Splenic Epidermoid Cyst in a Five-Year-Old Child
Sumit Grover1, Bhavna Garg2, Neena Sood3, Satpal Singh4
1 Assistant Professor, Department of Pathology, Dayanand Medical College & Hospital, Ludhiana, Punjab, India.
2 Professor, Department of Pathology, Dayanand Medical College & Hospital, Ludhiana, Punjab, India.
3 Professor and Head, Department of Pathology, Dayanand Medical College & Hospital, Ludhiana, Punjab, India.
4 Professor, Department of G.E. Surgery, Dayanand Medical College & Hospital, Ludhiana, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sumit Grover, Assistant Professor, Department of Pathology, Dayanand Medical College & Hospital, Tagore Nagar, Ludhiana, Punjab-141001, India.
E-mail: sumitgrover1204@gmail.com
Splenic epidermoid cysts are rare non-parasitic true cysts affecting the spleen. We report a five-year-old child who presented with an abdominal lump associated with pain of 15 days. Ultrasonography of the abdomen showed a huge cystic lesion of obscure origin. At laprotomy a huge unilocular cyst involving upper part of spleen containing pultaceous fluid was seen and its removal necessitated splenectomy. Histopathological findings were consistent with splenic epidermoid cyst. Thus histopathology helped in elucidating the aetiology and diagnosis.
Histopathology, Spleen, Splenectomy, Squamous lining, True cyst, Unilocular
Case Report
