encountered. Based on the degree of chronic inflammation, fibrosis and capillary proliferation, each specimen was assigned a chronic inflammation score, which in turn is a relevant factor of prognostic outcome of the case. The histomorphologic features vary depending on the aetiology of NLDO in a particular case. Apart from inflammatory lesions, common neoplastic lesions which may be responsible include papilloma, lymphoproliferative disorders and transitional cell carcinoma [4].
Materials and Methods
The present study was a prospective cross-sectional type of study, undertaken in the Department of Pathology of a tertiary care hospital for a period of one year, from December 2013 to November 2014. All patients who were clinically diagnosed as cases of Chronic dacryocystitis and underwent DCR during the period of study were included. Patients who were operated by Dacryocystectomy (DCT) were excluded. Patients’ consent for operative procedure and subsequent histopathological study of resected material were taken before the surgical procedure.
A total of 50 patients were included in the study. Patient details were recorded including age, gender, chief complaints and relevant medical history. A thorough pre-operative ophthalmic check-up was undertaken for all the patients to rule out any posterior segment abnormalities. The lacrimal drainage system was assessed by means of probing and syringing to confirm nasolacrimal duct obstruction.
Following DCR, the specimens of lacrimal sac, nasal mucous membrane and nasal bone were collected from each patient and sent to the histopathology laboratory in 10% neutral buffered formalin. The samples were appropriately processed for paraffin blocks and stained with Haematoxylin-Eosin (H&E) stain. In suspected cases, sections were stained with Ziehl-Neelsen (ZN) and Periodic Acid Schiff (PAS) stain for detection of acid fast bacilli (AFB) and fungi respectively. ZN stain was done in 9 (18%) and PAS stain in 4(8%) cases.
Histopathological slides were meticulously examined for the chronic inflammatory cell infiltration, fibrosis and capillary proliferation and whenever present, were graded according to severity, in each specimen. Three observers were involved in evaluation of each case. Gradation was done using the same scheme as Amin RM et al., [2]: 1) Severity of chronic inflammatory cell infiltration – mild: <50 cells per High Power Field (HPF); moderate: 50-200 cells per HPF; severe:>200 cells per HPF; 2) Severity of fibrosis was based on the amount of fibrotic tissue per HPF – mild: <25%; moderate: 25%-50%; severe:>50%; 3) Severity of capillary proliferation was based on the number of capillaries per HPF –mild: <5;moderate: 5-10; severe:>10. For all the three features, “mild” category was assigned a score of 1; “moderate”, a score of 2 and “severe”, 3 [Table/Fig-1].
Scheme for gradation of histopathologic findings of lacrimal sac specimens obtained by dacryocystorhinostomy.
| Grade | Inflammatory cell infiltrate | Fibrosis | Capillary proliferation | Chronic inflammation score |
|---|
| Mild | <50 cells/HPF | <25% per HPF | <5 capillaries/HPF | ≤3 |
| Moderate | 50-200 cells/HPF | 25%-50% per HPF | 5-10 capillaries/HPF | >3 but ≤6 |
| Severe | >200 cells/HPF | >50% per HPF | >10 capillaries/HPF | >6 |
HPF: high power field
A chronic inflammation score, ranging between 3 and 9, was recorded for each case, after adding the individual scores for each of these histopathologic features. This final score was used to categorize each case as mild (score ≤3), moderate (score >3 but ≤6) and severe (>6) chronic inflammation [2]. Any other relevant histopathologic findings, if noted, were also recorded. Even though inter-observer variability with regard to individual parameters of the chronic inflammation score was found in 7 (14%) cases, there was no discrepancy in the final scores assigned to each case by the observers.
Results
Present study included 50 patients over a period of one year. The average age of the patients was 39.04 years, having a standard deviation (SD) of ±14.22 and their age ranged between 13 and 62 years. The number of female patients exceeded that of the males, with 28 (56%) females and 22 (44%) males.
The nasal bone did not reveal any abnormality in any case. Viable bony tissue without any inflammation was found in all patients.
