Actinomycotic Osteomyelitis of the Maxilla – A Delusive Presentation
Anjana Chathoth Meethal1, Manjusha Pattamparambath2, Anita Balan3, Nileena R Kumar4, Sudha Sathyabhama5
1 Junior Resident, Department of Oral Medicine and Radiology, Government Dental College, Calicut, Kerela, India.
2 Senior Resident, Deparment of Oral Pathology and Microbiology, Government Dental College, Calicut, Kerela, India.
3 Professor and Head, Department of Oral Medicine and Radiology, Government Dental College, Calicut, Kerela, India.
4 Associate Professor, Department of Oral Medicine and Radiology, Government Dental College, Calicut, Kerela, India.
5 Professor and Head, Department of Oral Pathology and Microbiology, Government Dental College, Calicut, Kerela, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Manjusha Pattamparambath, Senior Resident, Deparment of Oral Pathology and Microbiology, Government Dental College, Calicut, Kerela-673005, India.
E-mail: manjumdvn@gmail.com
Actinomycosis, Cervicofacial, Oroantral fistula
A 79-year-old female patient reported to the Department of Oral Medicine and Radiology, with a complaint of a progressively enlarging painless ulcer of the palate of six months duration. The ulcer caused difficulty in speech and swallowing due to nasal regurgitation. Her medical history revealed that she was a chronic diabetic patient with poor glycemic control. She was on insulin one year back and now on oral hypoglycemics. She gave a history of carcinoma breast and extensive esophageal candidiasis one year back for which she had undergone treatment. She also complained of severe headache, tiredness, nasal discharge and numbness over the right side of her face and appeared cachectic. Examination of the patient’s face revealed no gross asymmetry. Intraorally, the ulcer measured approximately about 6x6cm involving most of the anterior part of hard palate with irregular and undermined edges [Table/Fig-1]. There was exposed necrotic grey colored bone on the base of the ulcer and discrete areas of black eschar. Slough was seen more towards the periphery of the lesion. Oro-nasal communication of size approximately 1.5x1.5cm was present on the anterior part of the lesion towards right side and a smaller one towards left side. On palpation the lesion was tender. Upper deep cervical lymph nodes were palpable bilaterally. Multiple missing teeth, root stumps and caries exposed teeth were present in the maxillary and mandibular arches. Results of complete blood count and serum electrolyte analysis were within normal limits.
Ulcer with irregular and undermined edges. Oro-nasal communication seen.

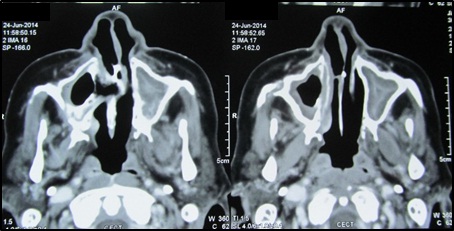
Radiographic examination was performed to assess the nature and extent of the lesion. A maxillary occlusal radiograph revealed an irregular radiolucency in the anterior palate with destruction of the alveolar process in relation to the upper anterior region [Table/Fig-2]. A panoramic radiograph revealed ill-defined radiolucency involving the palate on right side crossing the midline up to the premolar region on left side extending superiorly to involve the maxillary sinus with sinus floor destruction bilaterally [Table/Fig-3]. Water’s view was also taken which showed haziness in the right maxillary sinus [Table/Fig-4]. Plain and contrast enhanced CT report revealed soft tissue density lesions involving the palate, both maxillary sinuses, left posterior ethmoid sinus and margin of the sphenoid sinus and was associated with erosion of the adjacent part of sphenoid bones on both sides. A large bone defect was seen in the floor of right maxilla which indicated oro-antral fistula. Smaller bone defects were also visible in the anterior part of the floor of both nasal cavities with evidence of oro-nasal fistulae. Enlarged level II lymphnodes were also noted on both sides. All these findings suggested the lesion to be an extensive fungal granuloma or a neoplasm [Table/Fig-5,6].
