Wuchereria bancrofti: Unusual Presentation as Pancytopenia
Mili Jain1, Ayush Shukla2, Ashutosh Kumar3, Rashmi Kushwaha4, Uma Shankar Singh5
1 Assistant Professor, Department of Pathology, King George’s Medical University, Lucknow, UP, India.
2 Senior Resident, Department of Clinical Hematology, King George’s Medical University, Lucknow, UP, India.
3 Professor, Department of Pathology, King George’s Medical University, Lucknow, UP, India.
4 Associate Professor, Department of Pathology, King George’s Medical University, Lucknow, UP, India.
5 Professor, Department of Pathology, King George’s Medical University, Lucknow, UP, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mili Jain, Assistant Professor, Department of Pathology, King George’s Medical University, Lucknow, UP-226003, India.
E-mail: milijain786@gmail.com
Wuchereria bancrofti is an endemic filarial nematode spread by a mosquito vector. The clinical manifestations vary from asymptomatic microfilaremeia to lymhoedema. We report two cases of microfilaria of Wuchereria bancrofti in bone marrow presenting as peripheral pancytopenia. The patient did not have any classical features of lymphoedema or elephantiasis. The diagnostic demonstration of microfilaria with unusual presentations has been done in cytology specimens from various sites. Microfilaria infection in association with peripheral blood pancytopenia has been rarely reported. An aetiopathological co-relation of these haematological manifestations of microfilaria needs further investigation.
Bone marrow parasite, Maturation arrest, Microfilariae
Case Report
Case 1
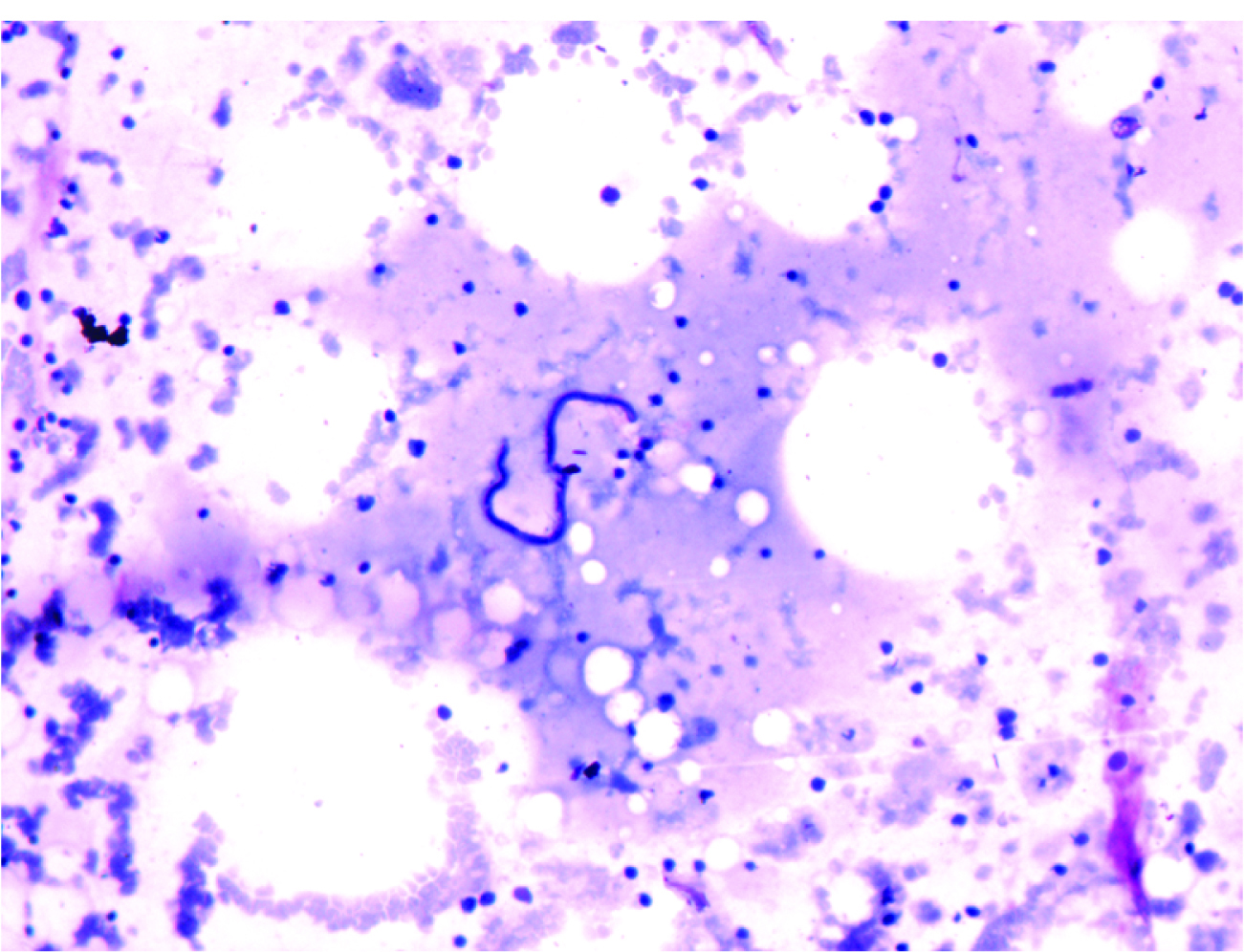
A 14-year-old male presented with generalised weakness, high grade fever and progressive pallor for 1 month. On examination he had pallor and fever. There was no lymphadenopathy or organomegaly. On routine haemogram he had pancytopenia, haemoglobin (Hb) 7 gm%, Total Leukocyte Count (TLC) was 3700/ul and platelet count was 45000/ul. Differential Leucocyte count revealed 85% lymphocytes. No immature cells were seen. Serum biochemical parameters including serum bilirubin, liver