Female urethral injuries are rare occurrence. Obstetric injuries to urethra are predominantly due to prolonged labour, particularly if maternal fetal disproportion exists, causing urethral pressure necrosis [1]. Urethral injuries can occur in cases of gynaecological surgeries like vaginoplasty or in cases of urethral diverticulae [2]. Obstetric injuries are one of the important causes of urethral loss in developing countries. Urethral injury has been described in association with pelvic fracture in as many as 6% of cases [3]. Female urethral injury can be associated with fracture pelvis but that can be proximal or distal; however total urethral loss is rare [4].
Multiple techniques of urethral reconstruction are developed with goals of reconstruction of urethra and restoration of continence. Neourethra should permit normal urinary passage with continence and should be of sufficient length to ensure that the patient does not void into the vagina. Urethral replacement can be accomplished by anterior bladder wall (Tanagho) tube or tubularization of vaginal wall flap (Blaivas) [5,6]. Advantage of bladder wall tube is vaginal wall flap cannot be done in patients with small atrophic vagina secondary to initial insult or when virginity is concerned. The disadvantage of bladder wall tube is it requires extensive reconstruction. We describe our experience of vaginal flap urethroplasty in females with complex urethral injury with total incontinence treated at our tertiary care institute. There is no such study from India till now.
Materials and Methods
Retrospective analysis of patients was done from August 2008 to July 2015 in tertiary care centre. All the patients with complete urethral loss irrespective of etiology of urethral loss were included in this study. All patients presented with overt urinary incontinence. The diagnosis was confirmed by clinical examination of the vagina. Urinary drainage was done with Suprapubic catheterization (SPC) till definitive management was deferred. After 8-12 weeks of initial insult, upper urinary tract evaluation was performed in all patients by either Computed Tomography urography (CT) scan or intravenous urography. Pre-operative panendoscopy and pelvic examination were done to evaluate extent of the anatomic defect, possibility of unrecognized secondary fistulae, pliability of local vaginal tissue and then reconstructive urethral surgery was planned. Patients were subsequently operated by single surgeon with neourethral tube formation from anterior vaginal flap.
Technique
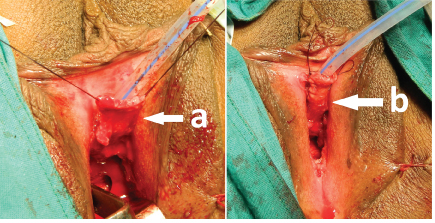
Patient was placed in the dorsal lithotomy position, and panendoscopy was performed which was suggestive of wide open bladder neck with total loss of urethra as shown in [Table/Fig-1], A 14-perurethral Foley catheter was inserted into the urinary bladder, and the balloon was inflated with normal saline to hold it securely at the bladder neck.
Wide open bladder neck with bladder mucosa
(a) Absent of urethra with bladder mucosa prolapsing through the opening
(b) Adequate vagina with healthy mucosa
(c) Vaginal flap marking.

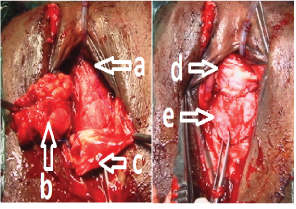
The neourethral tube was created by taking two parallel anterior vaginal wall incisions around existing urethral meatus around 4-5 cm in length and 1.8 to 2 cm width as shown in [Table/Fig-1]. Vaginal flap was dissected and flipped up. Flap was tabularized over 14 Frfoley’s catheter with absorbable 4-0 polyglactin sutures as shown in [Table/Fig-2]. Neourethra was covered with Martius labial flap and autologous fascia as shown in [Table/Fig-3].
(a) Raised vaginal flap; (b)Tubularized vaginal flap.
(a) Completed vaginal flap layer (b) Raised Martius labial flap (c) Fascia lata sling (d) Completed second layer of Martius flap (e) Third layer of fascia lata.
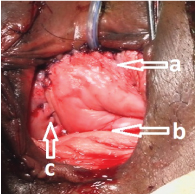
In all patients sling was placed to give support to neourethra and aid urinary continence. Pubovaginal sling technique involves harvesting a strip of autologous fascia (Fascia lata or rectus abdominis fascia), which was fashioned as 2cm X 10 to 15cm strip as shown in [Table/Fig-3]. Autologous fascia was placed over Martius fat pad and the sling was anchored to anterior abdominal wall. Vaginal incision was closed with 3-0 polyglactin [Table/Fig-4]. Vaginal pack was kept for 24 hours. Intravenous antibiotics were given for seven to ten days. Perurethral catheter was removed after three weeks. Suprapubic catheter was removed after successful voiding trial. Patients were followed up with urine flow study, post-void residue and urinary continence.
Completed Neourethra reconstruction (a) Neourethra (b) Vagina (c) Sutured Martius flap incision.
Results
[Table/Fig-5] Shows details of all patients with postoperative follow-up. Out of seven patients which were included in present study, four patients were after obstructed labour, two after post vaginal hysterectomy with anterior colporrhaphy, one patient following pelvic trauma. All patients were operated by transvaginal route and neourethral tube was created with the help of anterior vaginal wall, 4-5 cm in length. Second layer of Martius labial fat pad was covered in all patients. Autologous pubovaginal fascia lata sling was used in five patients and rectus abdominis fascia sling was used in rest two patients.