Maxillary occlusal radiograph showing irregular radiolucency in the anterior palate with destruction of alveolar process.

Panoramic radiograph showing ill-defined radiolucency involving the palate.

Water’s view showing haziness in the right maxillary sinus.

Coronal CT section showing oro-antral communication.
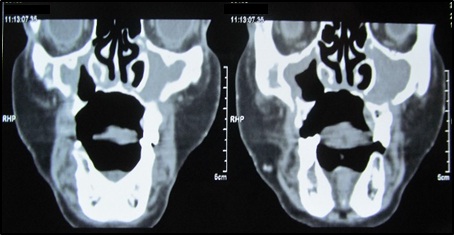
Axial CT section showing oro- antral communication.
Our clinical differential diagnosis included deep fungal ulcer, primary syphilitic gumma, metastatic carcinoma of the maxilla, idiopathic midline granuloma and osteomyelitis of the maxilla. Insulin-dependent uncontrolled diabetics like the current patient, are more prone to develop deep fungal ulcers. In such cases, the oral and nasal cavities may reveal a black eschar on the palate, septum or turbinate. Oral manifestations of tertiary syphilis are characterized by a gumma formation on hard palate, tongue or lower alveolus resulting in bone destruction, palatal perforation and oro-nasal fistula. However, Venereal Disease Research Laboratory (VDRL) test was done for the patient, which was negative. Metastatic tumor to the maxilla was considered since the patient reported