enzymes, glucose, vitamin B12, folic acid and creatinine were within normal range. Viral serology was negative. These findings provisionally ruled out megaloblastic anaemia and viral infection. A provisional diagnosis of bone marrow failure was made and bone marrow aspiration and biopsy was done for further evaluation to rule out any hematopoietic neoplasm. Bone marrow smears revealed markedly hypo-cellular particles rich in fat. All hematopoietic elements were markedly reduced, with predominant population of lymphocytes (72%) and plasma cells (6%). In addition, the Leishmann stained bonemarrow smear also revealed few sheathed microfilariae of Wuchereria bancrofti with tail end free from nuclei [Table/Fig-1]. The patient was started on DEC along with cyclosporine and supporting transfusions. At 6 month follow-up patient had recovered peripheral blood counts.
Leishmann stained Hypocellular marrow smears with microfilaria (100 X).
Case 2
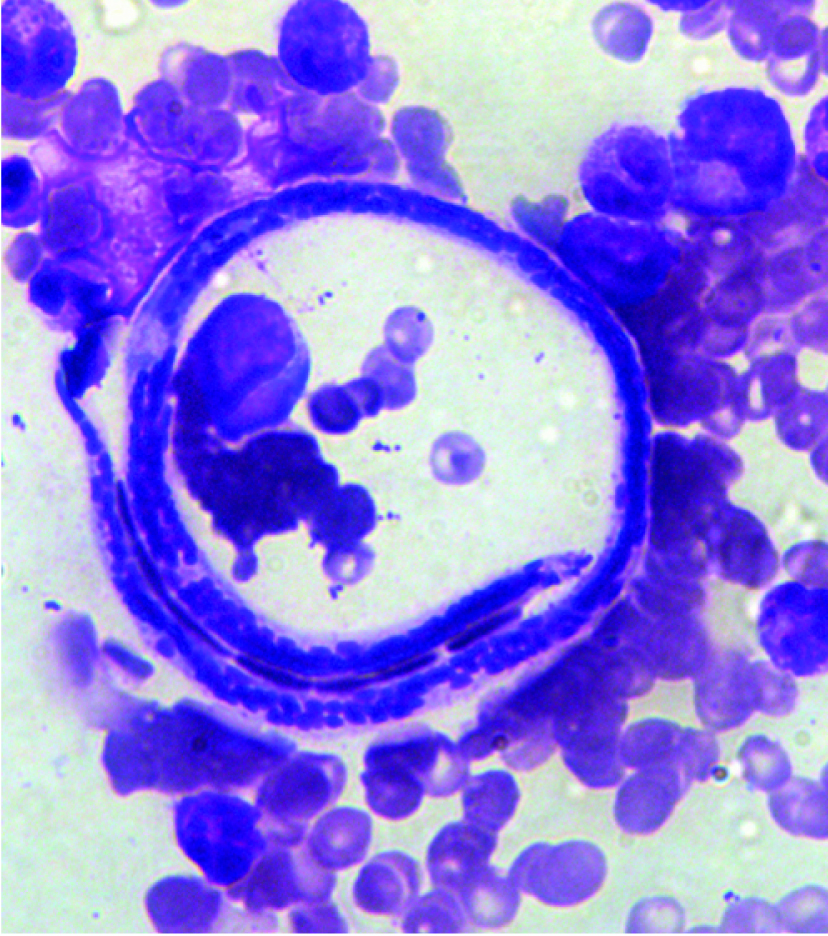
A 35-year-old female presented with petechial rashes, fever and mennorhagia for 2 months. Her examination was unremarkable except for presence of pallor and petechial haemorrhages over extremities. Her TLC was 2100/μL with 90% mature lymphocytes, reduced platelet count of 9000/μL and Hb of 6gm%. The bone marrow was hyper cellular with predominance of granulocytic precursors (82%) with maturation arrest. Megakaryocytes were adequate however had reduced thrombopoietic activity. Erythroid precursors had normoblastic maturartion. Dispersed throughout the leishmann stained bone marrow smear were few sheathed microfilariae of W Bancrofti with tail end free from nuclei [Table/Fig-2]. The patient left and no follow-up could be obtained.
Leishmann stained marrow smears with myeloid left shift cells and microfilaria of Wuchereria bancrofti (400X).
Discussion
The filarial infection of W bancrofti results in a wide spectrum of clinical presentations ranging from asymptomatic microfilaremia to one with chronic manifestations including lymphoedema and elephantiasis. The diagnostic demonstration of microfilaria with unusual presentations has been done in cytology specimens from various sites [1–3]. Microfilaria infection in association with peripheral blood pancytopenia has been rarely reported.