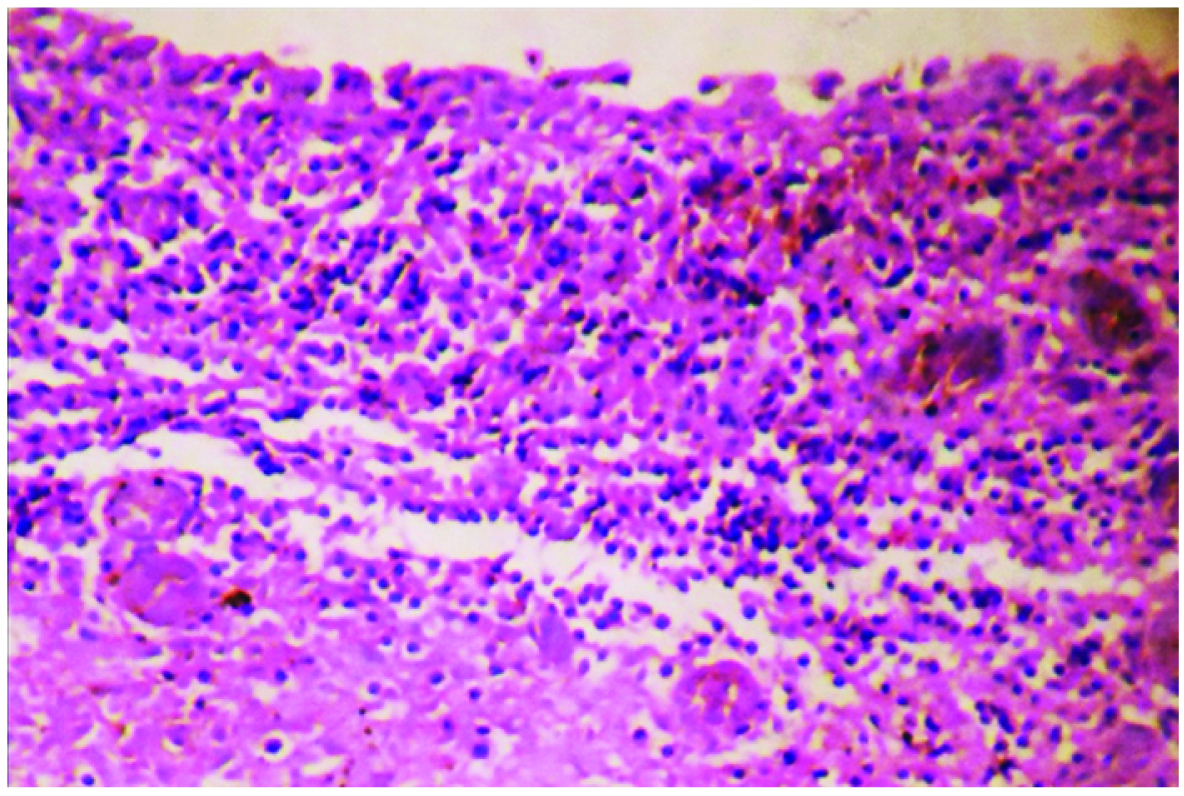
The lacrimal sac and nasal mucous membrane, on the other hand, did not reveal normal histologic features in any patient. The nasal mucous membrane showed mild degree of chronic inflammatory cell infiltration in 46 (92%) cases. Linear band of chronic inflammatory infiltrate was noted below nasal mucous membrane in some of those cases [Table/Fig-2]. In the other 4 (8%) patients, moderate degree of infiltration by chronic inflammatory cells was noted. Denudation of nasal mucous membrane was seen in one of them [Table/Fig-3].
Mild chronic inflammatory cell infiltration in the form of linear band beneath nasal mucous membrane (H&E ×100).