Details of all patients with postoperative follow up.
| Case | Age(years) | Aetiology | Operativetime (minutes) | blood loss (ml) | Mean duration ofhospitalisation | PostoperativeQmax (Maximumurine flow rate) | PostoperativePost void residue | PostoperativeContinence |
|---|
| 1 | 65 | Vaginal hysterectomy with colporrhaphy | 200 | 230 | 8 | 15.4 | 10 | Mild SUI |
| 2 | 30 | Obstructed labour | 160 | 230 | 7 | 16.2 | 22 | Continent |
| 3 | 28 | Obstructed labour | 180 | 250 | 9 | 16.9 | 21 | Continent |
| 4 | 32 | Traumatic injury | 190 | 260 | 7 | 6.7 | 50 | Stenosis |
| 5 | 58 | Vaginal hysterectomy with colporrhaphy | 190 | 180 | 8 | 17.3 | 10 | Continent |
| 6 | 25 | Obstructed labour | 180 | 220 | 8 | 15.2 | 30 | Continent |
| 7 | 32 | Obstructed labour | 160 | 170 | 9 | 18.2 | 15 | Continent |
SUI – Stress urinary incontinence.
Mean operative time was 180 minutes (160–200 minutes) and mean intraoperative blood loss was 220ml (170-260ml). Mean duration of hospitalization was 8 days (7-9 days). On follow-up patients were assessed for continence, urine flow rate, renal biochemical parameters and ultrasound for upper urinary tract and post void residue every 3 monthly. On follow-up one patient had mild stress urinary incontinence however another patient developed urethral stenosis and managed with urethral dilatation. All patient’s serum creatinine and upper tract were maintained, mean urine flow rate was 15.1ml/sec (6.7 -18.2 ml/sec) and mean postoperative post void residue was 22.5cc (10-50 cc). Median follow-up time was 35 months.
Discussion
The management of female urethral loss can be challenging. In our study, most common cause of urethral loss was obstructed labour (57.1%). Damage to urethra during delivery is thought to be due to prolonged labour, most often associated with maternal- fetal disproportion. Long standing labour with prolonged pressure of fetal head on vesico-urethral junction leads to ischemia and urethral injury [7]. Vaginal hysterectomy with anterior coporraphy can cause urethral injury while dissection of anterior vaginal wall presenting as total incontinence. Rarely, trauma to the pelvis bone may result in fracture or pubic symphysis diastasis, which causes urinary bladder neck transaction or urethral injury. Traumatic fracture of the pelvis may result in urethral contusion, partial or complete transection of the female urethra. Postulated mechanisms of urethral injury are diametric fracture, diastasis of pubic symphysis with rupture of posterior pubourethral ligament, direct injury by a bony spicule [8]. In our case it was pubic symphysis diastasis and direct injury of bony tissue causing total urethral loss.
Urethral injury should be suspected when patient presents with urinary incontinence after difficult vaginal delivery, pelvic surgery or pelvic fracture. In all of such injuries, one must have a high index of suspicion that concomitant injuries such as vesicovaginal or ureterovaginal fistula might be present, and complete preoperative evaluation to exclude these conditions should be done. The main indications for reconstruction are urethral obstruction or sphincteric incontinence [9]. In our study all patients were operated by anterior vaginal wall tube reconstruction. We did delayed management of urethral loss, after allowing time for local tissue to heal.
There are various management options available for female urethral trauma like primary closure, vaginal flap urethroplasty, vaginal wall urethroplasty and bladder wall urethroplasty [10]. Primary closure is suitable only for small defects. For larger defects other options should be chosen. Success rate of vaginal flap urethroplasty was around 91% which was comparable to present study results of 86% [10]. Vaginal flap urethroplasty can be done for stricture urethra. In a study of vaginal wall urethroplasty two patients out of five patients required dilatation, as compared to one out of seven patients in present study [11]. In this same study median postoperative maximum flow rate and post void residue were 10.5 ml/sec and 25cc. In present study mean maximum flow rate and post void residue were 15.1 ml/sec and 22.5cc. Reported complications of urethral construction were obstruction, fistula and incontinence. Complications could be reduced with adequate width of flap and layered closure of urethra.
Tanagho described a technique of urethral construction using anterior bladder wall, disadvantage of this operation is extensive reconstruction required. Blaivas JG studied vaginal flap reconstruction on ten patients with continence rate of 60% after single reconstruction [5,6]. Out of four incontinent patients, two patients were further cured by pubovaginal sling. He concluded that single stage vaginal flap reconstruction and pubovaginal sling procedure is effective and offers viable, simple alternative to bladder flap urethral reconstruction. Bladder wall flaps are preferred over vaginal wall flap when patient’s vagina is scarred or patient’s virginity is concerned.
Radwan studied 15 patients of urethral loss, out of which six patients were operated by anterior bladder tube (Tanagho) and rest of patients by labia minor apedicled tube with Transobturator Tape (TOT) sling. Total continence was achieved in 66.6% of patients in both the groups. He concluded that both procedures have high success rate and equally effective in females with total urethral loss [12]. Flisser AJ had also studied patients with urethral loss and majority of patients were treated by vaginal flap repair. He also reproduced continence in 87% patients and successful anatomical repair was achieved in 93 % of patients [13]. These statistics were comparable with our study in which only 14% patient was having mild urinary incontinence and rest 86% patients were continent. In our study all patients achieved anatomical repair with no postoperative fistula and redo-surgery.
Limitation
Major limitation of present study is limited number of cases, as total urethral loss is very rare phenomenon hence long term study should be done before concluding superiority of vaginal flap over other techniques.
Conclusion
Total urethral loss is a very rare phenomenon. Treatment option should be decided after local examination and extent of injury. Urethral reconstruction with vaginal flap and autologous pubovaginal sling is feasible option in such cases if vaginal mucosa is adequate and healthy. Success rate in present study is approximately 86%. This procedure is a simple alternative to bladder wall tube and should be considered in cases of female urethral loss.
SUI – Stress urinary incontinence.