The peak age for filarial infection is 15 to 20 years. In natural life cycle of W bancrofti, the adult worm lodges in the lymphatics and microfilaria circulate in the blood. During their circulation, the microfilaria gets lodged in various tissue sites. They may rarely be trapped in the bone marrow. Such cases, though very few in number, have been reported previously [Table/Fig-3] [4–12]. The present cases did not have a classical presentation of lymphatic filariasis, similar to the previous reports [4–9]. Peripheral blood eosinophilia, a common finding in filariasis was not seen in our cases as well as in majority of previous reports [4,6,8]. Shenoi et al., described 2 cases of bone marrow aspirate showing incidental finding of microfilaria. One case had aplastic anaemia and other had megakaryocytic aplasia [8]. Similarily Hemchandran et al., in 2003 reported a single case with aplastic anaemia and co-existing infection with varicella and Wuchereria bancrofti [5]. Sharma et al., reported 6 cases of bone marrow aspirate positive for Wuchereria bancrofti. Five of the six cases had marrow hypoplasia [4]. Tejwani et al., reported a patient with marrow failure and incidental finding of microfilaria of Wuchereria bancrofti [10]. The present cases also point to this rare association of pancytopenia with microfilariasis. Majority of the reported cases report hypoplasia in the marrow, however the second case here had hypercellular marrow with maturation arrest. The aetio-pathological significance of microfilaria in these cases needs to be worked further. The drug of choice for treatment of bancroftian filariasis is Diethylcarbamazine (DEC) which is effective in killing microfilariae. The effect on adult worm is uncertain. The dose of DEC for treatment of filaria is 6mg/kg body weight per day orally for 12 days given preferably in divided doses after meals. In addition the patients with pancytopenia need transfusion support and haematinics.