A five-year-old male child presented to the paediatric emergency room with a dull dragging epigastric and right hypochondriac pain since 15 days. The parents denied any history of abdominal injuries, dyspepsia and constipation in the past. On examination he was found to have tenderness and a diffuse palpable lump in left hypochondriac and lumbar region without any definite margins.
Base line laboratory investigations including haemoglobin, complete blood count were normal. Serological tests for HBsAg and HIV were nonreactive. Indirect haemagglutination test and enzyme-linked immunosorbent assay for detection of anti-Echinococcus antibodies were negative.
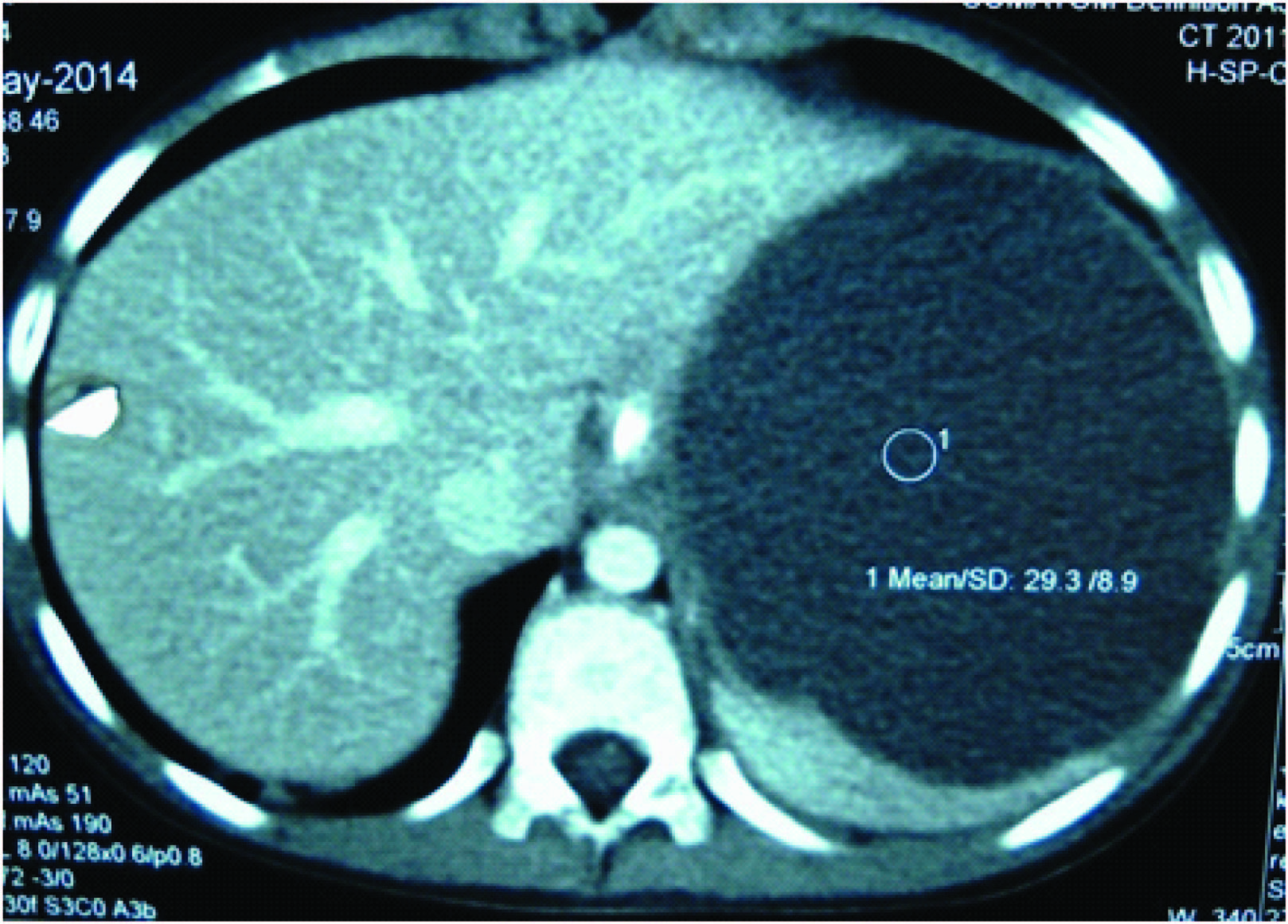
On contrast enhanced MDCT scan of whole abdomen a large exophytically bulging well defined cystic lesion is seen measuring 12x10x10cm and replacing upper and mid part of spleen, extending superiorly up to left dome of diaphragm, medially indenting posterior and lateral wall of stomach and indenting the tail of pancreas [Table/Fig-1]. A clinical and radiological impression of pseudocyst was made.
Axial contrast enhanced computed tomography image revealing a well defined clear cystic lesion in the inferior recess of lesser sac arising from spleen.
At laparotomy a huge unilocular cyst involving upper part of spleen containing purulent fluid was found. The large size of cyst and little splenic parenchyma made preservation of spleen impossible.
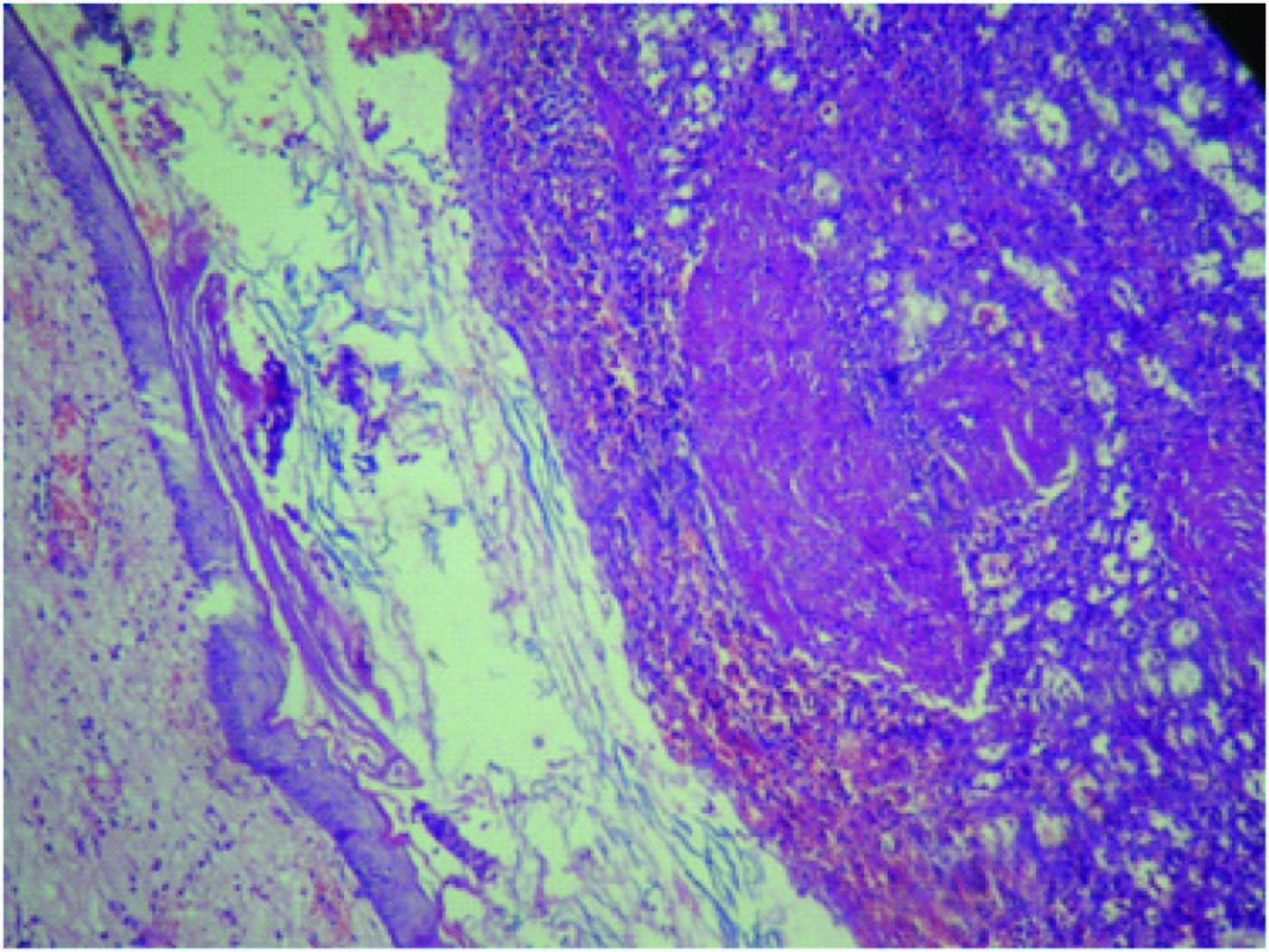