a prior history of carcinoma breast. Owing to the presence of multiple root stumps and carious teeth osteomyelitis of the jaws was also considered in the differential diagnosis. Idiopathic Lethal Midline Granuloma (LMG) is an idiopathic lethal tumor of granulation tissue arising in the nose and palate [1]. There was chronic destructive process of the palate in our case, similar to that seen in LMG.
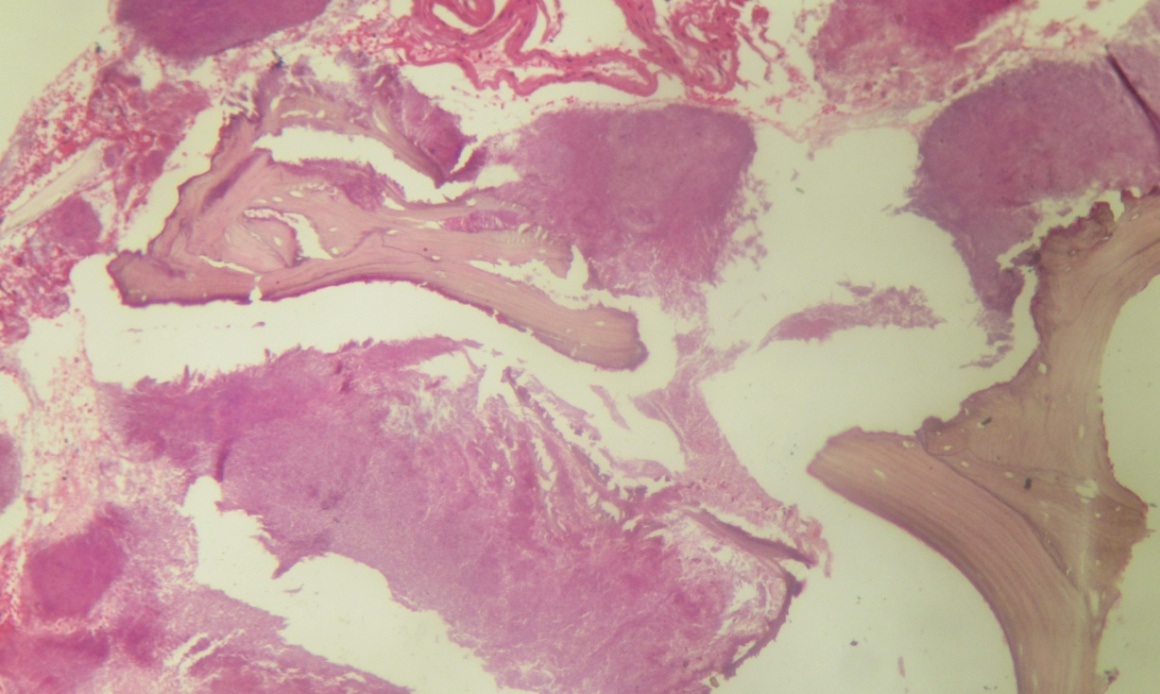
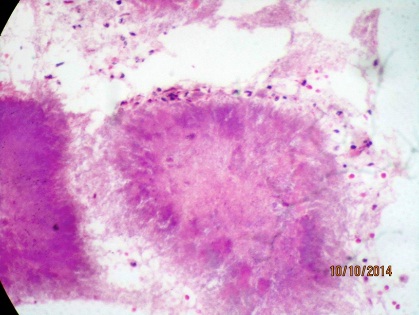
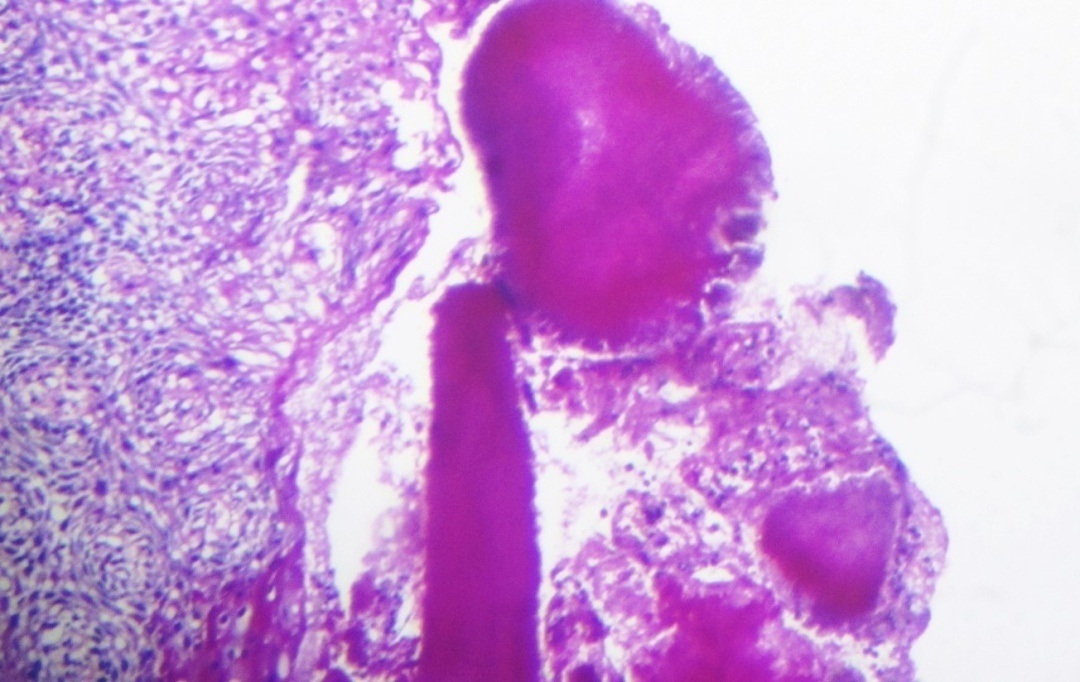
An incisional biopsy was done under local anesthesia. Hard and soft tissue specimens were sent for histopathologic examination, which revealed the presence of necrotic bone enclosing colonies of actinomycotic organism [Table/Fig-7]. The colonies consisted of characteristic club shaped filaments that formed radiating rosette pattern with peripheral basophilic filaments and eosinophilic club shaped ends [Table/Fig-8]. To confirm the histopathologic diagnosis sections were stained with Periodic Acid Schiff (PAS) [Table/Fig-9] and Gomori Methanamine Silver stains (GMS) [Table/Fig-10]. Thus a final diagnosis of actinomycotic osteomyelitis was reached.