Summary of clinical and hematological features in previous reports.
| Study | No. of cases | Organo-megaly | PBS finding | Eosinophilia | BM |
|---|
| Sharma et al., [4] | 6 | Absent | Pancytopenia (5/6) | Absent | Hypoplastic (5/6) with microfilariae |
| Hemchandran et al., [5] | 1 | Absent | Pancytopenia | Absent | Aplastic with microfilariae |
| Pradhan S et al., [6] | 1 | Absent | Anaemia | Absent | Microfilariae |
| Molina MA et al., [7] | 1 | Absent | HIV positive | Present | Hypocellular with microfilariae of Mansonella |
| Shenoi U et al., [8] | 2 | 1/2 | Pancytopenia (1/2) | Absent | Aplastic (1/2) Megakaryocytic aplasia (1/2) |
| Arundhati et al., [9] | 1 | Present | Lymphoid blasts | Absent | Acute lymphoblastic leukemia with microfilariae |
| Tejwani et al., [10] | 1 | Absent | Pancytopenia | Absent | Aplasia with microfilarae |
| Zafar U et al., [11] | 1 | Absent | Normal | Absent | Metastatic epithelial malignancy with microfilariae |
| Uma Shankar T et al., [12] | 1 | Absent | Pancytopenia with microfilariae | Absent | Megaloblastic changes with microfilariae |
| Present report | 2 | Absent | Pancytopenia | Absent | Aplasia with microfilariae (1/2) Myeloid maturation arrest with microfilariae (1/2) |
Conclusion
It is important to screen, with high suspicion, the marrow smears of pancytopenic patients for parasites. A possible aetiological role of filariasis in bone marrow hypoplasia or maturation arrest needs further investigation.
[1]. Yenkeshwar PN, Kumbhalkar DT, Bobhate SK, Microfilariae in fine needle aspirates: a report of 22 casesIndian J Pathol Microbiol 2006 49:365-69. [Google Scholar]
[2]. Khare P, Kala P, Jha A, Chauhan N, Chand P, Incidental diagnosis of filariasis in superficial location by FNAC: A retrospective study of 10 yearsJ Clin Diagn Res 2014 8(12):FC05-08. [Google Scholar]
[3]. Gupta S, Gupta R, Bansal B, Singh S, Gupta K, Kudesia M, The significance of the incidental detection of filariasis on aspiration smears: a case seriesDiagn Cytopathol 2010 38:517-20. [Google Scholar]
[4]. Sharma S, Rawat A, Chowhan A, Microfilariae in bone marrow aspiration smears; their correlation with marrow hypoplasia: a report of six casesIndian J Pathol Microbiol 2006 49:566-68. [Google Scholar]
[5]. Hemachandran M, Varma N, Varma S, Aplastic anaemia following a varicella infection with a co-existent microfilaraemia of Wuchereria bancrofti- a case reportIndian J PatholMicrobiol 2003 46:662-63. [Google Scholar]
[6]. Pradhan S, Lahiri VL, Elhence BR, Singh KN, The microfilariae of Wuchereria bancrofti in bone marrow smearsAm J Trop Med Hyg 1976 25:199-200. [Google Scholar]
[7]. Molina MA, Cabezas MT, Giménez MJ, Mansonella perstans filariasis in an HIV patient: a finding in the bone marrowHaematologica 1999 84:861 [Google Scholar]
[8]. Shenoi U, Pai RR, Pai U, Nandi GK, Adhikari P, Microfilariae in bone marrow aspiration smearsActa Cytol 1998 42:815-16. [Google Scholar]
[9]. Arundhati, Kumar A, Kumar R, Acute lymphoblastic leukaemia with microfilaria: a rare coincidence in bone marrow aspiratesIndian J HematolBlood Transfus 2011 27:111-12. [Google Scholar]
[10]. Tejwani N, Tyagi S, Dass J, Aplastic anaemia with microfilaria in marrow aspirateMediterr J Hematol Infect Dis 2012 4(1) [Google Scholar]
[11]. Zafar U, Rahman K, Sherwani RK, Shahid M, Microfilariae of Wucheria bancrofti in bone marrowIndian J Hematol Blood Transfus 2009 25(1):42-43. [Google Scholar]
[12]. Umashankar T, Yarnal PJ, Microfilariae in bone marrow aspirate: report of a caseJ Clin Diagn Res 2012 6(7):1294-95. [Google Scholar]