A splenectomy specimen weighing 600 grams with a large cut open cyst measuring 10x8cm was received in laboratory for histopathological examination. Grossly inner cyst wall was greyish white glistening with marked trabeculations and slightly congested adjacent splenic parenchyma of size 4x2cm [Table/Fig-2]. Microscopic examination revealed a true cyst with thick fibrous wall and a lining of keratinized stratified squamous epithelium [Table/Fig-3]. The adjacent spleen showed sinusoidal congestion. Final diagnosis of an infected epidermoid cyst spleen was made.
Greyish white glistening cyst wall with marked trabeculations.

Fibrous cyst wall lined by stratified squamous epithelium with in splenic parenchyma (H&E, X 100).
The postoperative course was uneventful and the child was discharged after 5 days of operation.
Discussion
Cystic lesions are among the unusual lesions of spleen which include parasitic and non-parasitic cysts. The non-parasitic cysts are still rarer and divided into true cysts having an epithelial lining (epidermoid, dermoid and mesothelial) or endothelial lining (haemangioma, lymphangioma) and secondary (pseudocysts/nonepithelial), which are generally of post-traumatic origin [1,2]. Robbins et al., in an autopsy series of 42,327 autopsies conducted over 25 years reported only 32 cases of splenic cysts [3]. Elias and Evangelos recently reported three cases of splenic cysts; one lympangioma, one post-traumatic and one epidermoid cyst [4]. True cysts account for around 10% of non-parasitic cysts, but they are the most frequent type of splenic cysts in children [5]. In our case cyst was lined by stratified squamous epithelium revealing its true nature.