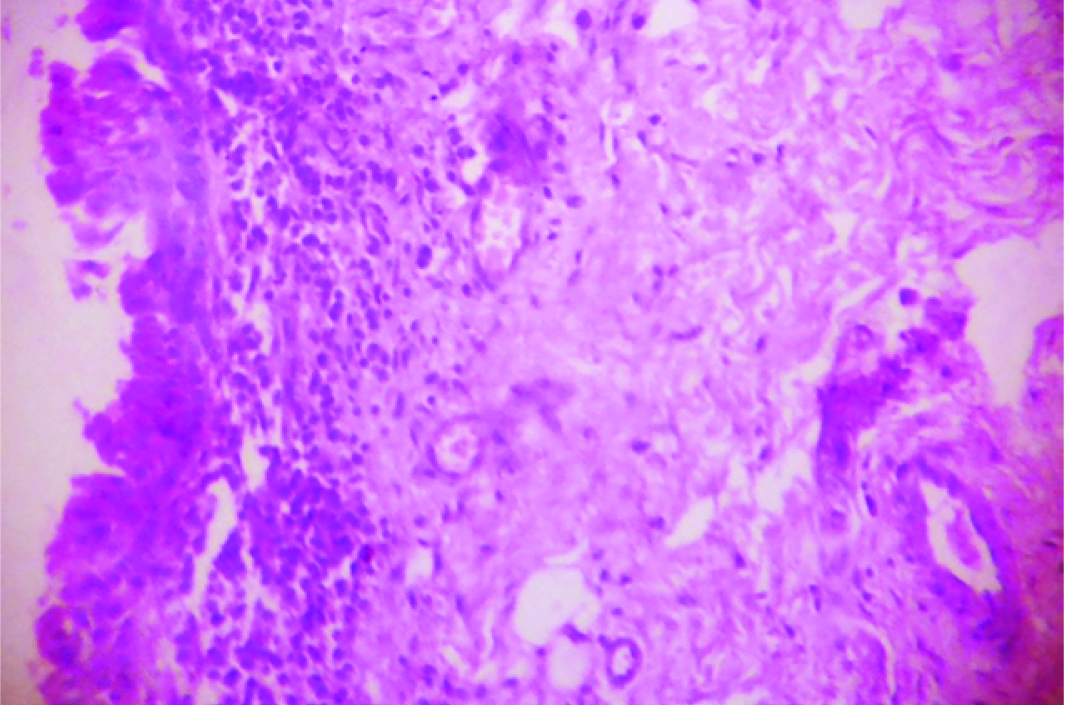
Moderate degree of chronic inflammatory cell infiltration with denudation of the overlying nasal mucous membrane (H&E ×100).
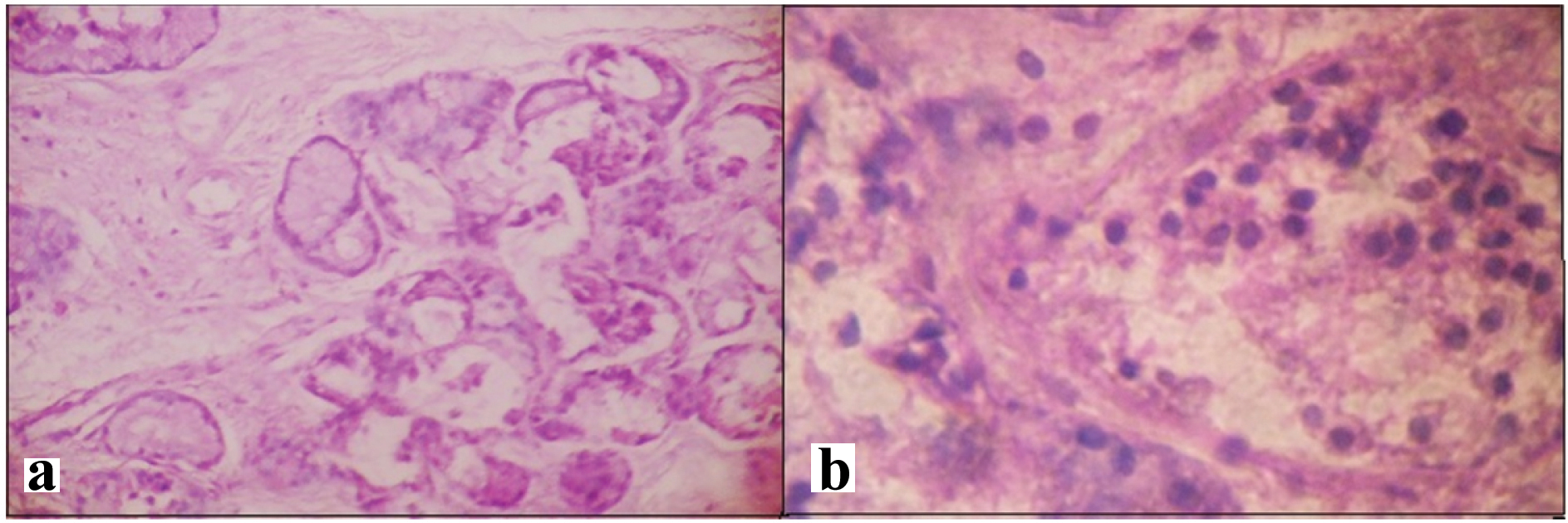
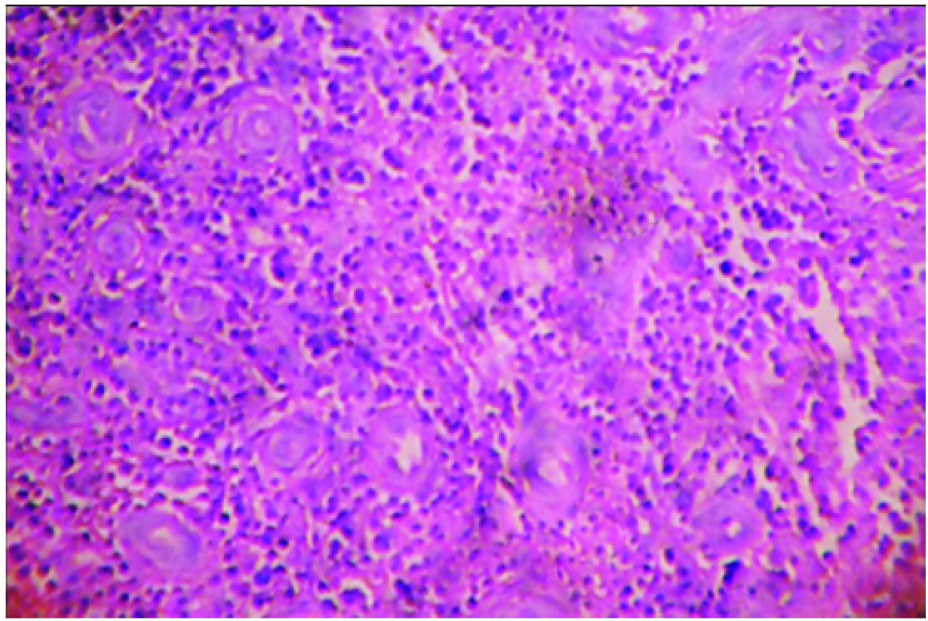
Chronic inflammation with granulation tissue formation was noted in the lacrimal sacs of all patients. Chronic inflammatory cell infiltration was found to be mild in 14 (28%) cases and severe in 12 (24%) cases [Table/Fig-4a,b]. No lacrimal sac specimen showed severe fibrosis, however, severe grade of capillary proliferation was found in 10 (20%) cases. Diffuse, chronic inflammation with marked vascular proliferation was noted in some of those cases [Table/Fig-5]. The chronic inflammation score was calculated in each case and it revealed that 14 (28%) cases belonged to the “mild” group, 26 (52%) to the “moderate” group and 10 (20%) to the “severe” category [Table/Fig-6].
(a) Lacrimal sac; mucous glands with mild chronic inflammatory cell infiltration in stroma (H&E ×100); (b) Mild degree of lymphocytic infiltration in lacrimal sac (H&E ×400).
Lacrimal sac; diffuse severe chronic inflammation with vascular proliferation (H&E ×100).