H& E stained section at 100X magnification showing necrotic bone enclosing colonies of actinomycotic organism.
H& E stained section at 400X magnification showing characteristic actinomycotic colony.
PAS stained section at 100X magnification showing actinomycotic colonies.
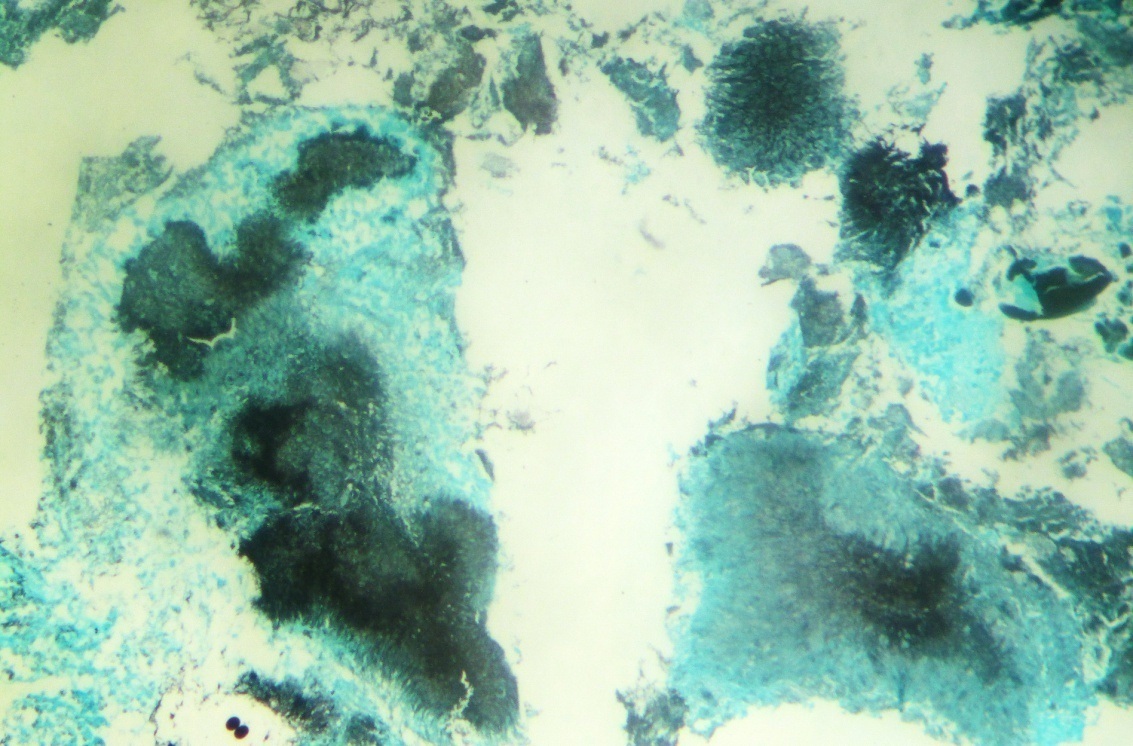
GMS stained section at 100X magnification showing black coloured colonies of actinomyces.
The patient was hospitalized and surgical debridement was done for the removal of necrotic, fibrous and edematous tissue. Surgical correction of the defect was avoided owing to the debilitated condition of the patient. Diagnostic Nasal Endoscopy (DNE) was done under local anesthesia which confirmed oro-nasal fistula and oro-antral fistula. The maxillary sinus was found normal in the DNE. Post operatively she was treated with antibiotics and analgesics- Injection Crystalline Penicillin (CP) 20 lac U 6th hourly for four weeks and oral penicillin/amoxicillin 500mg 6th hourly to be continued for 18 months. An obturator was then constructed for the patient. The patient was discharged and is now under regular follow-up [Table/Fig-11,12].