Secondary cysts (pseudocysts) are thought to result from splenic trauma (resolving haematoma), inflammation (post pancreatitis walled off necrosis), or vascular insult (cystic change post infarction) to the spleen. Burrig and Morgenstern questioned the existence of the post-traumatic pseudocysts. According to Burrig, the gross appearance of most of these cysts is the same whether or not an epithelial lining is demonstrated on histological sections. Many of the so-called pseudocysts, ascribed to antecedent trauma, reveal remnants of epithelial lining [6,7]. In our case there was no history of trauma which made the possibility of pseudocyst unlikely.
Epidermoid cysts are thought to arise from inclusion of splenic surface mesothelium into the splenic parenchyma during development. Mostly asymptomatic these cysts cause symptoms only if they acquire a size of 5cm or more by the second or third decade of life; though our patient became symptomatic in the first decade. Common symptoms are dull aching pain with left upper quadrant fullness. Epidermoid cysts have been reported by various authors in recent studies, arising in pregnant women and in intra-pancreatic accessory spleen especially in elderly [Table/Fig-4]. Complications include rupture with abdominal trauma, hypertension due to renal compression, infection, hypersplenism, haemorrhage within the cyst and even malignant degeneration [7]. In our patient abdominal tenderness was present along with pain. Pus was drained during operation which shows it was secondarily infected.
Recent studies from literature with varied presentation of epidermoid cyst of spleen, their clinical features and outcome.
| Author | Year of publication | Age of presentation | Clinical presentation | Remarkable feature | Outcome |
|---|
| Narita M [8] | 2016 | 75 year | Left upper quadrant pain for one month | Intrapancreatic accessory spleen cyst in pancreatic tail | Uneventful recovery posts laproscopic excision |
| Rana APS [9] | 2014 | 12 year | Dull pain and fullness in left upper abdomen for three years | 10.2 X 8.4 cm cyst with 600 ml turbid fluid in spleen | Uneventful recovery post splenectomy |
| Forouzesh M [10] | 2013 | 26 year | Left upper quadrant pain | Splenic epidermoid cyst detected at 15 weeks of gestation | Uneventful recovery post splenectomy |
| Horn JA [11] | 2011 | 62 year | Vague left abdominal pain | Cyst in Intra-pancreatic accessory spleen | Uneventful recovery post splenectomy |
| Sarvaiya A [12] | 2006 | 26 years | Intermittent dull pain in left hypochondrium for 2 years | 14x13 cm non contrast enhancing cyst | Uneventful recovery post splenectomy |
| Present case | 2016 | 5 years | Dull dragging epigastric and right hypochondriac pain since 15 days | Cystic lesion is seen measuring 12x10x10 cm and replacing upper and mid part of spleen | Uneventful recovery post splenectomy |
The differential diagnosis could be splenic lesions like lymphangioma, haemangioma, hydatid cyst, bacterial abscess, cystic metastasis and intrasplenic pancreatic pseudocyst. Radiological investigations like ultra-sonogram, CT scanning or MRI may help in identifying the morphology, composition of cystic fluid and their location in spleen but the final diagnosis depends on the histopathological examination of the cyst [13–15]. The epidermoid cyst exhibits unique gross features with a grey white, smooth and glistening wall having prominent trabeculations [7]. The cyst contains thin to viscid, colourless to brownish fluid. Histologically it is characterised by squamous epithelial lining or a single layer of flattened epithelium without skin appendages. Desquamation of epithelium may lead to loss of lining in some portions of wall. Flattened lining may be mistaken for the endothelium. Positivity for CK and negativity for factor 8 may help in differentiating between the two [16]. Calcifications of both the primary and secondary cysts are frequently found, which are useful in diagnosing cysts from other causes of splenomegaly [13].
The conventional treatment of splenic epidermoid cyst has been splenectomy. Alternative treatments include: aspiration and sclerotherapy, partial splenectomy, cyst decapsulation (unroofing) and laparoscopic partial cystectomy [17]. Small asymptomatic cysts less than 5cm are generally left untreated [7]. In our case the cyst was 10x8cm, symptomatic hence, it needed surgical intervention.