Histopathologic findings of lacrimal sac specimens obtained by dacryocystorhinostomy.
| Grade | Inflammatory cell infiltrate (n=50) | Fibrosis(n=50) | Capillary proliferation (n=50) | Chronic inflammation score (n=50) |
|---|
| Mild | 14 (28%) | 36 (72%) | 32 (64%) | 14 (28%) |
| Moderate | 24 (48%) | 14 (28%) | 8 (16%) | 26 (52%) |
| Severe | 12 (24%) | 0 | 10 (20%) | 10 (20%) |
Discussion
Diseases of lacrimal drainage system are so common that they account for nearly 3% of all visits to eye clinic [2]. Chronic dacryocystitis is a frequently encountered disorder among these patients. The usual symptoms include excessive watering of the eyes and pain towards the side of the nose [5].
NLDO is most commonly associated with non-specific chronic inflammation. Specific pathologies, both inflammatory and neoplastic, have been reported in 0 to 14·3% cases in previous studies. The most frequently reported specific pathologies include sarcoidosis, lymphoma and papilloma [6].
The common causative organisms of Chronic Dacryocystitis include Staphylococcus aureus, Streptococcus species and other Gram negative bacteria like Pseudomonas, Citrobacter and Enterobacter species [3,7]. Comez AT et al., reported a rare case of chronic dacryocystits caused by Stenotrophomonas maltophilia and methicillin-sensitive Staphylococcus aureus [8].
Treatment of choice for chronic dacryocystitis is Dacryocystorhinostomy (DCR). Dacryocystectomy (DCT) is reserved for those patients in whom DCR is contraindicated [2]. There is difference in opinion among authors regarding the requirement of routine histopathological examination of specimens obtained after DCR. Merkonidis C et al., concluded in their study that routine lacrimal sac biopsies after DCR are unnecessary. They opined that such biopsies must only be undertaken if any specific pathology is suspected based either on clinical features or gross appearance of lacrimal sac [6].
On the other hand, Anderson et al., believed that lacrimal sac biopsies must be undertaken routinely after DCR [4]. This is due to the fact that ominous diseases may be present in innocuous looking lacrimal sacs [9]. Since neoplastic diseases that affect lacrimal sac are mostly malignant in nature, routine biopsies are indispensable, as they ensure early detection in otherwise asymptomatic cases [2]. Common malignancies of lacrimal sac are epidermoid carcinoma, transitional carcinomas, mucoepidermoid tumours, adenocarcinomas and adenoid cystic carcinomas [10]. Various lesions detected in apparently normal lacrimal sacs include sarcoidosis, papilloma, granular cell tumour, oncocytoma, adenocarcinoma, transitional cell carcinoma, adenocarcinoma, lymphoma and plasmacytoma [4].
Knežević M et al., highlighted that even though most lacrimal sac biopsies reveal non specific chronic inflammation, routine biopsies must always be undertaken to rule out any specific pathologies and also for better understanding of various diseases of lacrimal system [11].
Even though no specific pathology of lacrimal sac was detected in the present study, the authors agree that routine histopathological examinations are required after DCR. This is because studies suggest that non-specific findings like chronic inflammation is a prognostic parameter and chronic inflammation score may be used to predict outcomes after DCR. The difference of chronic inflammation scores between patients with successful and unsuccessful results after DCR was found to be statistically significant [12].
In most of the studies females have been found to outnumber males which corroborates the fact that chronic dacryocystitis has a predilection for female patients. Bhuyan J et al., diagnosed chronic dacryocystitis in 77% females and 23% male patients [13]. Corresponding figures of the present study were 56% in females and 44% in males. Amin RM et al., calculated chronic inflammation scores in all cases of Chronic Dacryocystitis and they found moderate score in 82%, severe in 12% and mild in 6% cases [2]. Chronic inflammation scores were obtained in all cases included in the present study and mild score was found in 28%, moderate in 52% and severe in 20%.
Conclusion
Authors of this study recommend that chronic inflammation score must be included in the histological evaluation of specimens obtained by DCR. Since greater degree of inflammation is associated with a poor outcome, this score would help clinicians to monitor the dose and duration of therapy with anti-inflammatory drugs, thereby modifying the course of the disease. Therefore protocol of histomorphological evaluation and scoring system of chronic inflammation as described in the present study will be of immense aid to clinician for appropriate management of such cases.
HPF: high power field