Palatal defect after surgical debridement.

Obturator placed over the palatal defect.

Discussion
Actinomycosis is an infection caused by anaerobic non acid fast Gram-positive Actinomyces species, which belong to the natural flora of the oral cavity, gastrointestinal tract and urogenital tract [2]. Actinomyces israelii is the principal cause of human actinomycosis. Based on the site affected actinomycosis is clinically classified into cervicofacial, pulmonothoracic and abdominocervical forms, of which the commonest form is cervicofacial one. Cervicofacial actinomycotic lesions usually presents as a single or multiple abscess or indurated lumps with fistulation and a discharge of sulfur granules [3]. Although the oral mucosa is often the site of entry of actinomyces into the deeper tissues, actinomycosis in the oral mucosa is extremely rare with fewer than 50 cases reported [4]. This may be due to the good blood supply of the face which provides better circulation and more oxygen supply.
Osteomyelitis due to actinomycosis has been reported infrequently in adults with bone involvement seen only 1 in 15 percent of those reviewed by Lewis and associates [5]. The exact pathophysiology of actinomycotic osteomyelitis is unclear; however it is suggested that inflammation begins when the normal composition of the microbial flora is disturbed as in trauma, periodontal infection or extractions. In our case the patient’s poor oral hygiene and multiple carious teeth hints that penetration site of this organism, into deeper tissue, was probably from a chronic periapical infection. The debilitated nature of the patient also contributed to the extensive progression of the lesion. Our case gains importance because of the rarity of the lesion, location in the palate, its extensiveness and the dilemma it causes in the diagnosis due to the varied clinical presentation.
Diagnosis of actinomycotic osteomyelitis is often based on clinical, radiological and microscopic evidence, rather than bacteriological culture and identification. This is due to numerous problems associated with culture like inability to maintain anaerobic conditions and overgrowth of other bacteria. Treatment often requires high-dose, long-term antibiotic therapy.
Actinomycosis has been referred to as the chameleon of head and neck pathology because of its varied clinical picture which can resemble pathologies ranging from benign infection to metastatic tumor [6]. Actinomycotic osteomyelitis affecting maxilla is a rare condition with features differing from that of cervicofacial actinomycosis. In this scenario it is crucial for a dentist to have an adequate knowledge of the various clinical presentations so that actinomycotic infection can be considered in the differential diagnosis of bone lesions affecting the jaws even in the absence of characteristic clinical presentations.
[1]. Batra P, Shah N, Mathur S, Midline lethal granuloma-a clinical enigmaIndian J Dent Res 2003 14(3):174-83. [Google Scholar]
[2]. Sarkonen N, Kononen E, Summanen P, Kanervo A, Takala A, Jousimies-Somer H, Oral colonization with actinomyces species in infants by two years of AgeJ Dent Res 2000 79(3):864-67. [Google Scholar]
[3]. Bennhoff DF, Actinomycosis: diagnostic and therapeutic considerations and a review of 32 casesThe Laryngoscope 1984 94(9):1198-217. [Google Scholar]
[4]. Goldstein B, Sciubba J, Laskin D, Actinomycosis of the maxilla: review of literature and report of caseJ Oral Surg 1972 30(5):362-66. [Google Scholar]
[5]. Lewis M, MacFarlane T, McGowan D, A microbiological and clinical review of the acute dentoalveolar abscessBr J Oral Maxillofac Surg 1990 28(6):359-66. [Google Scholar]
[6]. Norman J, Cervicofacial actinomycosisOral Surg Oral Med Oral Pathol 1970 29(5):735-45. [Google Scholar]