Conclusion
This case is reported because of the relative rarity of this type of cyst and because it presents such characteristic findings as young age group, the absence of acute symptoms except for the space occupying lesion in upper abdomen, its recent rapid growth and vague abdominal pain. Though splenic epidermoid cyst is an uncommon entity, it should be considered in the differential diagnosis of an abdominal mass in a young individual. Histopathology helps in the diagnosis and can help rule out the infectious and malignant differentials.
[1]. Reddy VR, Reddy MK, Srinivas B, Sekhar CC, Ramesh O, Mesothelial splenic cyst--a case reportAnn Acad Med Singapore 1998 27:880-82. [Google Scholar]
[2]. Verma M, Vashist MG, Dalal S, Chanchal Singla A, Epidermoid cyst of the spleenIJRRMS 2013 3:47-48. [Google Scholar]
[3]. Robbins FG, Yellin AE, Lingua RW, Crsig JR, Turrill FL, Mikkelsen WP, Splenic epidermoid cystsAnn Surg 1978 187:231-35. [Google Scholar]
[4]. Karfis EA, Roustanis E, Tsimoyiannis EC, Surgical Management of Nonparasitic Splenic CystsJSLS: Journal of the Society of Laparoendoscopic Surgeons 2009 13:207-12. [Google Scholar]
[5]. Ough YD, Nash HR, Wood DA, Mesothelial cysts of the spleen with squamous metaplasiaAm J Clin Pathol 1981 76:666-69. [Google Scholar]
[6]. Burrig KF, Epithelial (true) splenic cysts: pathogenesis of mesothelial and so-called epidermoid cyst of spleenAm J Surg Pathol 1988 12:275-81. [Google Scholar]
[7]. Morgenstern L, Nonparasitic Cysts: pathogenesis, classification, and treatmentJ Am Coll Surg 2002 194:306-14. [Google Scholar]
[8]. Narita M, Hanada K, Moriyoshi K, Matsusue R, Hata H, Yamaguchi T, Laparoscopic resection of an epidermoid cyst arising from intrapancreatic accessary spleenPancreas (Online) 2016 S(1):138-41. [Google Scholar]
[9]. Rana APS, Kaur S, Singh P, Malhotra S, Kuka AS, Splenic epidermoid cyst - a rare entityJ Clin Diagn Res 2014 8:175-76. [Google Scholar]
[10]. Forouzesh M, Ghanbarzadegan L, Rahimi M, Ghahramani L, Splenic epidermoid cyst during pregnancy; case report and review of the literatureBull Emerg Trauma 2013 1:179-81. [Google Scholar]
[11]. Horn AJ, Lele SM, Epidermoid cyst occurring within an intrapancreatic accessory spleen. a case report and review of the literatureJ Pancreas (Online) 2011 12:279-82. [Google Scholar]
[12]. Sarvaiya A, Raniga S, Vohra P, Sharma A, Bhrtyan Case report: Huge splenic epidermoid cystIndian J Radiol Imaging 2006 16:197-98. [Google Scholar]
[13]. Hansen MB, Moller AC, Splenic cystsSurg Laparosc Endosc percutan Tech 2004 14:316-22. [Google Scholar]
[14]. Robertson F, Leander P, Ekberg O, Radiology of the spleenEur Radiol 2001 11:80-95. [Google Scholar]
[15]. Labruzzo C, Haritopoulos KN, EL Tayar AR, Hakim NS, Posttraumatic cyst of the spleen: a case report and review of the literatureInt Surg 2002 87:152-56. [Google Scholar]
[16]. Vijay Shankar S, Usha R, Epidermoid cyst of spleenOnline J Health Allied Scs 2010 9:13 [Google Scholar]
[17]. Till H, Schaarschmidt K, Partial laparoscopic decapsulation of congenital splenic cysts. A medium-term evaluation proves the efficiency in childrenSurg Endosc 2004 18:626-28. [Google Scholar]